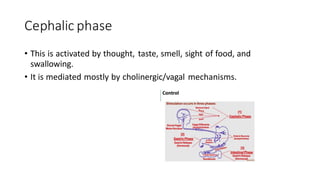
The stomach contains oxyntic glands that secrete hydrochloric acid via parietal cells. Parietal cells are stimulated by gastrin, histamine, acetylcholine, and ghrelin to secrete acid, which is precisely regulated. Gastrin and histamine are the major stimulants, released from G and enterochromaffin-like cells, respectively. Somatostatin from D cells is the main inhibitor by blocking gastrin and histamine. Acid secretion occurs in cephalic, gastric, and intestinal phases in response to food.