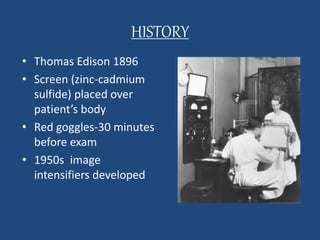
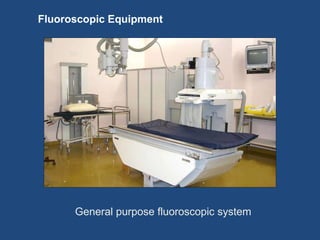
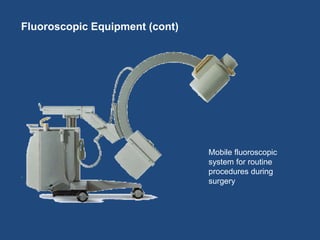
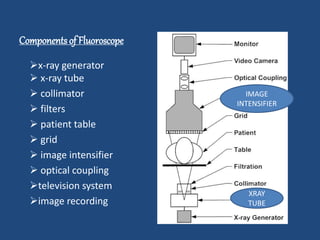
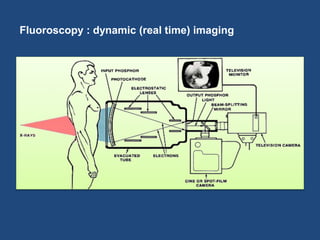
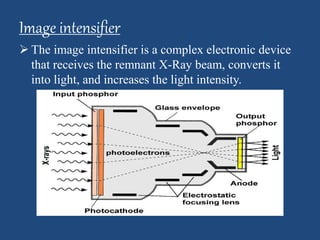
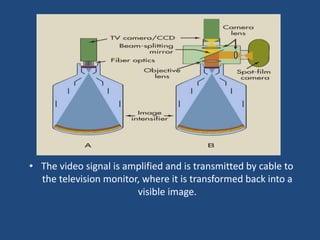
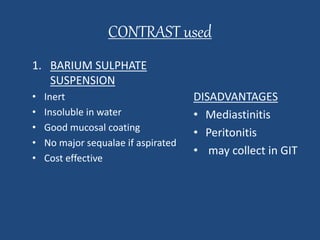
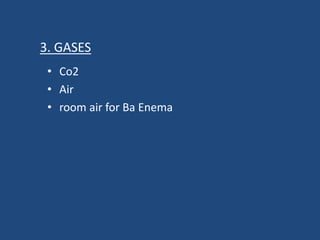
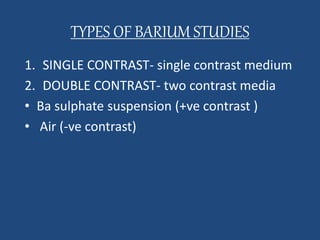
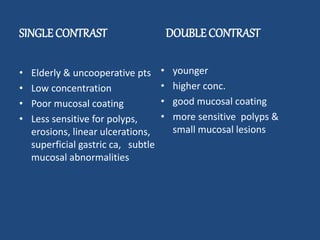
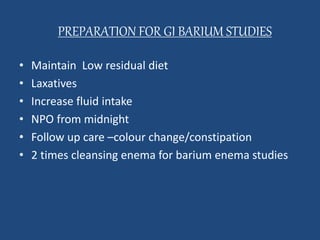
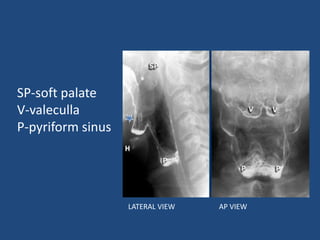
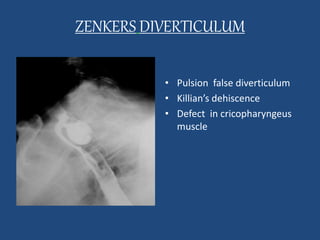
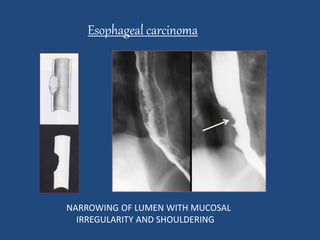
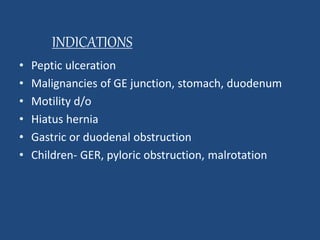
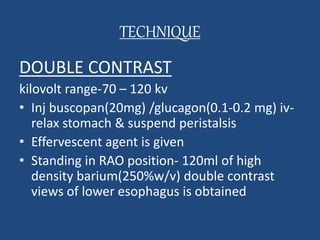
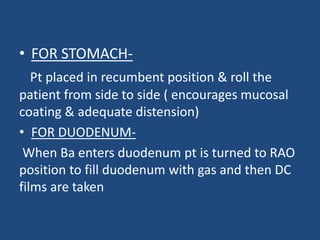
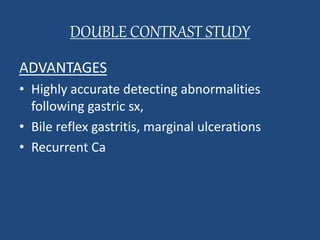
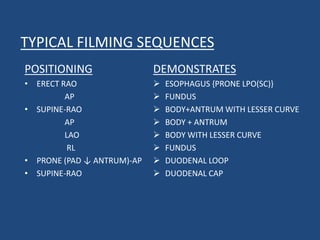
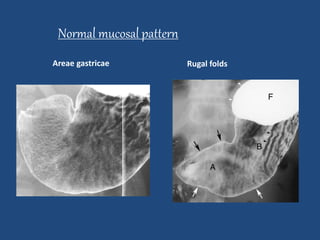
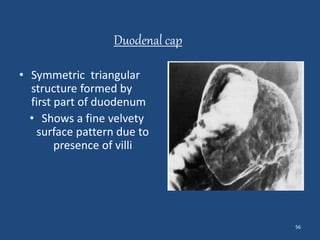
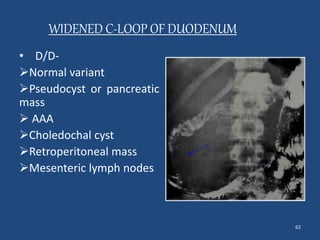
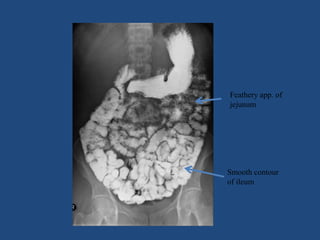
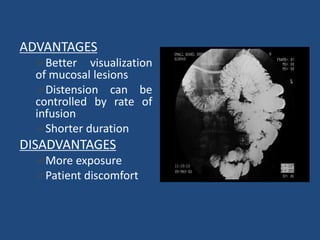
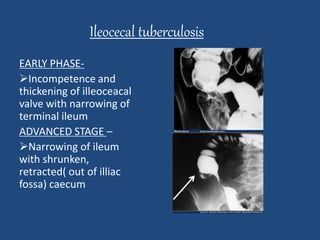
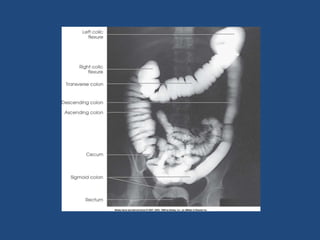
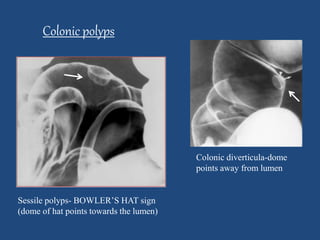
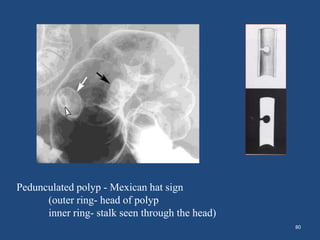
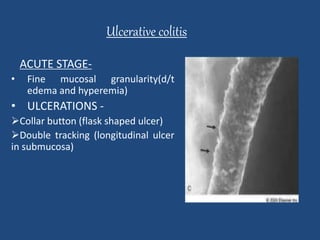
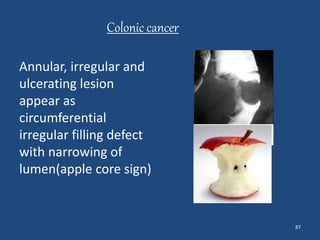
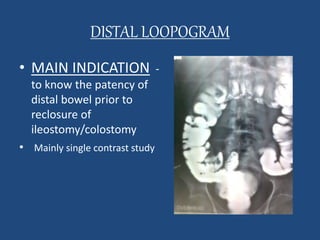
This document discusses various fluoroscopic procedures used in radiology. It begins by describing fluoroscopy as an imaging technique using real-time x-ray images. It then discusses the components of a fluoroscopy unit and how images are monitored. Various procedures using fluoroscopy and barium are described, including barium swallow, barium meal, follow through, and enema. Common indications, techniques, findings, and complications are summarized for each procedure. Contrast agents and preparation for GI studies are also outlined.