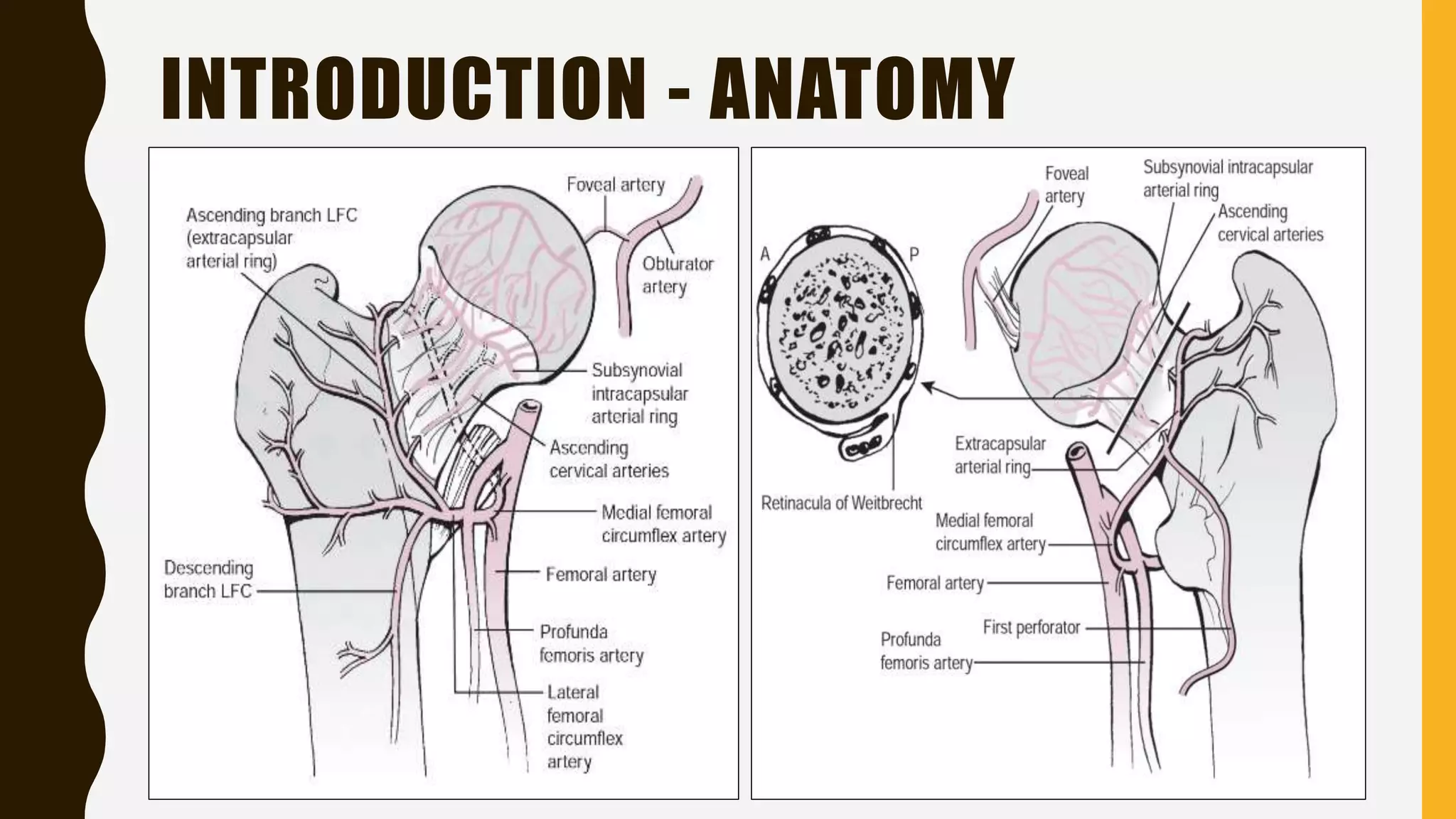
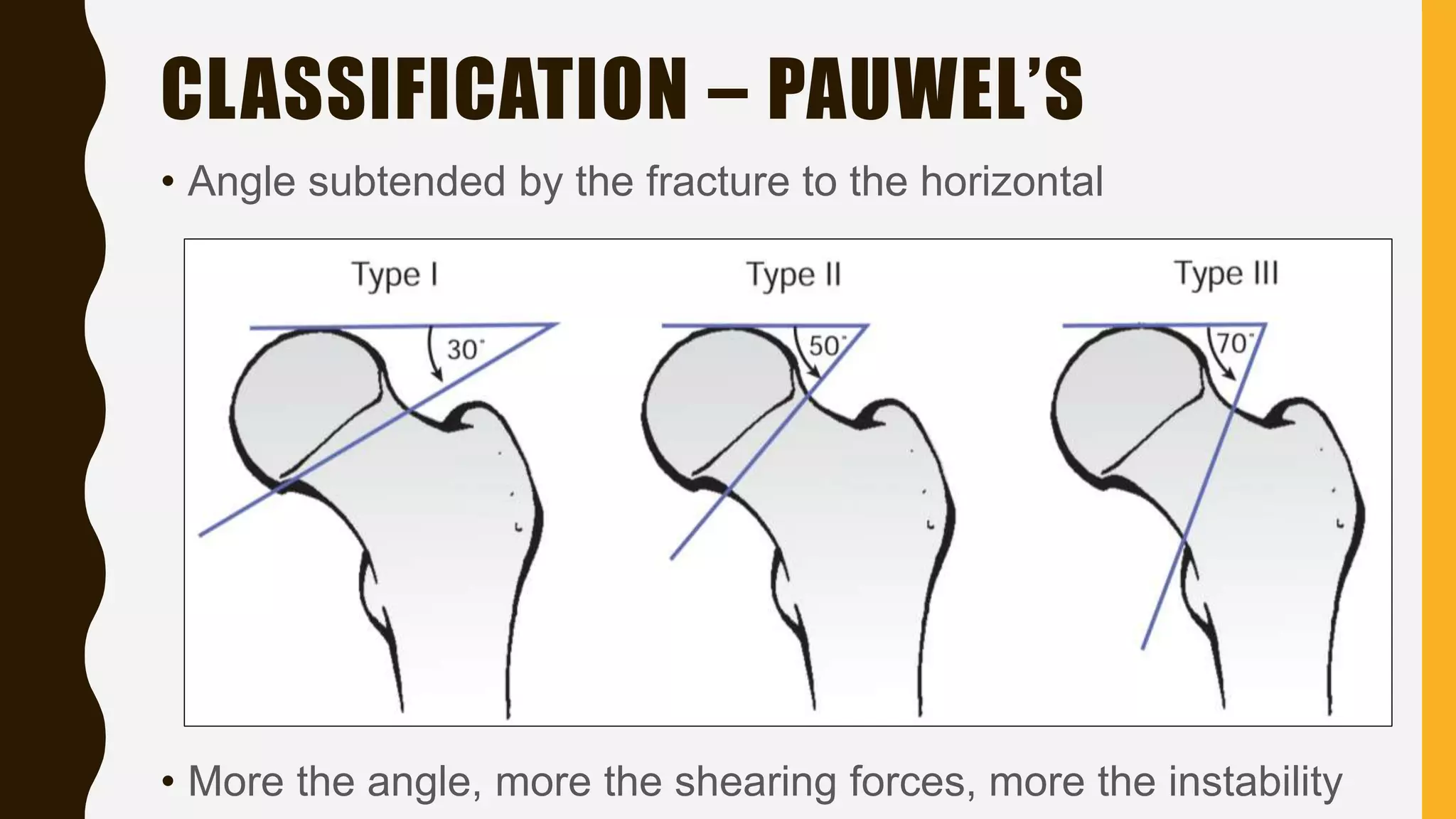
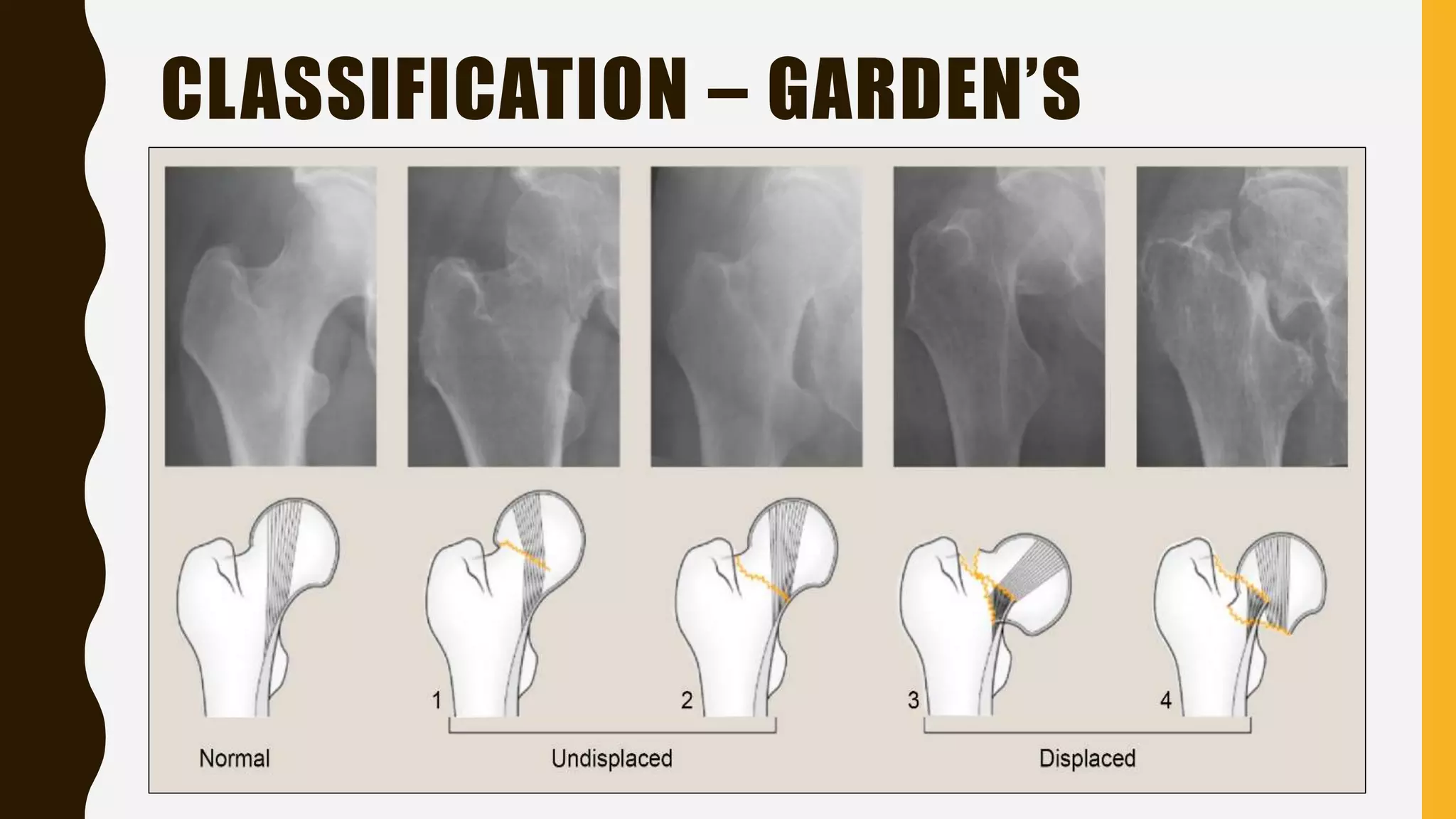
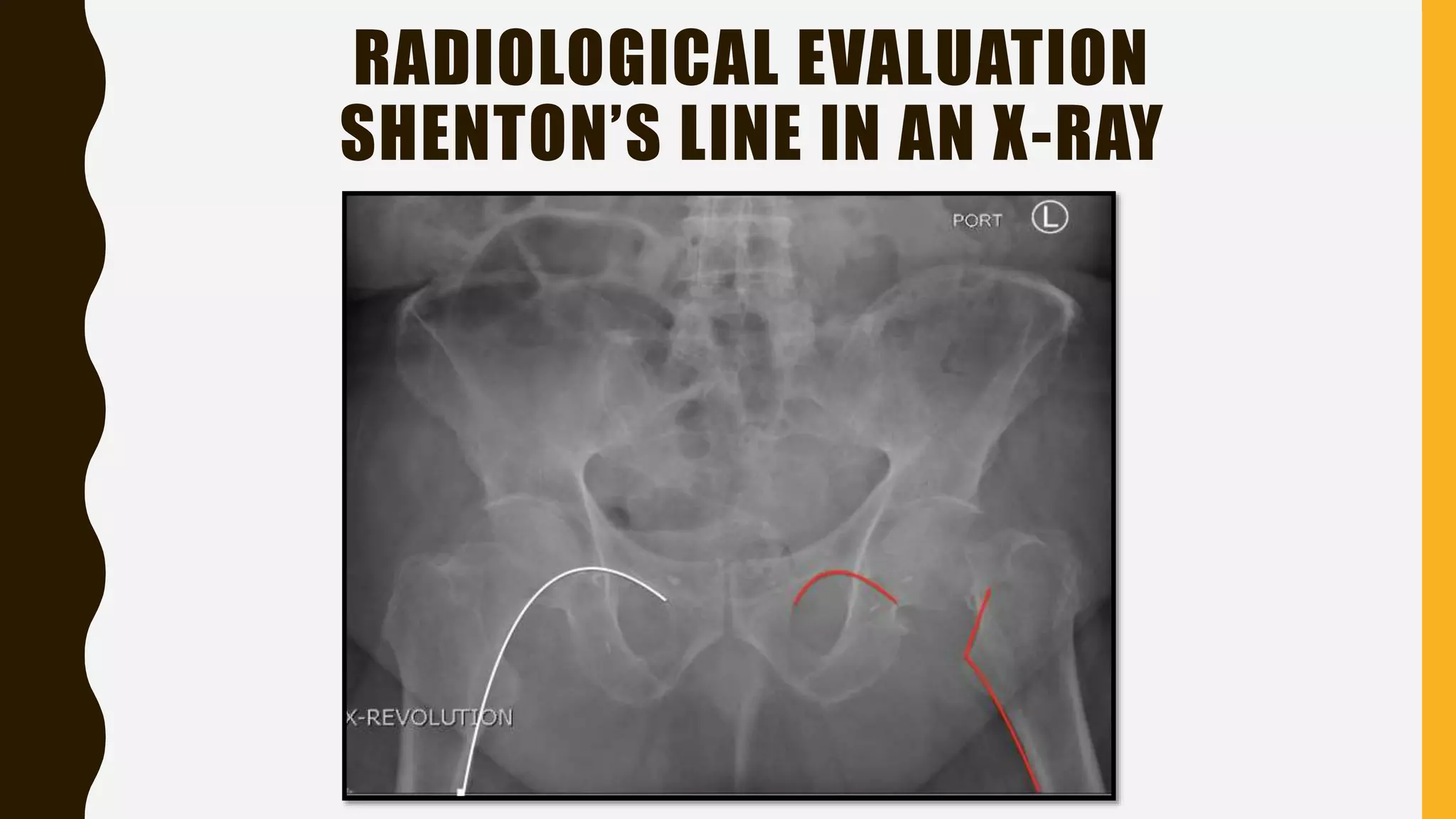
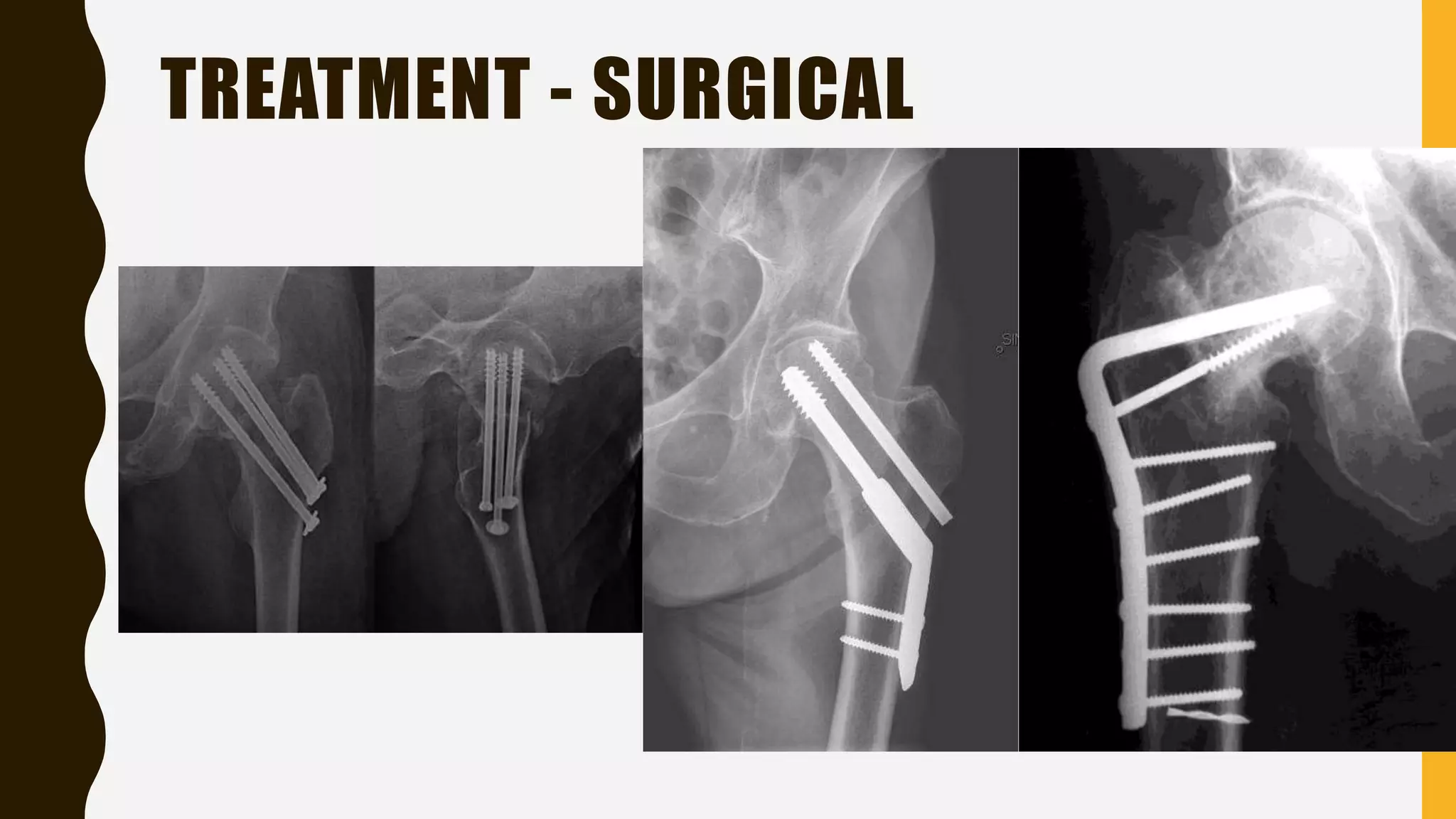
This document discusses the anatomy, blood supply, classification, clinical features, treatment, and complications of fractures of the neck of the femur. It notes that these fractures most commonly occur in elderly women due to low-energy falls. The goals of treatment are to minimize discomfort, restore hip function, achieve early stable fixation or prosthetic replacement, and allow rapid mobilization. Surgical options include internal fixation with screws or plates for younger patients or total hip replacement or hemiarthroplasty for elderly patients. Complications can include non-union, osteonecrosis, fixation failure, and issues associated with prolonged immobilization.