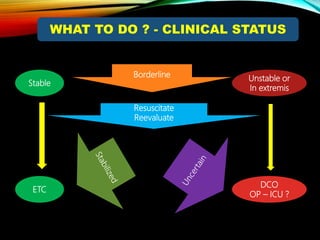
Control Orthopedics (DCO) provides guidelines for treating orthopedic injuries in polytrauma patients. It recognizes that definitive surgical stabilization can worsen a physiologically compromised patient's condition. DCO aims to 1) control hemorrhage and provisionally stabilize fractures, 2) avoid further physiological insult through delayed definitive repair, and 3) get the patient's condition optimized before further surgery. For unstable patients, DCO relies on external fixation and temporary stabilization rather than immediate internal fixation to minimize surgical impact. The approach balances fracture management with the overall goal of stabilizing the patient's physiology.