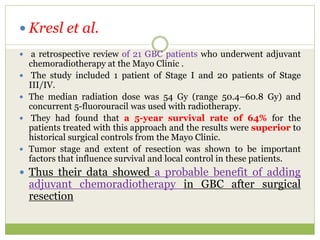
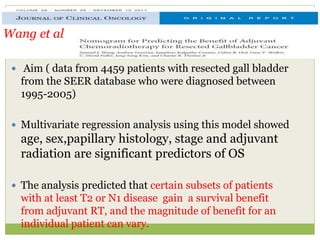
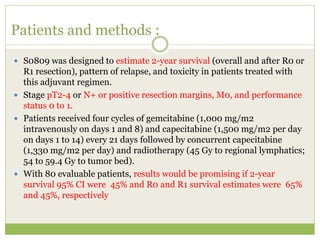
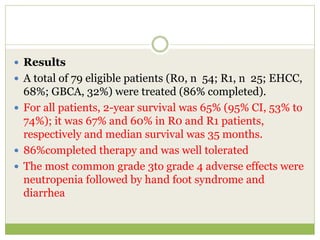
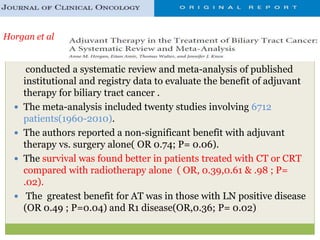
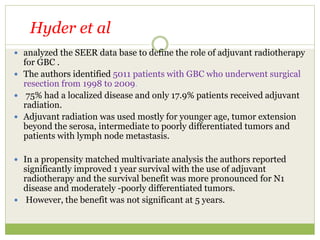
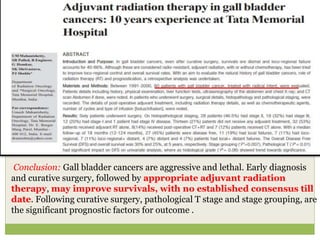
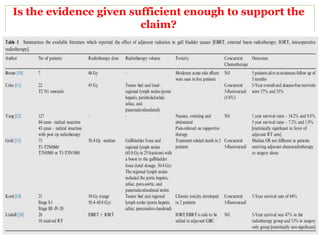
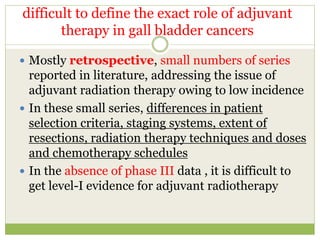
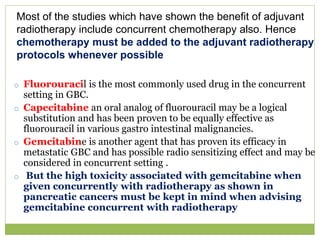
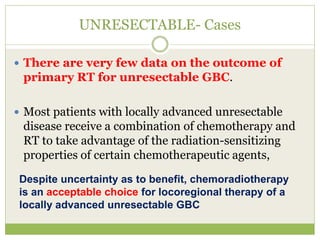
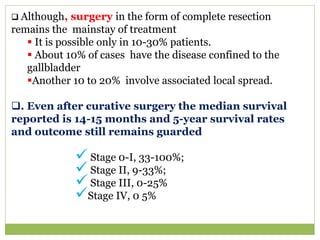
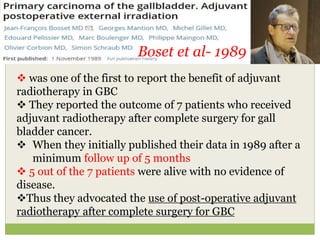
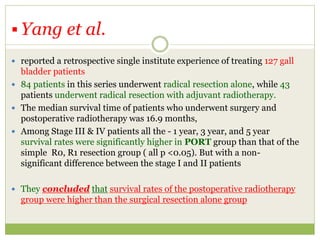
The document discusses adjuvant radiation therapy for gallbladder carcinoma based on available literature. It summarizes several retrospective studies that found improved survival outcomes with adjuvant radiation or chemoradiation after surgical resection compared to surgery alone, especially for node-positive or advanced-stage disease. However, it notes the evidence is limited due to the rarity of the disease and lack of large randomized controlled trials. While adjuvant therapy appears logical, more research is still needed to better define its role and optimal use.
![Zhonghua zhong liu za zhi [Chinese journal of oncology] 2013; 35: 534-539](https://image.slidesharecdn.com/gb-180331175841/85/ADJUVANT-RADIATION-IN-CA-GALLBLADDER-7-320.jpg)