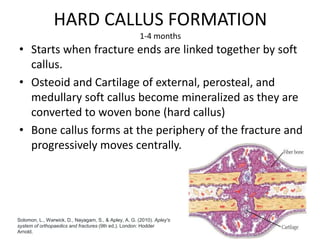
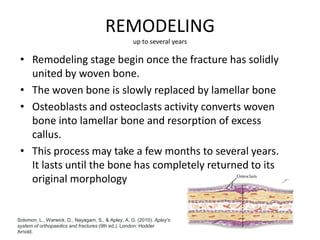
Fracture healing occurs through either primary or secondary bone healing. Primary healing involves direct bone formation without callus and requires perfect stability, while secondary healing involves callus formation over 4 stages - inflammation, soft callus formation, hard callus formation, and remodeling. Several internal and external factors can influence fracture healing, including blood supply, stability, bone stimulators, COX-2 levels, patient diet, diabetes, nicotine use, medications, and health conditions.