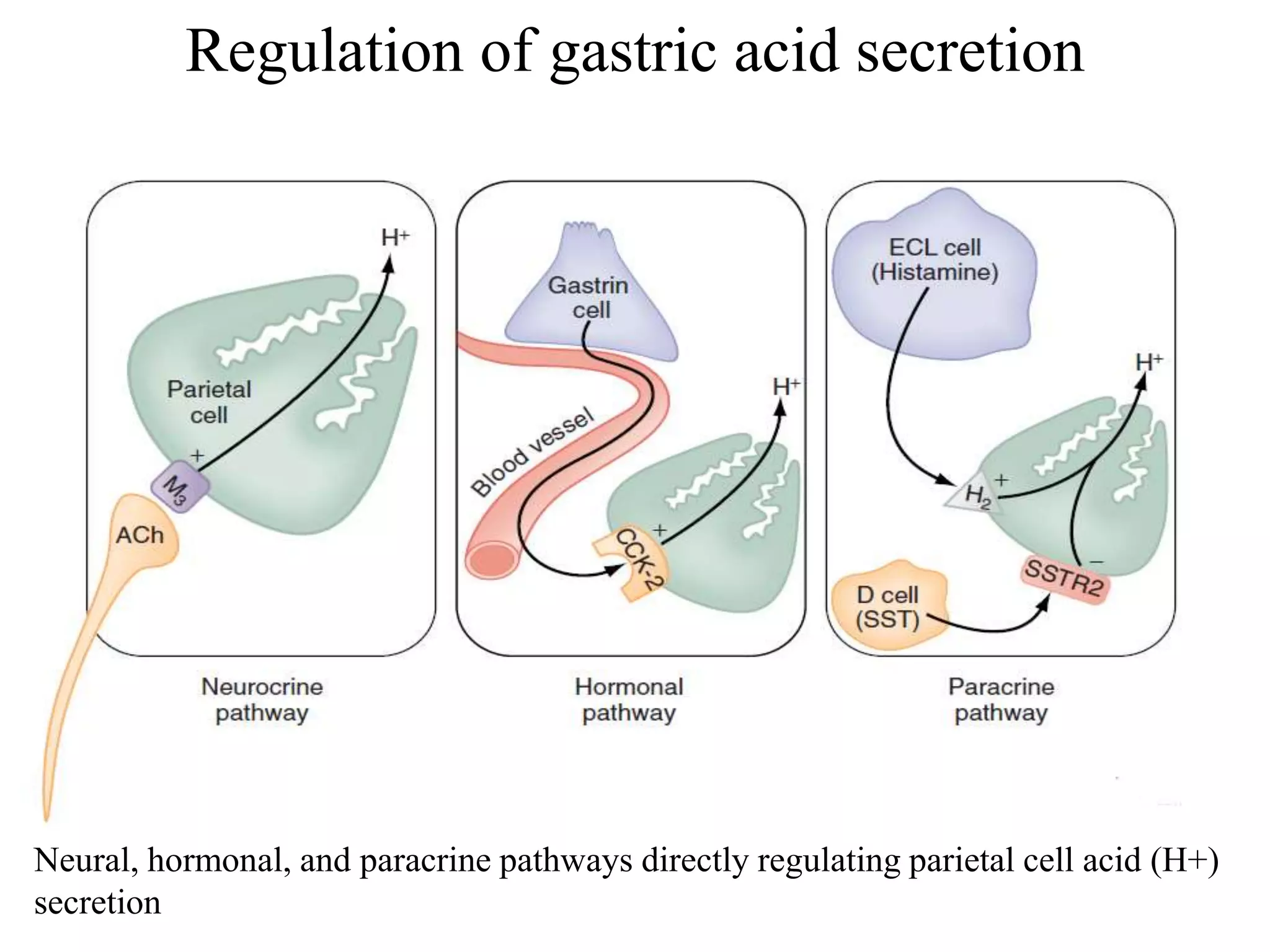
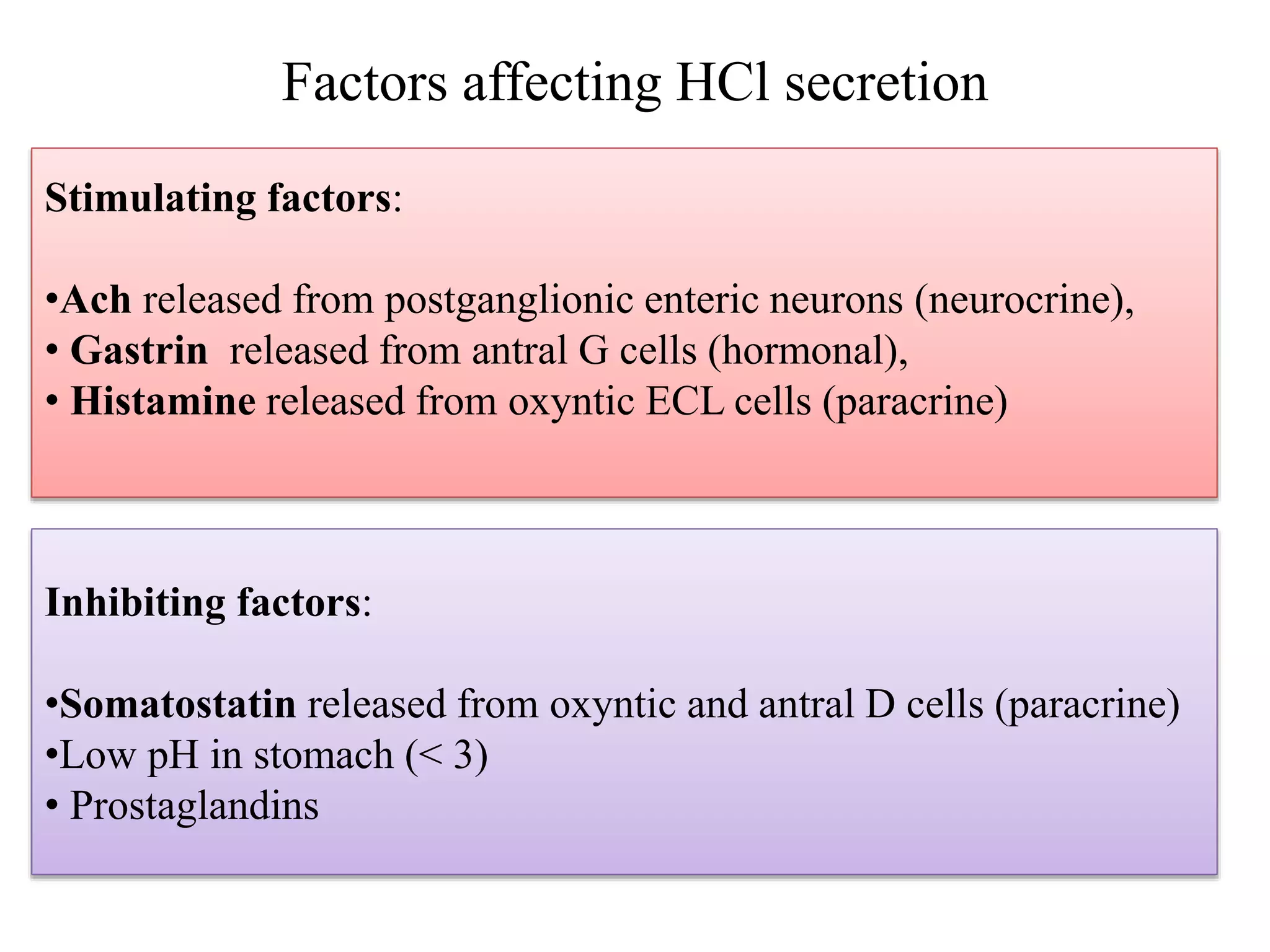
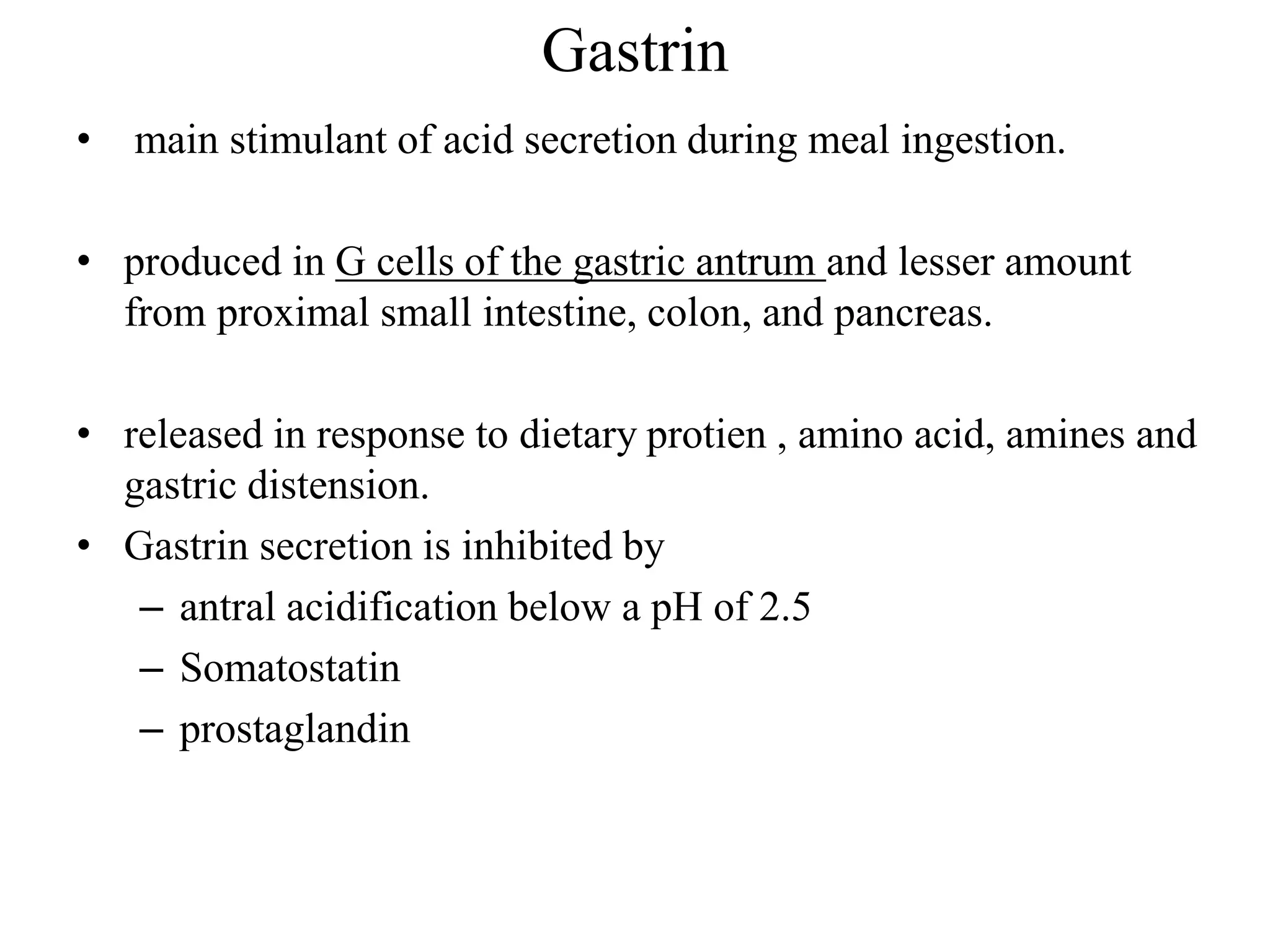
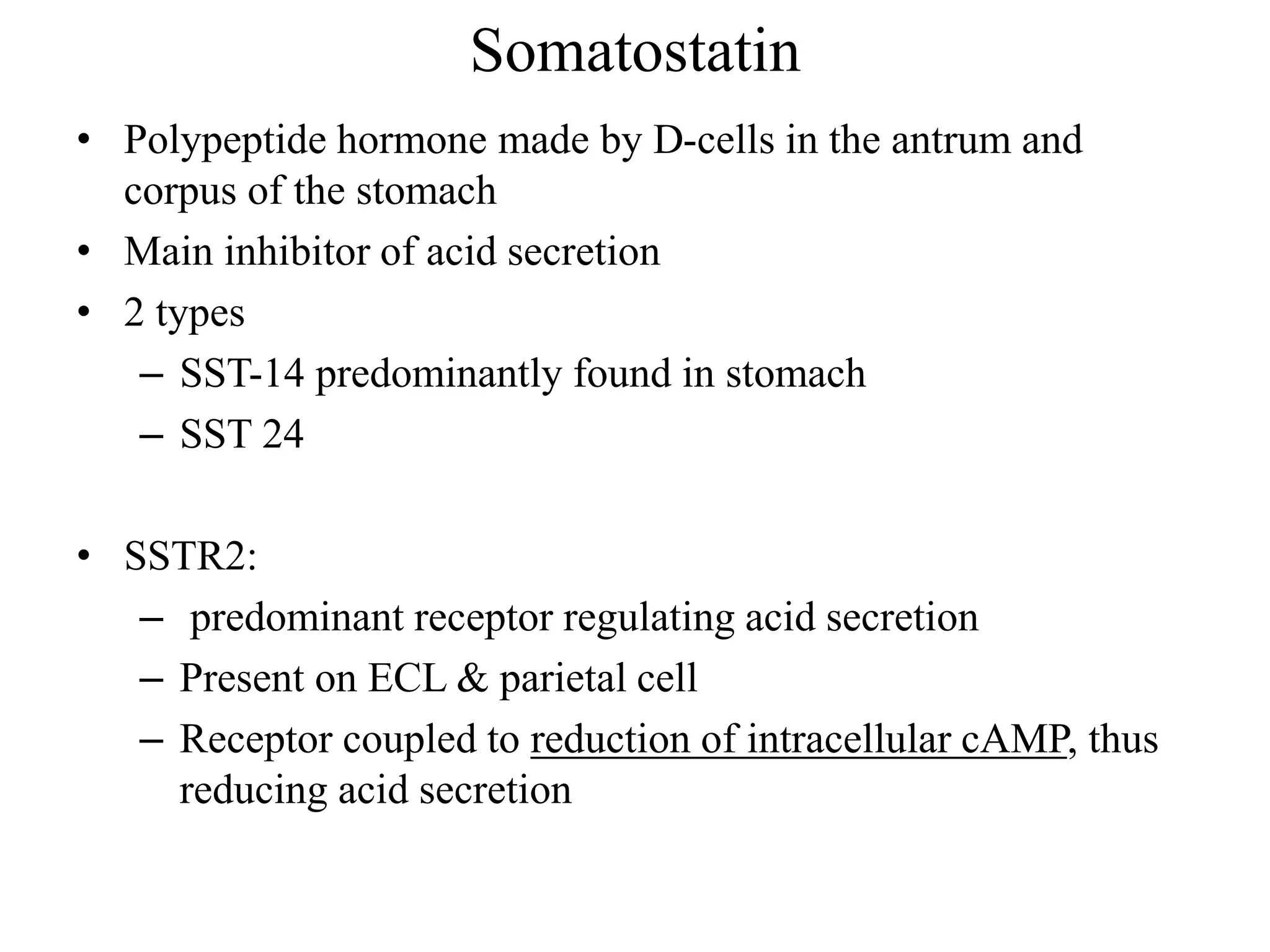
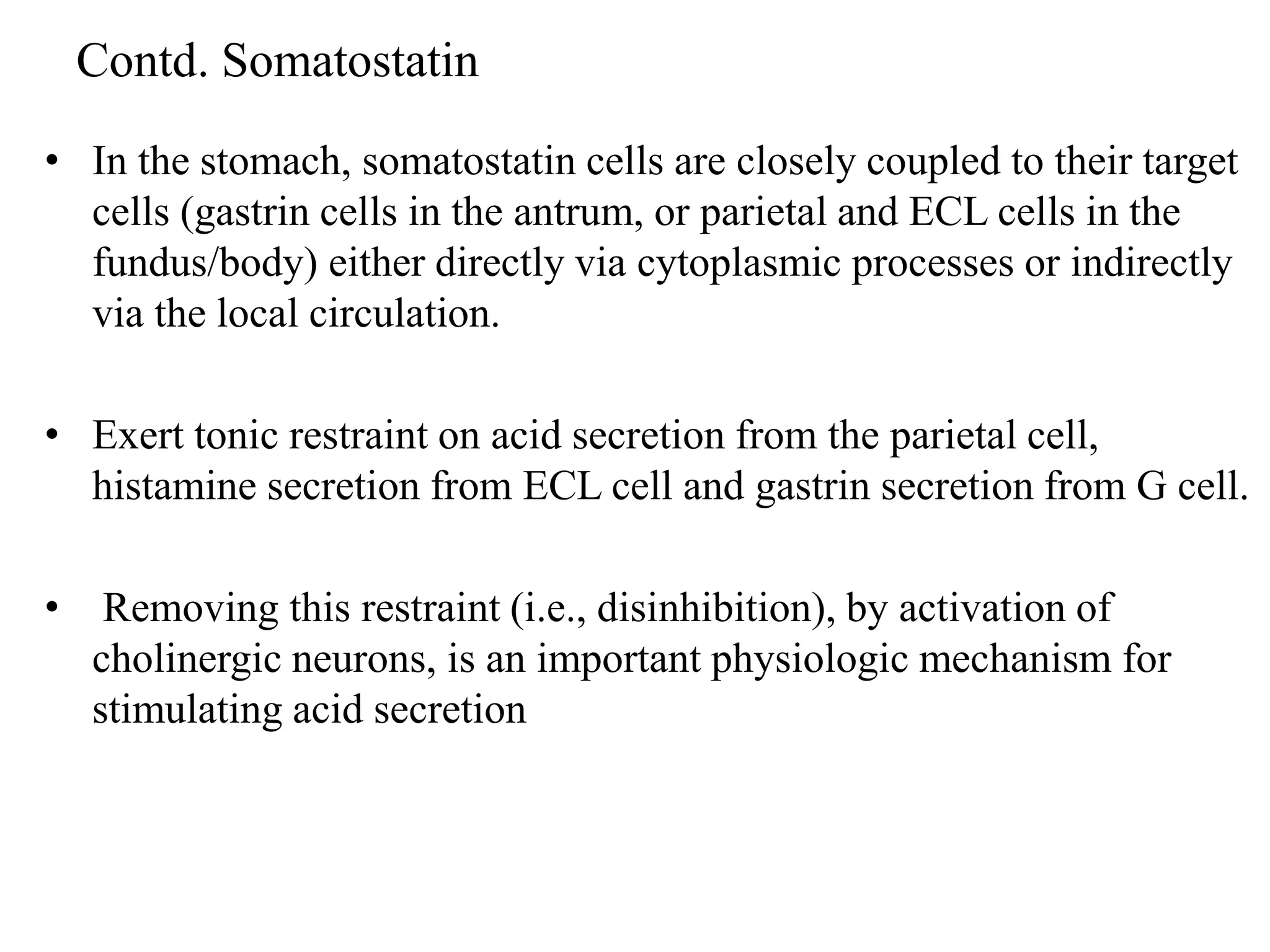
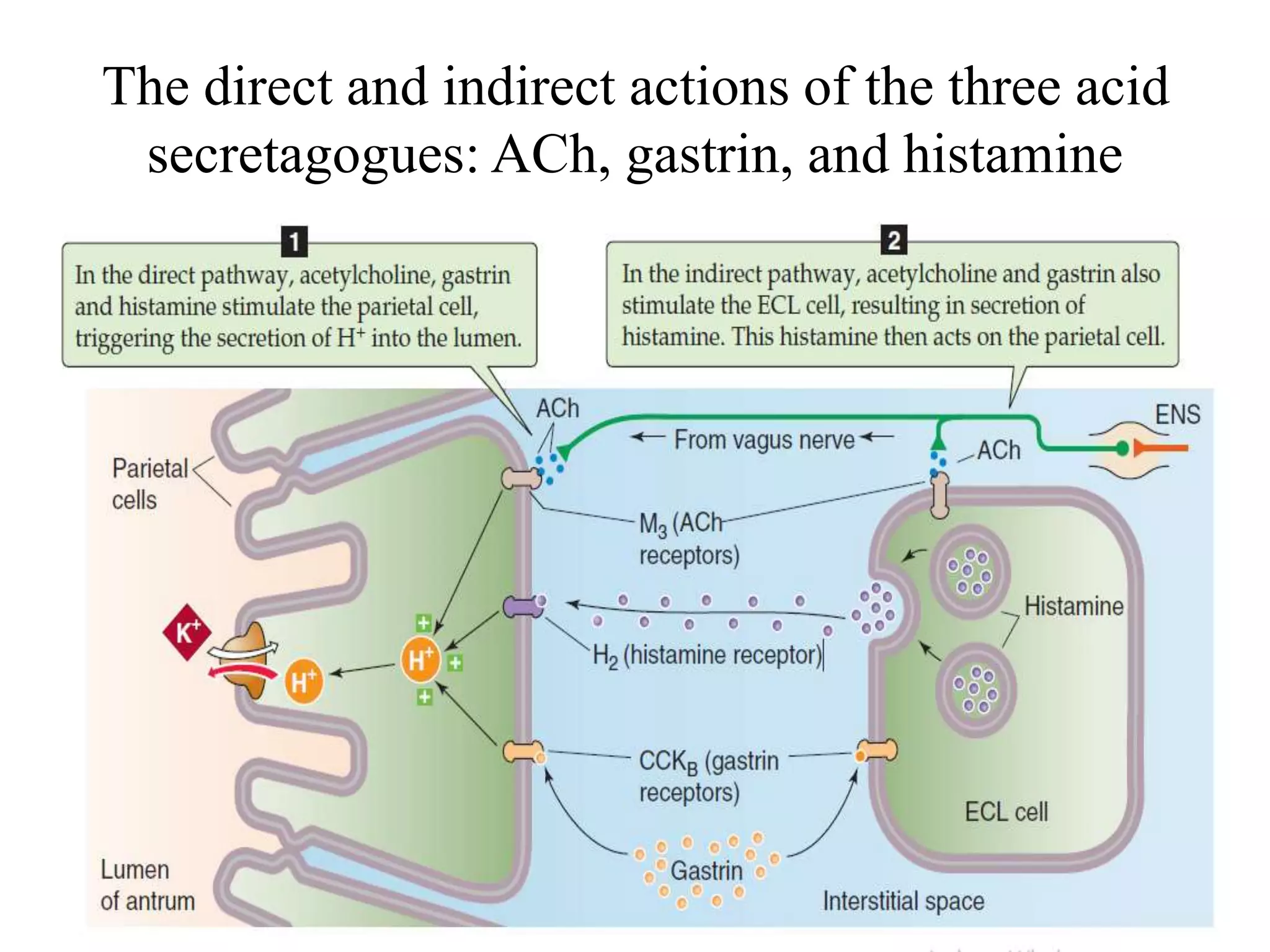
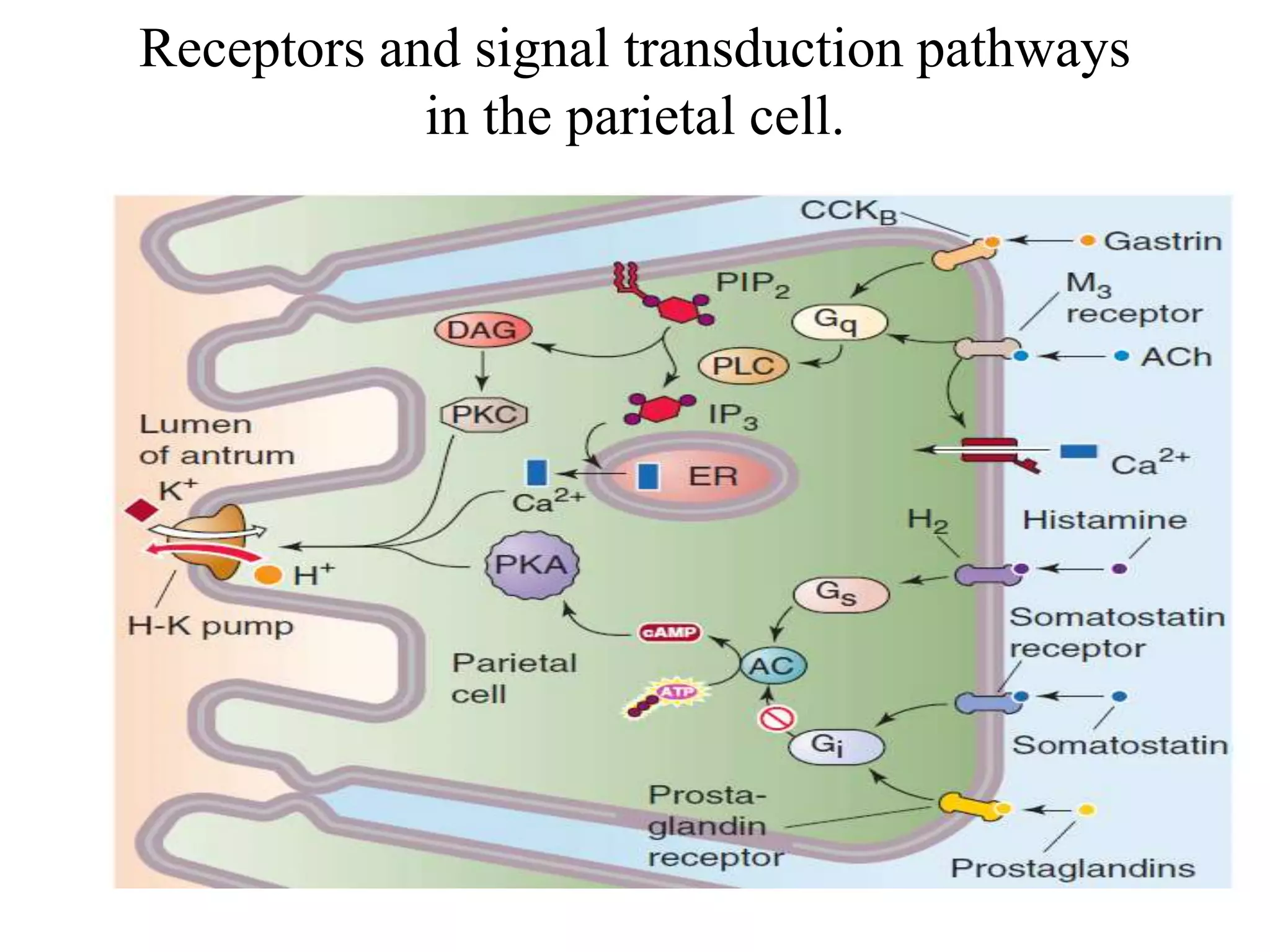
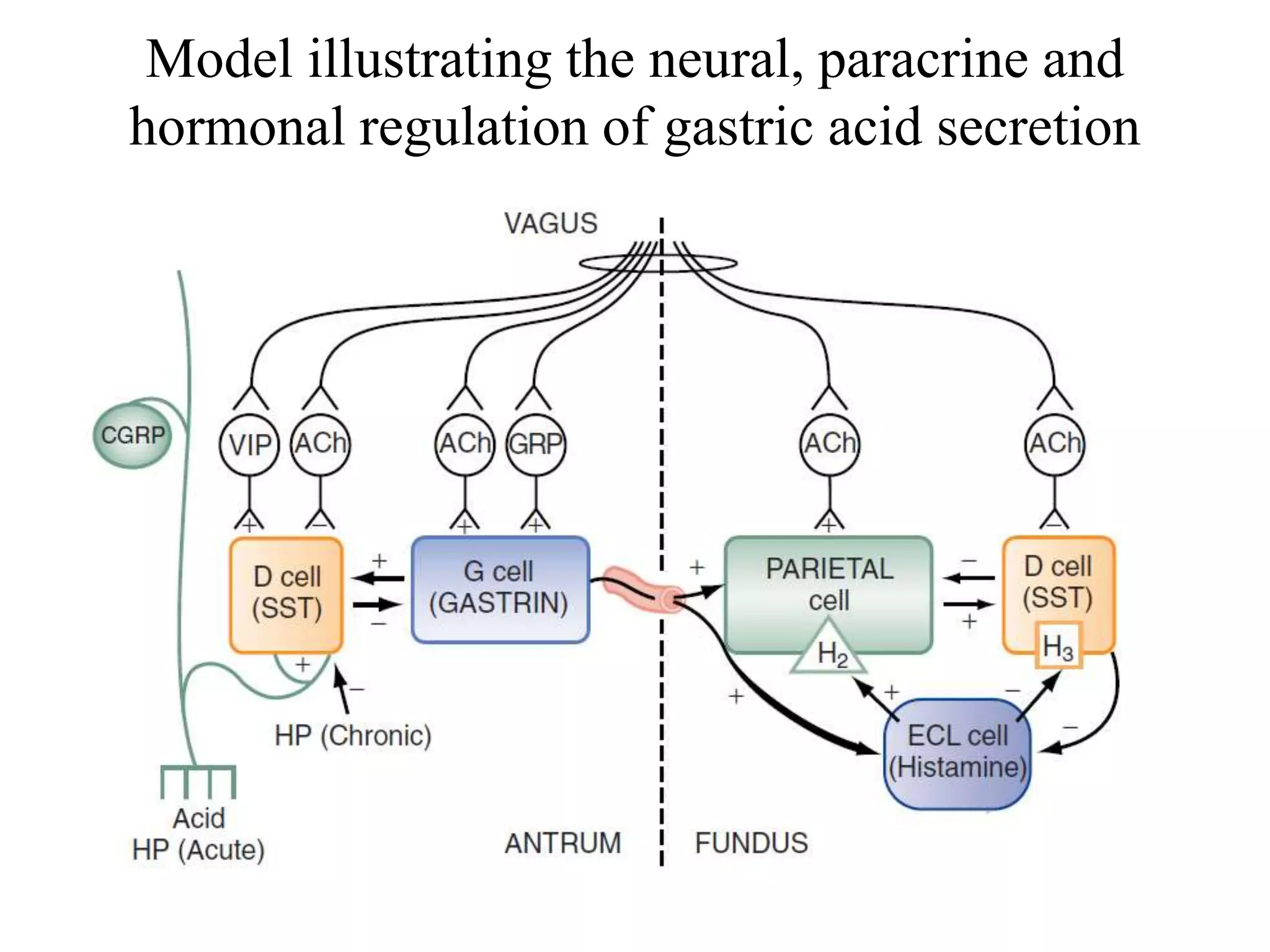
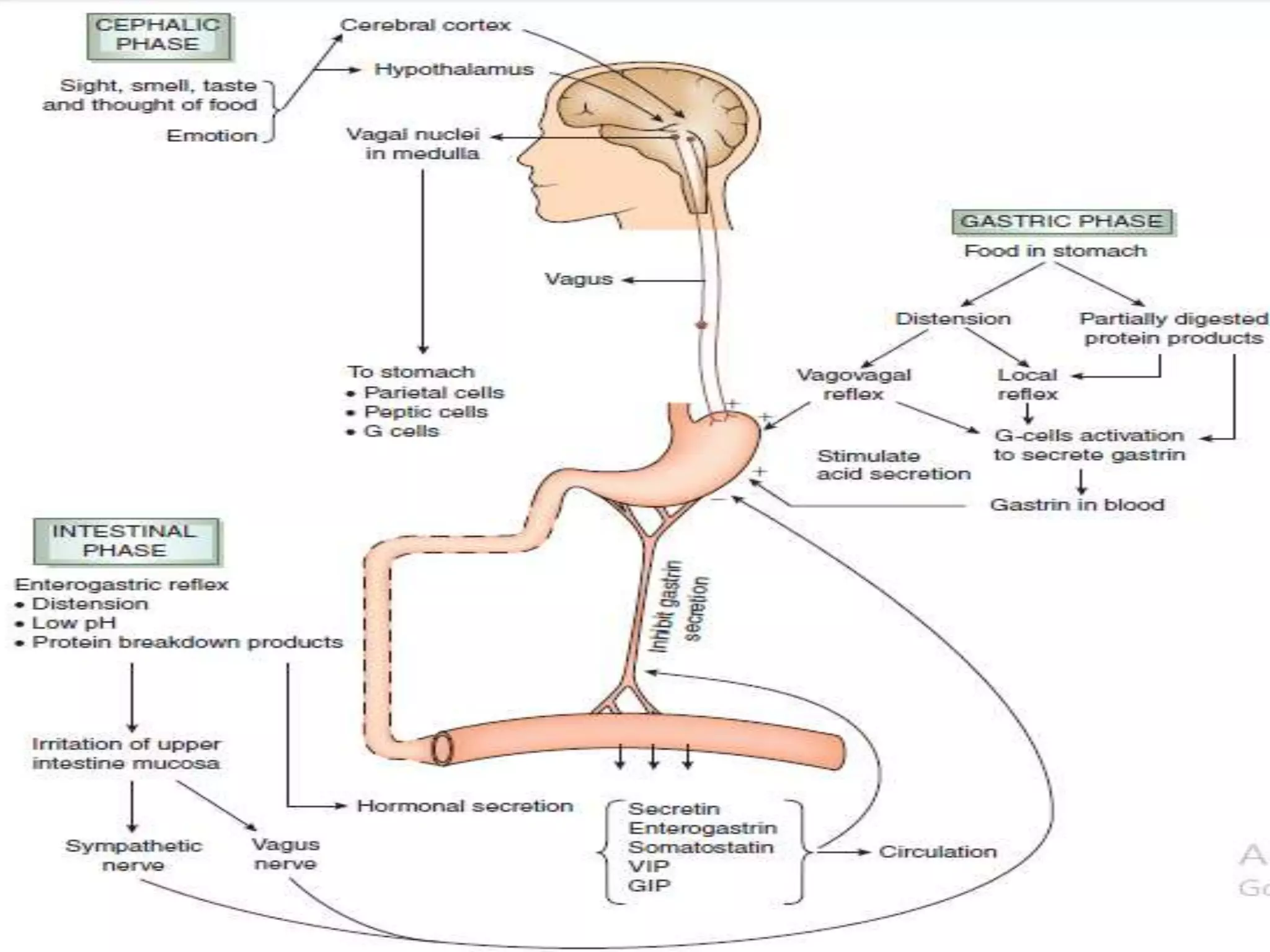
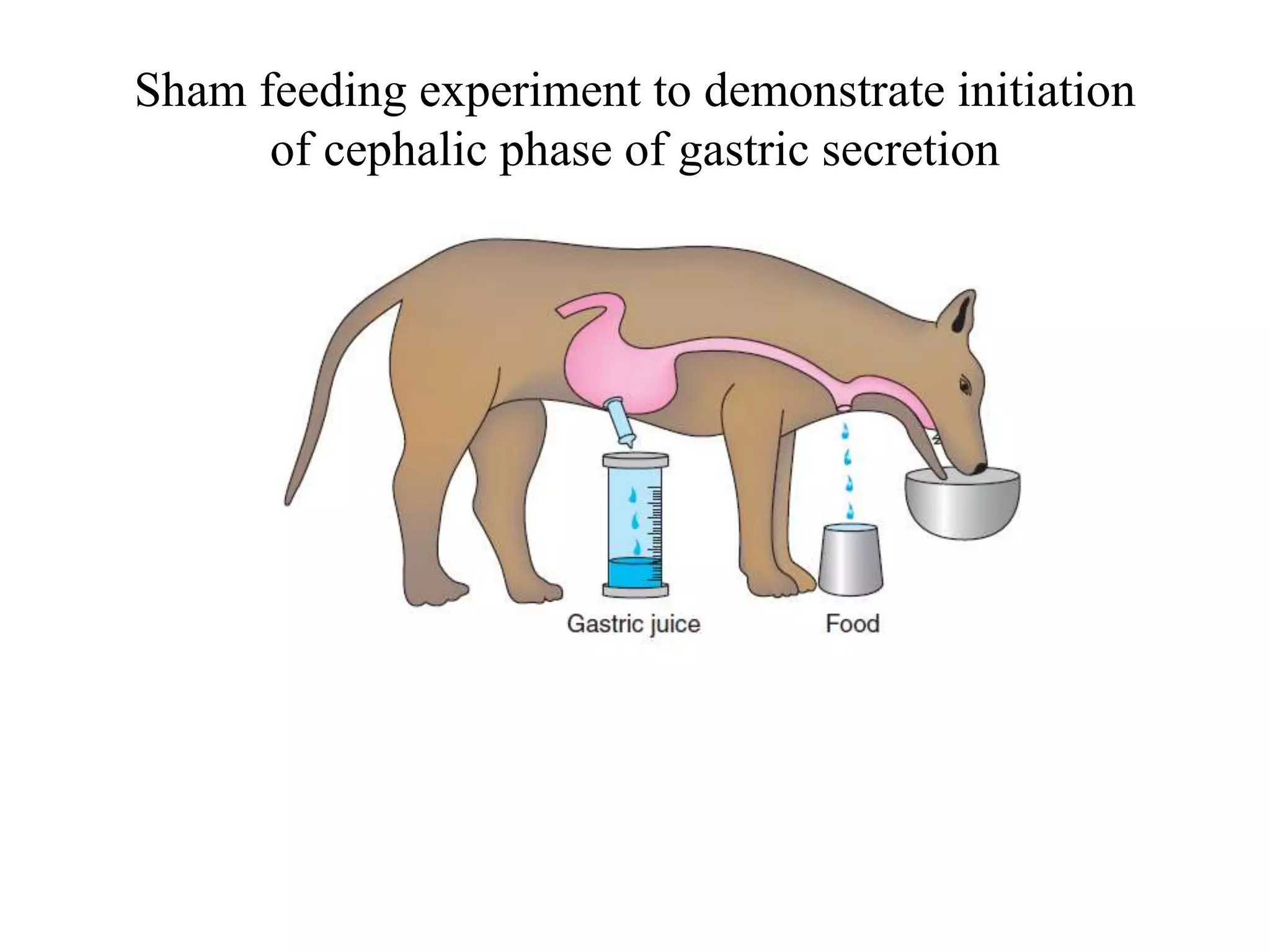
Gastric secretion is regulated by neural, hormonal, and paracrine pathways. The three major stimulants of acid secretion are gastrin from G-cells, acetylcholine as a neuromediator, and histamine from ECL cells. Somatostatin from D-cells is the main inhibitor. Parietal cells secrete hydrochloric acid and intrinsic factor, chief cells secrete pepsinogen, and surface mucous cells secrete mucus and bicarbonate to protect the gastric mucosa.