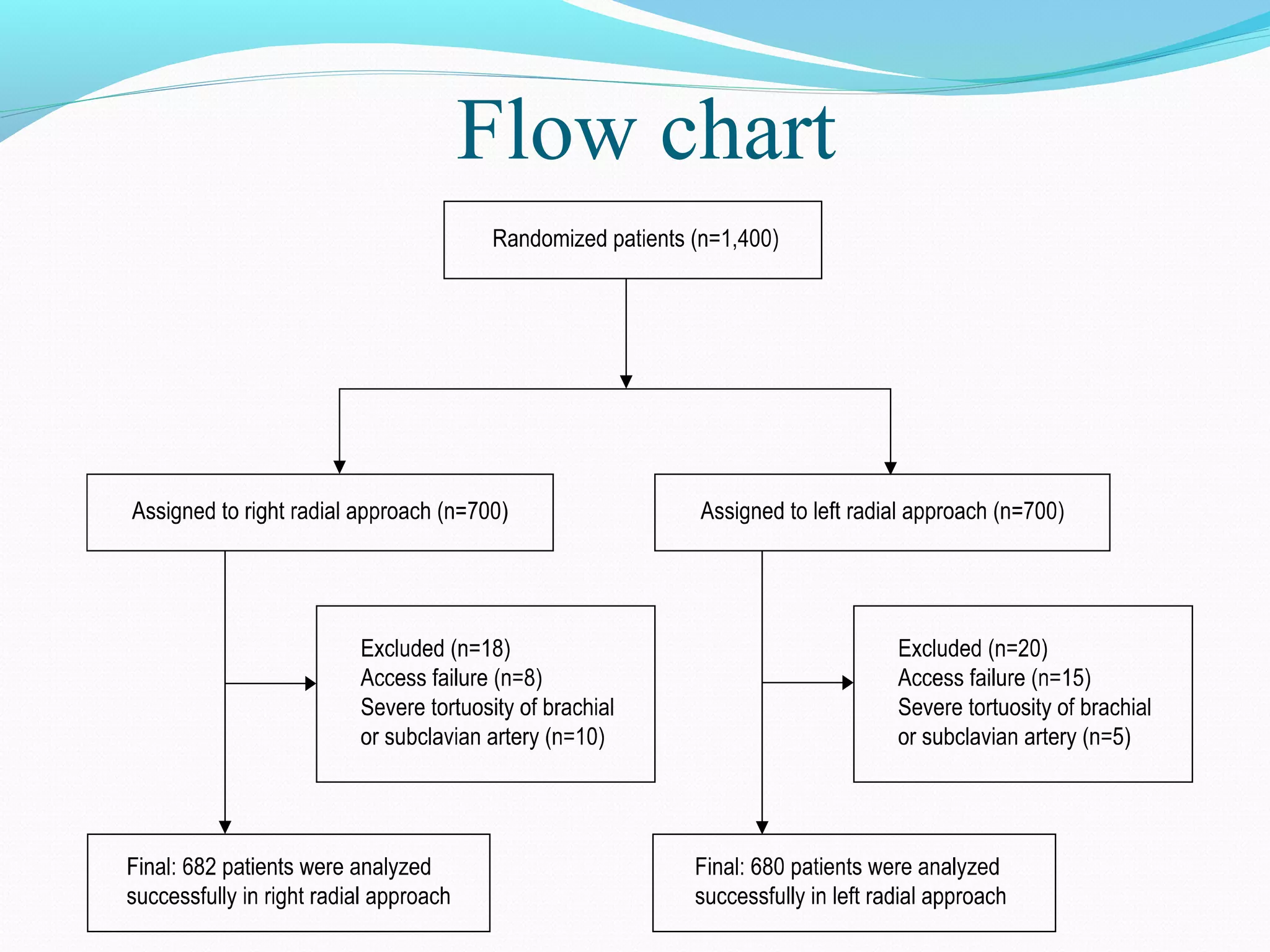
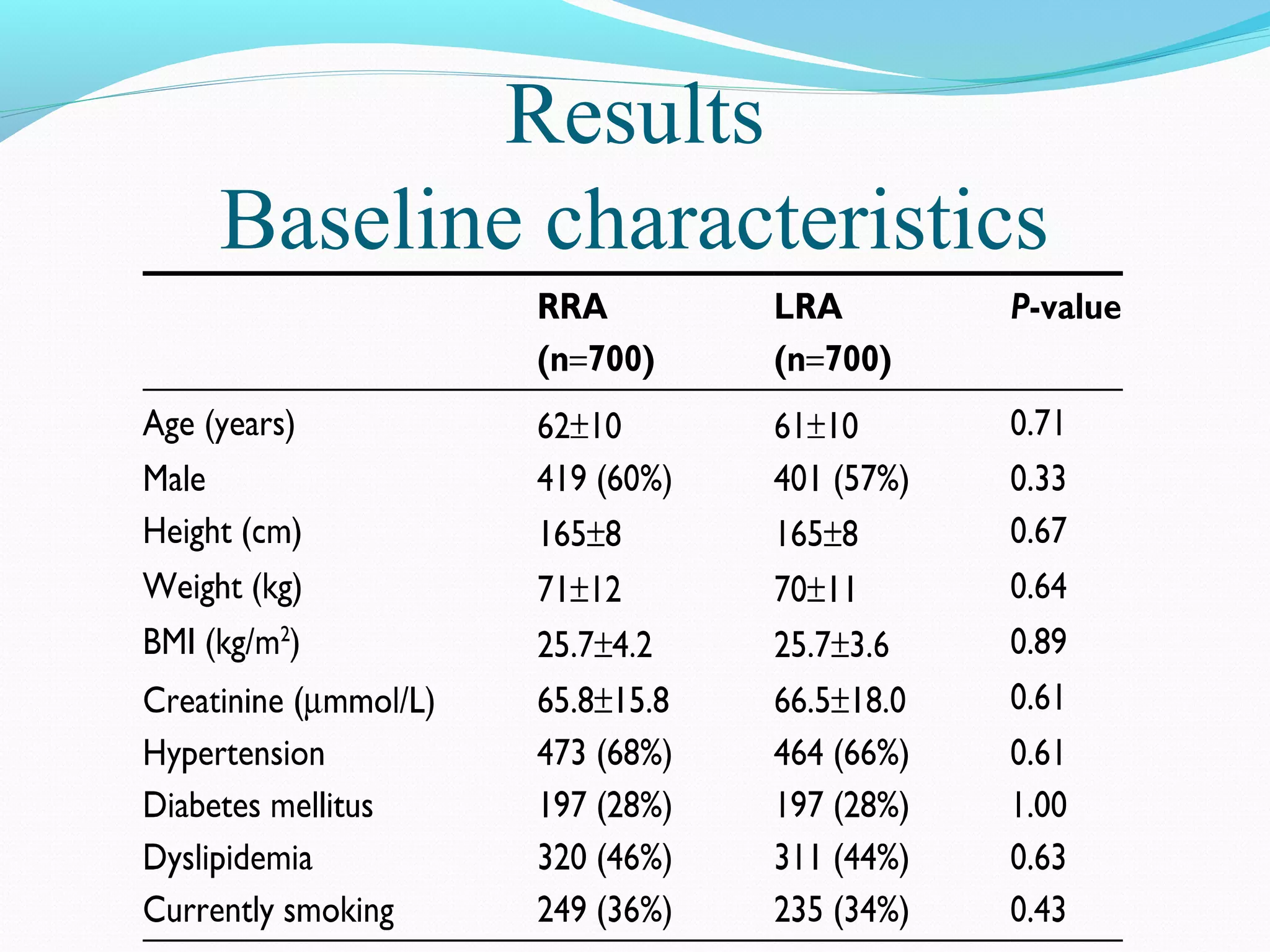
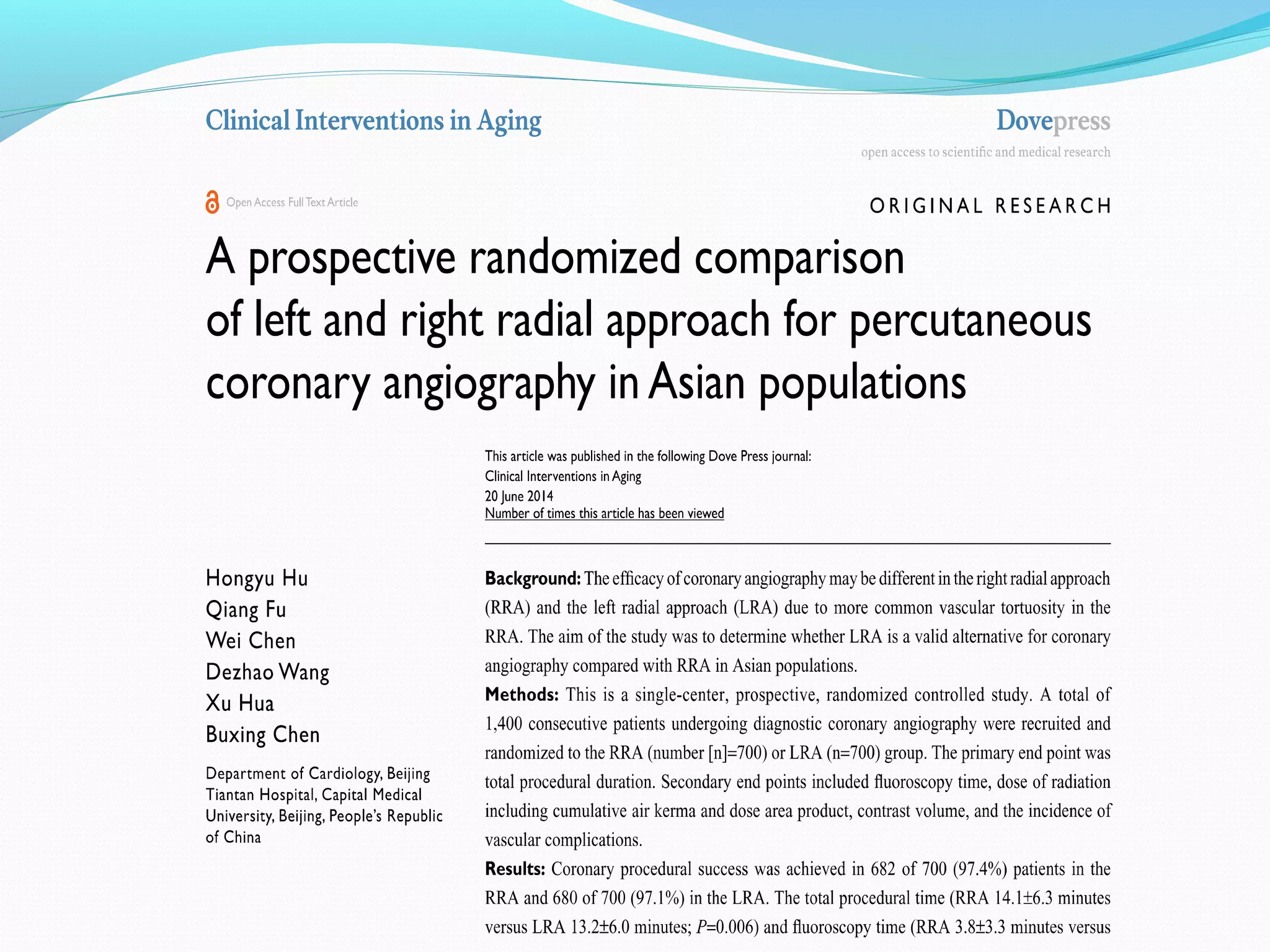
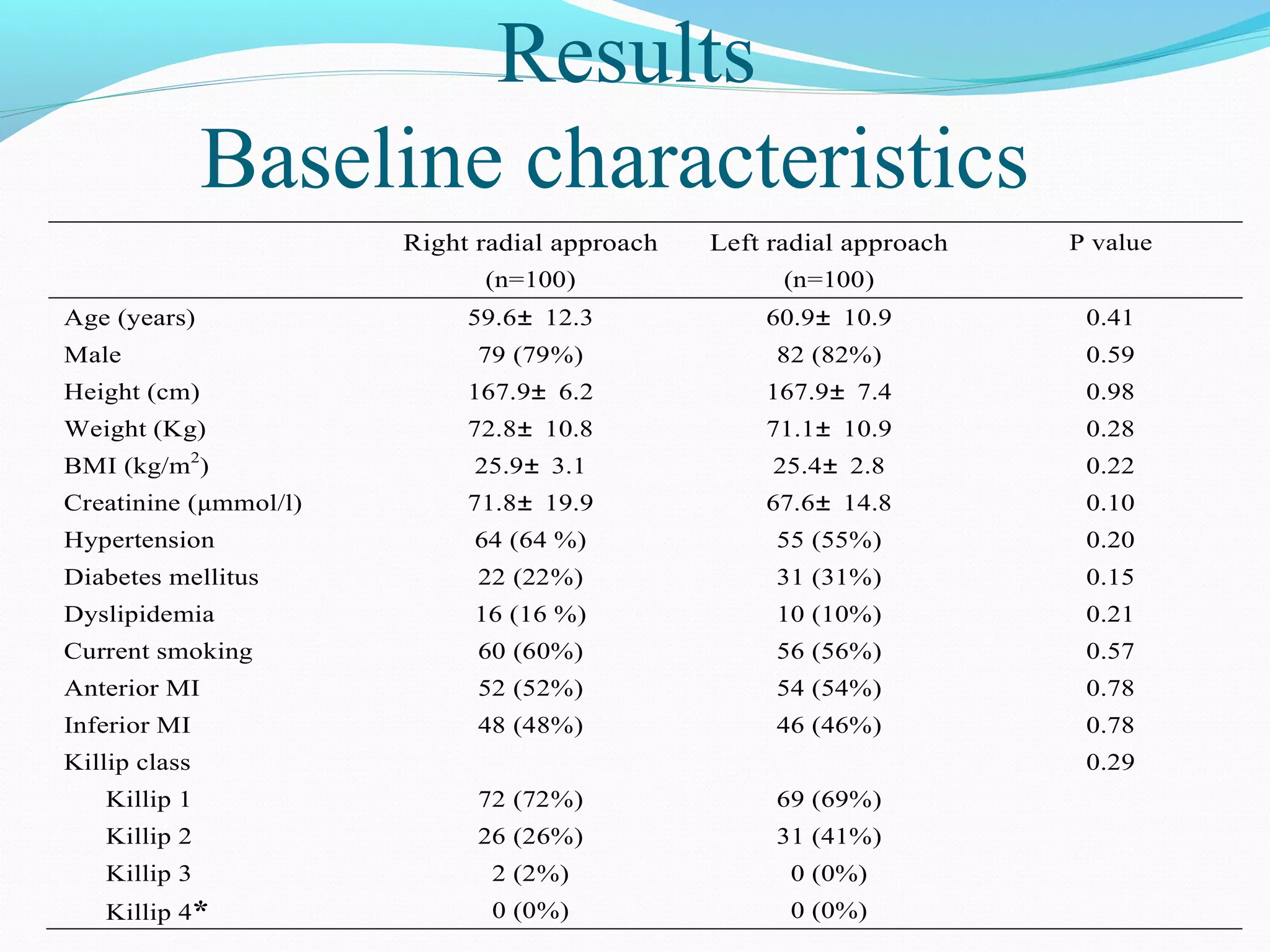
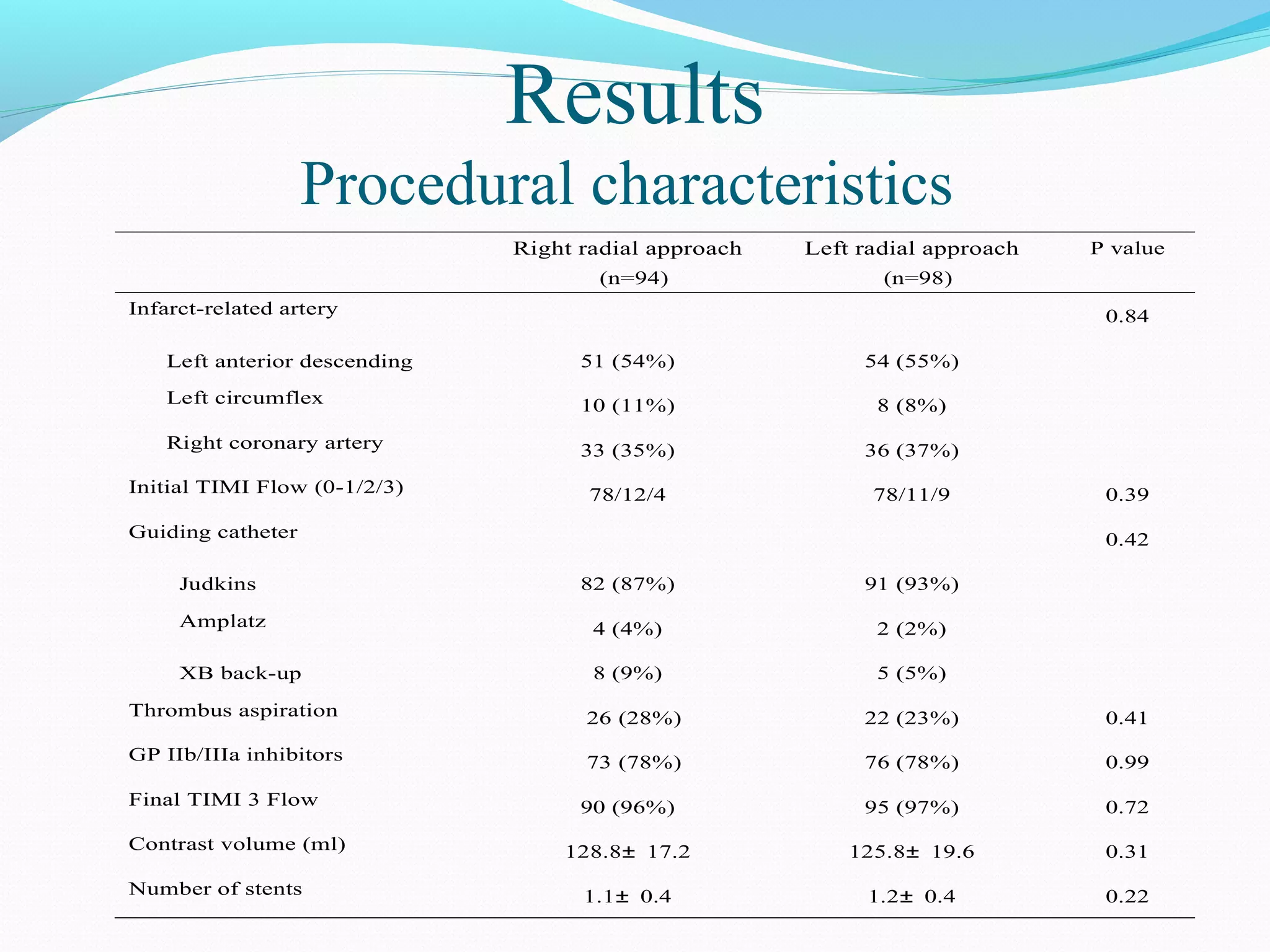
1) The document describes two studies comparing the left radial approach (LRA) and right radial approach (RRA) for coronary angiography and primary PCI in Chinese patients.
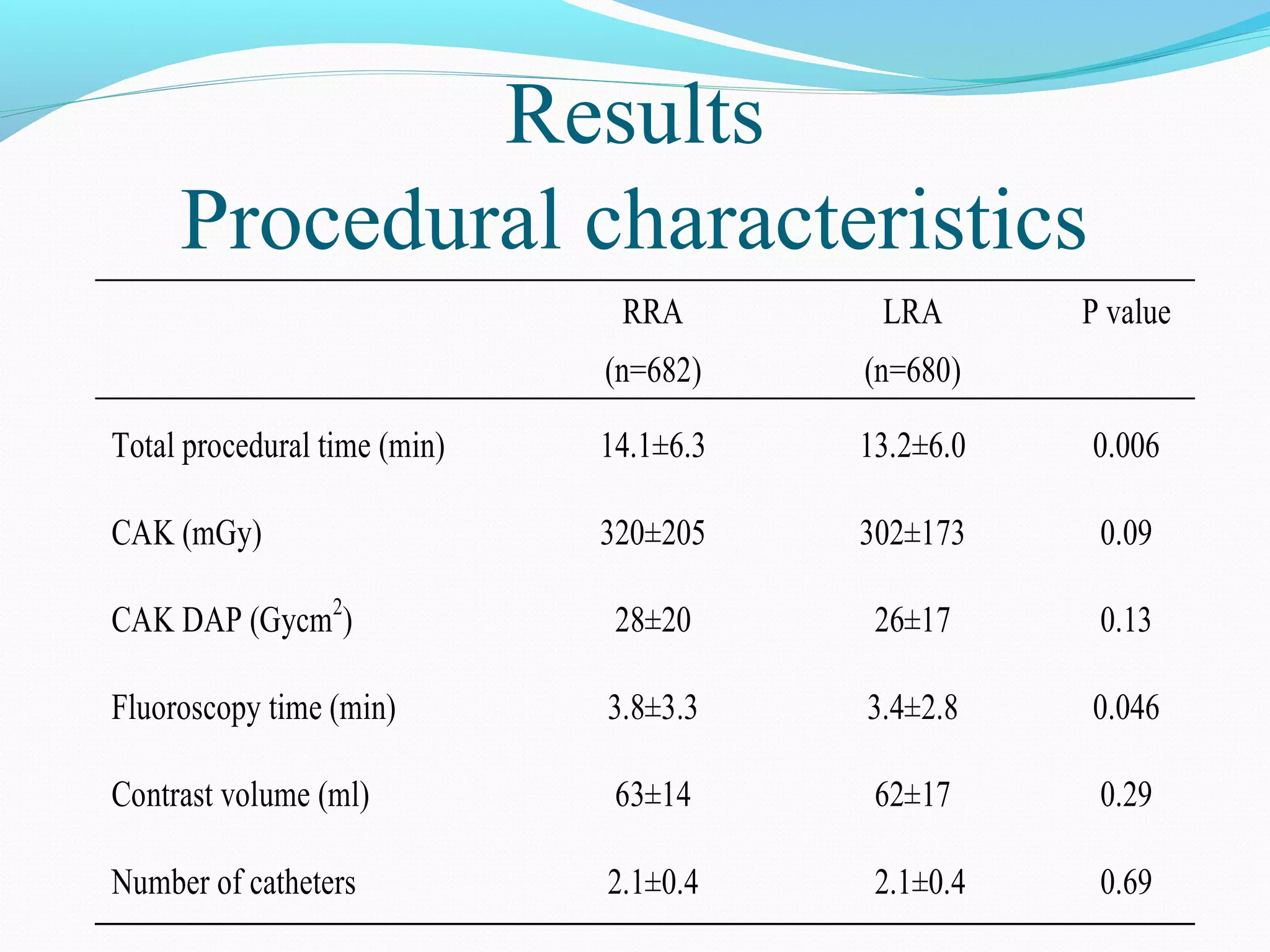
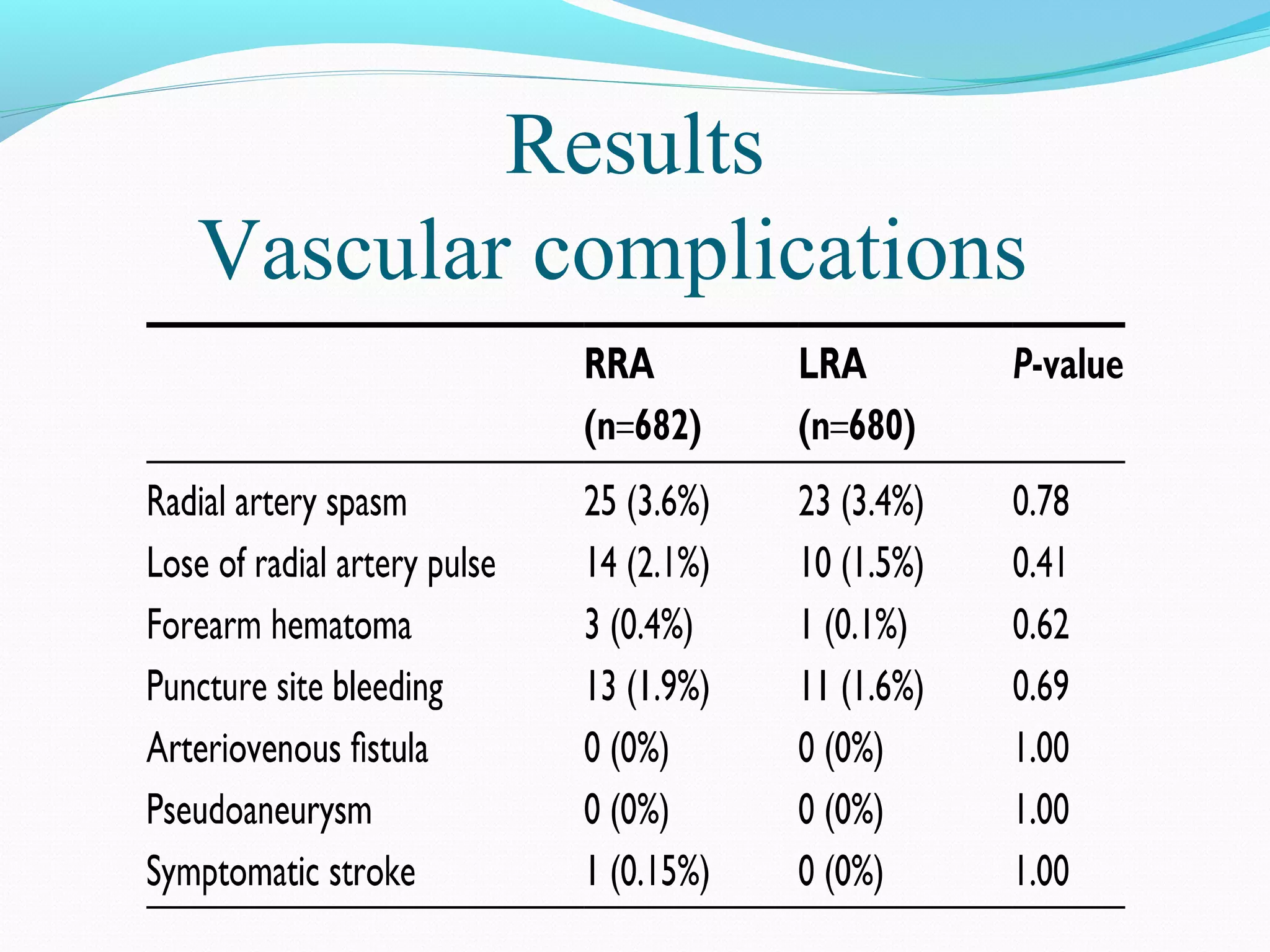
2) In the first study, LRA was associated with shorter procedure time and fluoroscopy time compared to RRA for coronary angiography.
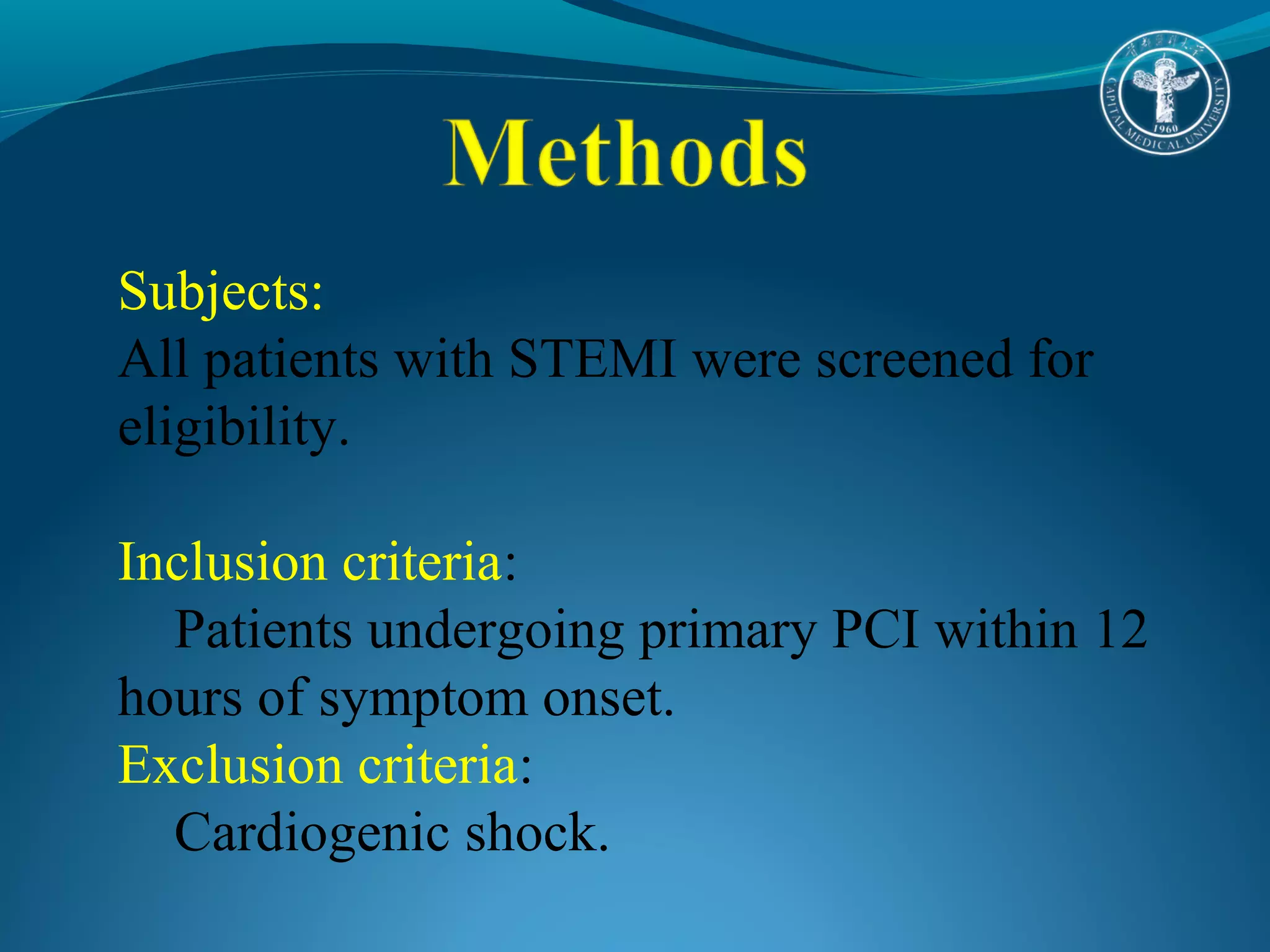
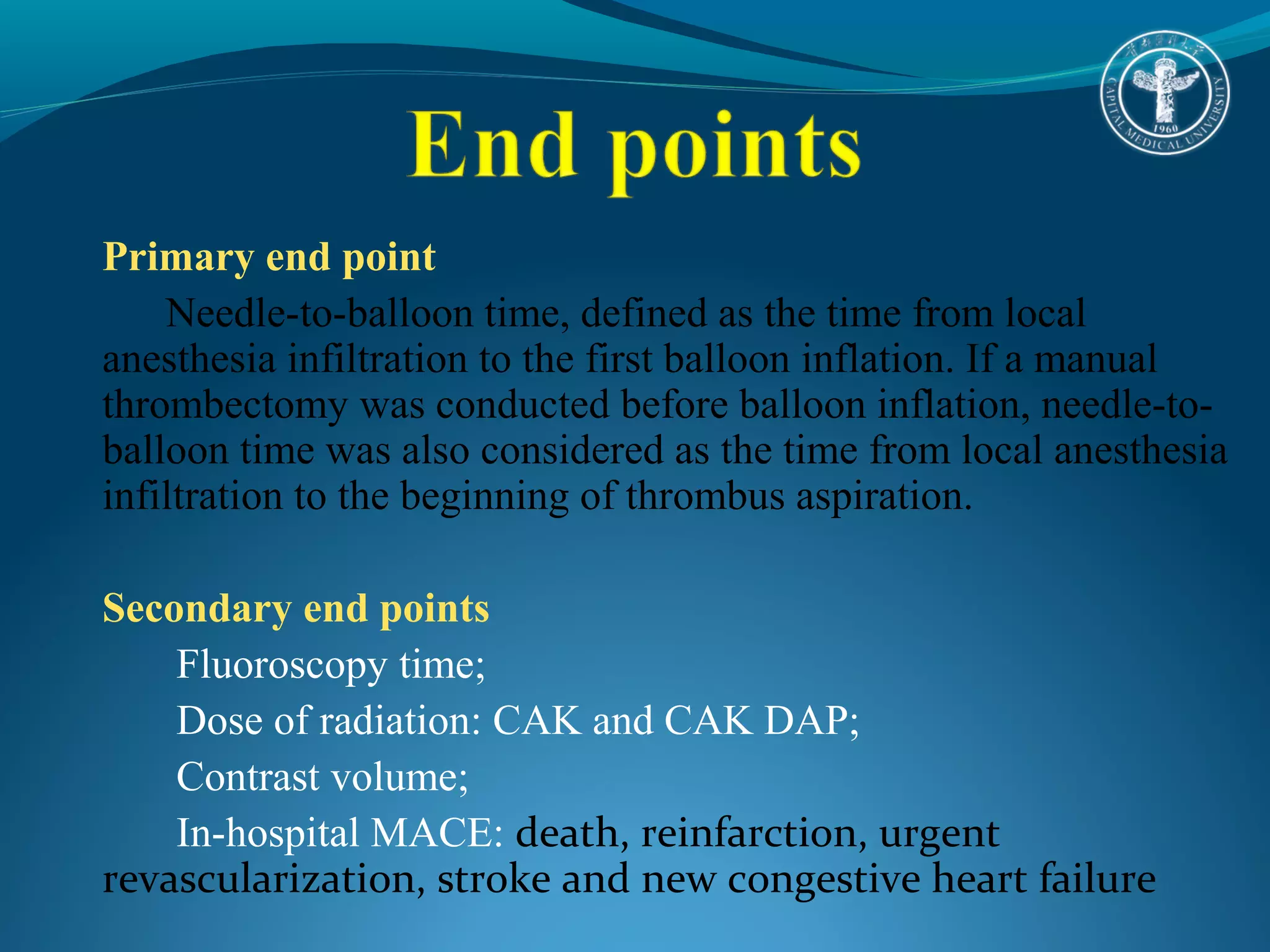
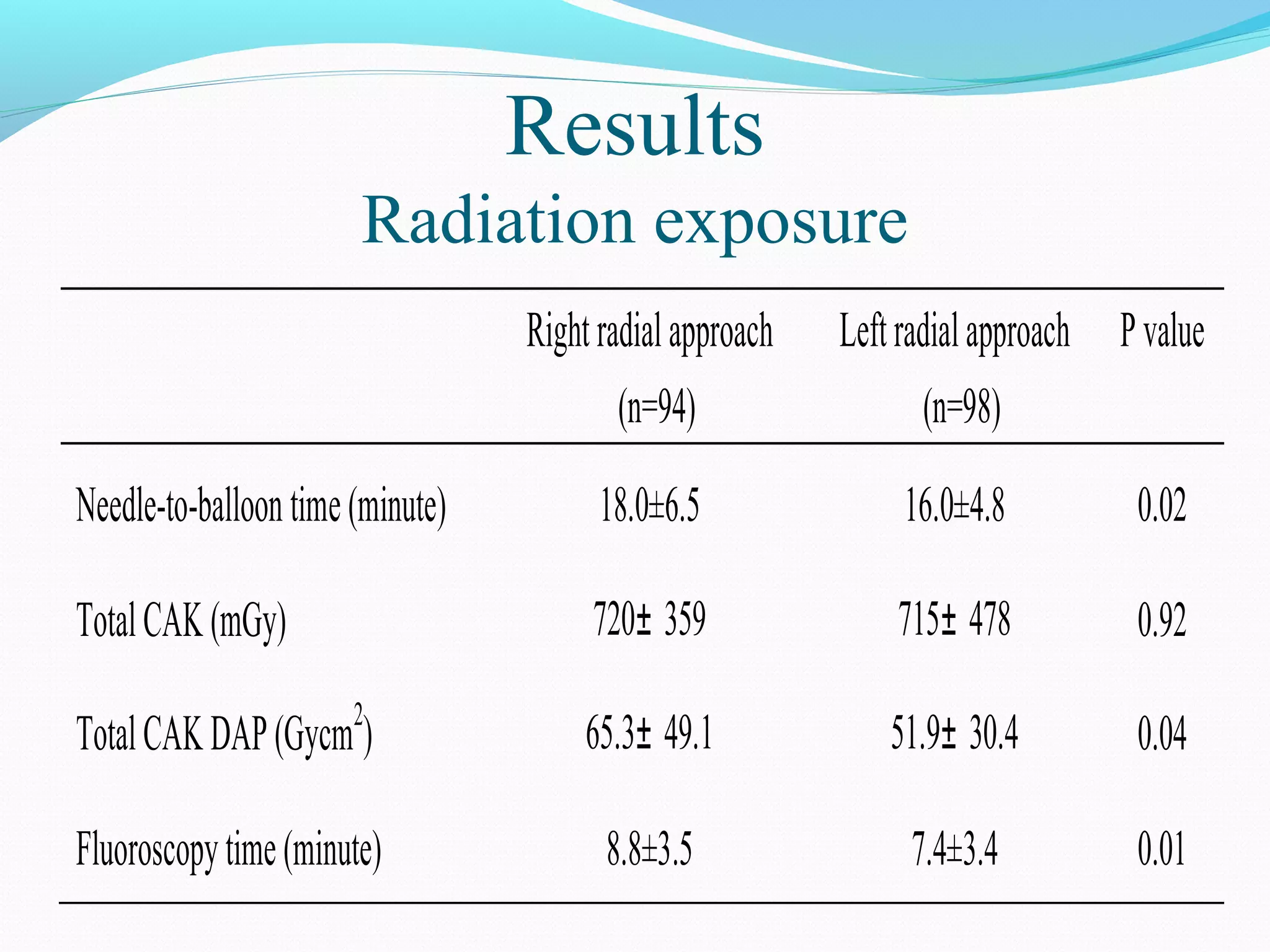
3) In the second study on primary PCI for STEMI, LRA was associated with earlier blood flow restoration in the infarct artery and lower radiation exposure compared to RRA.
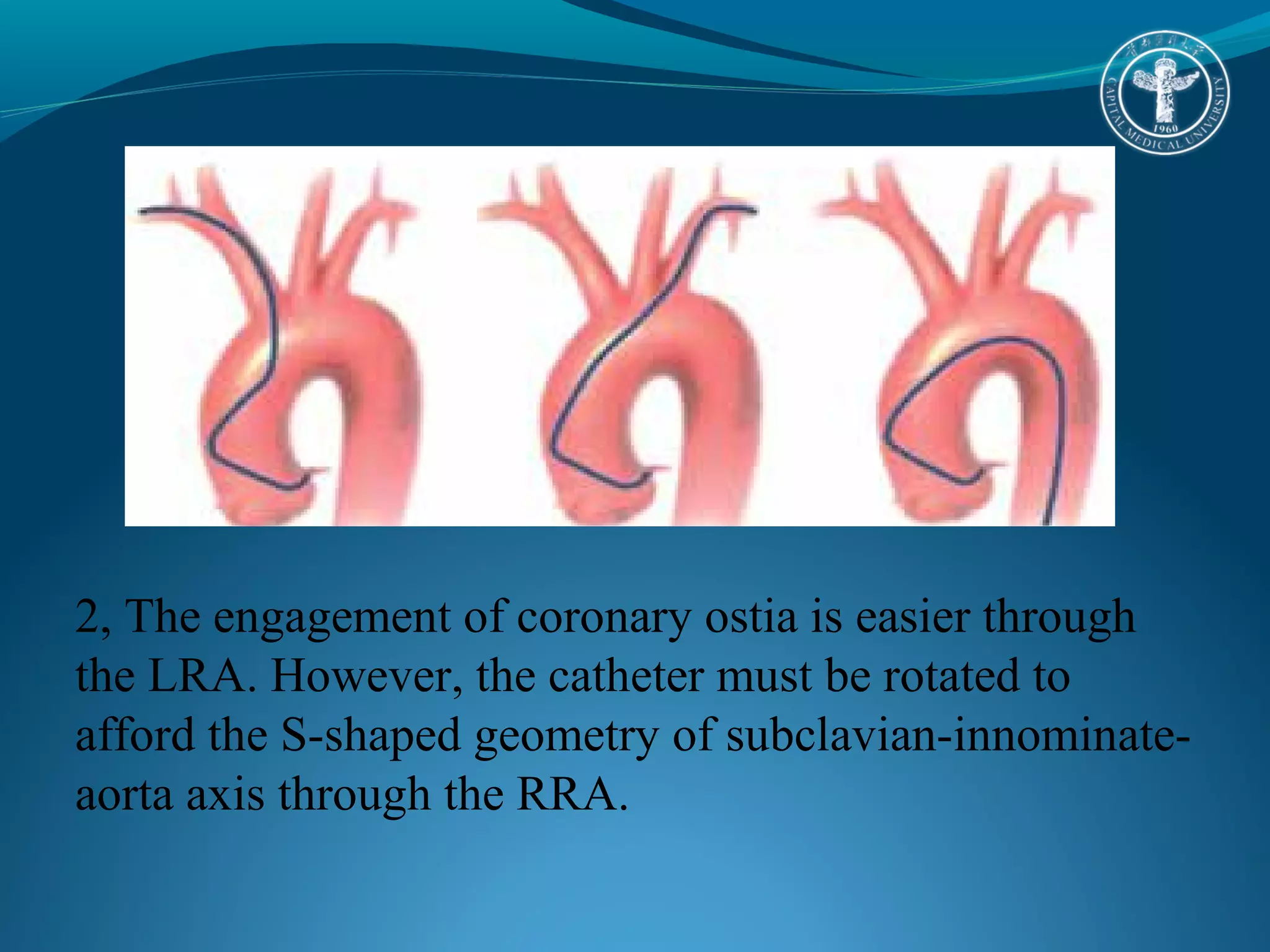
4) Based on the results, LRA may be preferable to RRA due to lower subclavian tortuosity, easier catheter manipulation, and less radiation exposure, especially for urgent cases requiring faster procedures.