The document discusses the etiology, pathophysiology, diagnosis and management of asthma. Some key points:
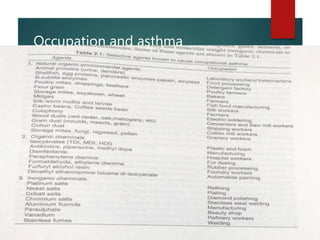
- Atopic allergy and allergy to common inhalants like house dust mites, pollens and molds contribute to 75-85% of asthma cases. Occupational allergens can also cause asthma.
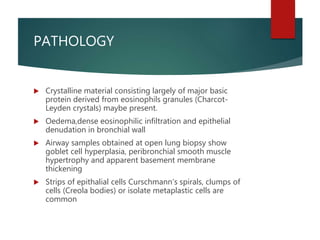
- Pathophysiology involves airway smooth muscle contraction, epithelial secretions and inflammatory edema narrowing the airways. Early and late phase asthmatic reactions are mediated by IgE and inflammatory cells/mediators.
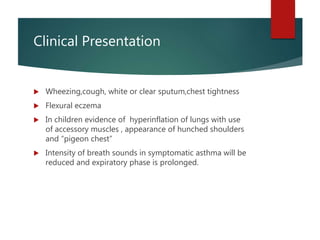
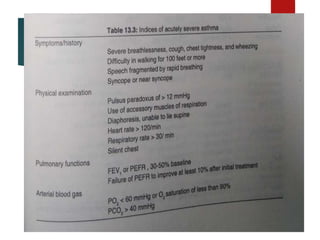
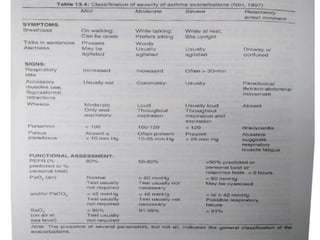
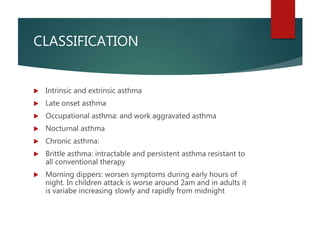
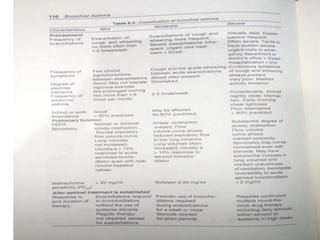
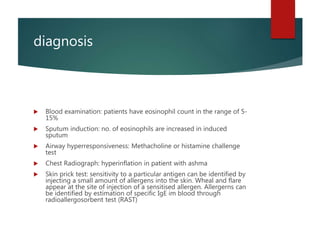
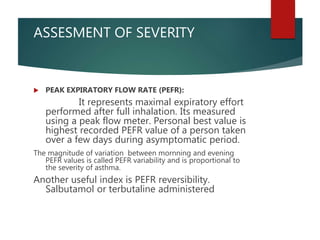
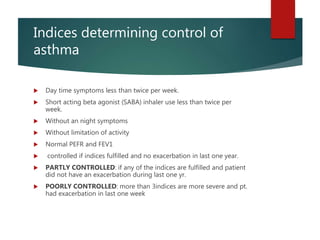
- Diagnosis involves assessing symptoms, lung function tests like spirometry, allergy tests and inflammation markers. Severity is classified based on symptoms, lung function