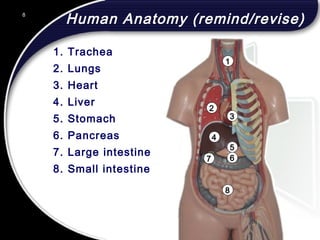
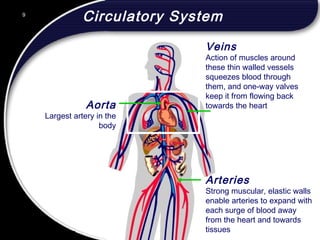
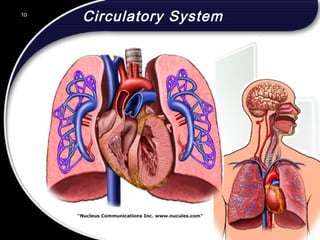
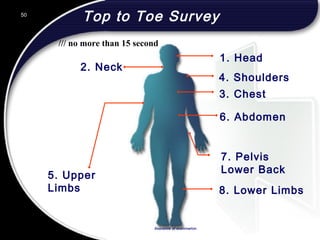
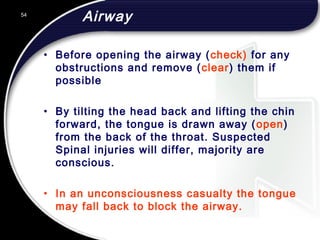
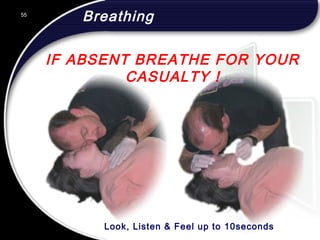
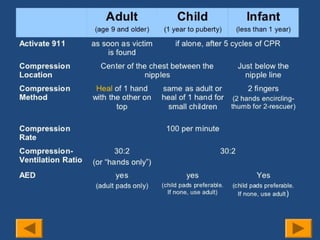
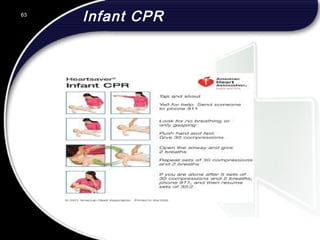
This document outlines the contents and objectives of an emergency first aid course. The course will cover topics such as human anatomy, the responsibilities of a first aider, assessment of casualties, CPR, and use of an automated external defibrillator. The goal is for cabin crew to be able to identify medical conditions, apply first aid, and deal with emergencies that may occur on an aircraft. The document provides an agenda that will allocate 1 hour to theory and 2 hours to hands-on training.