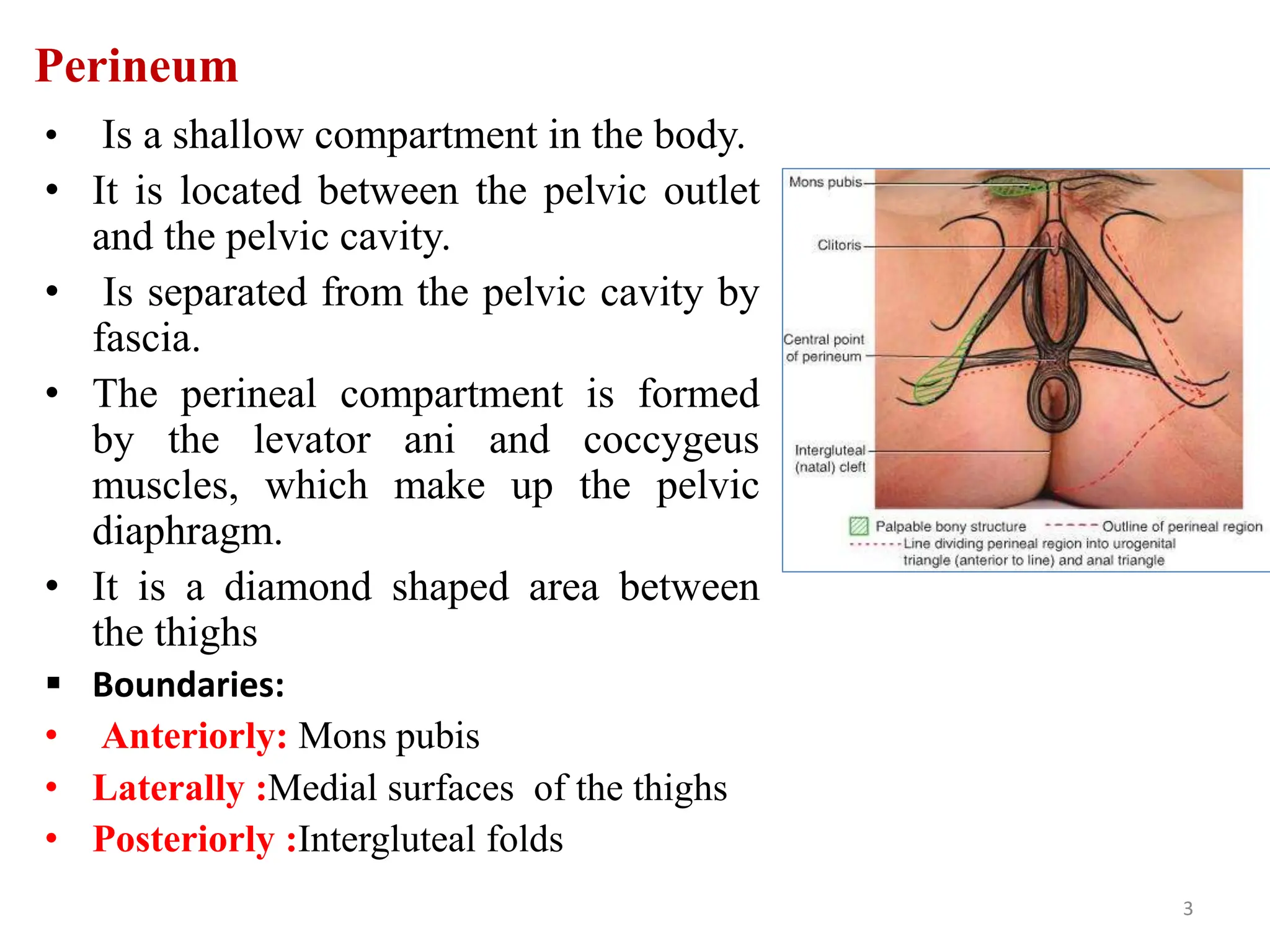
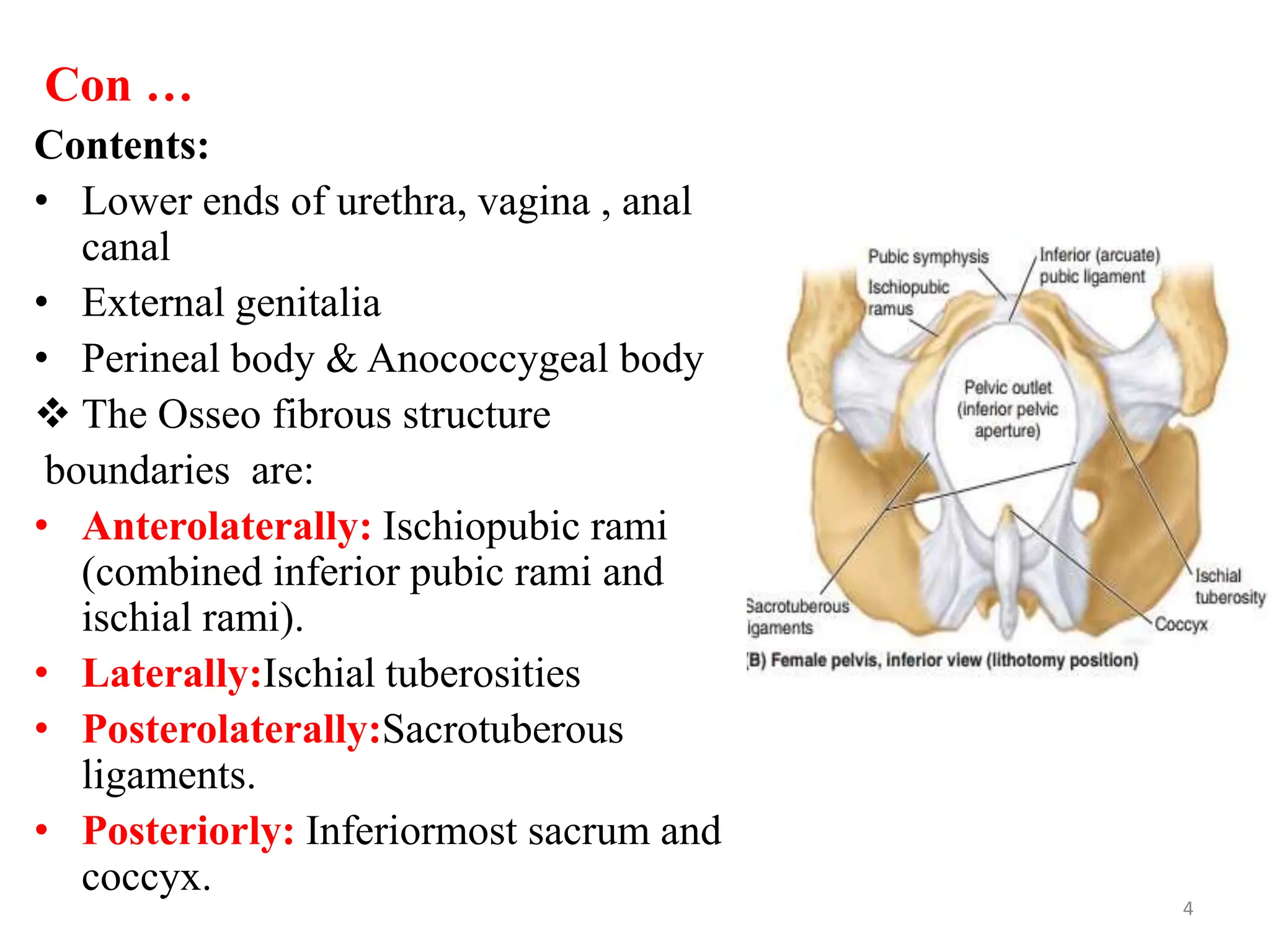
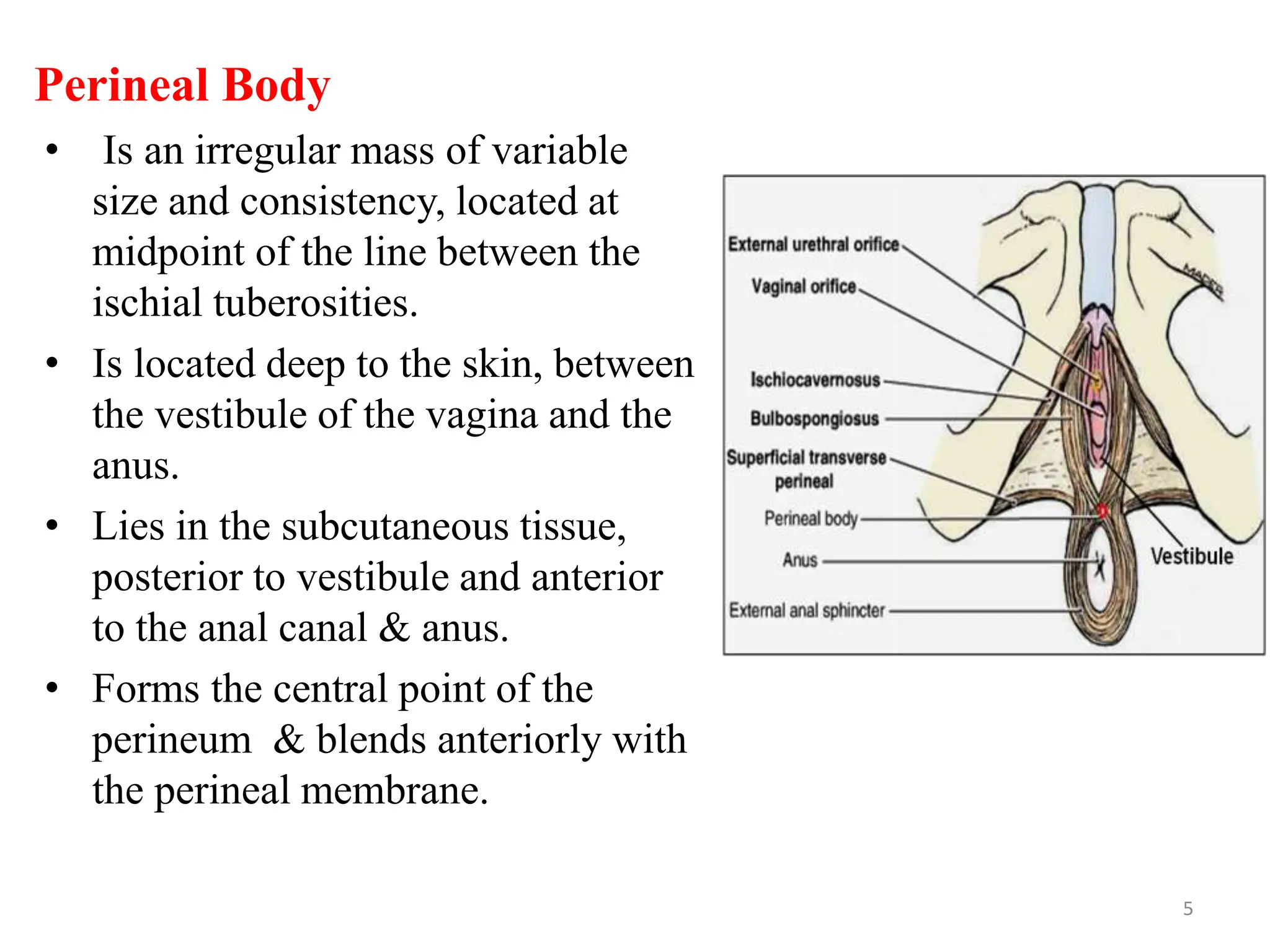
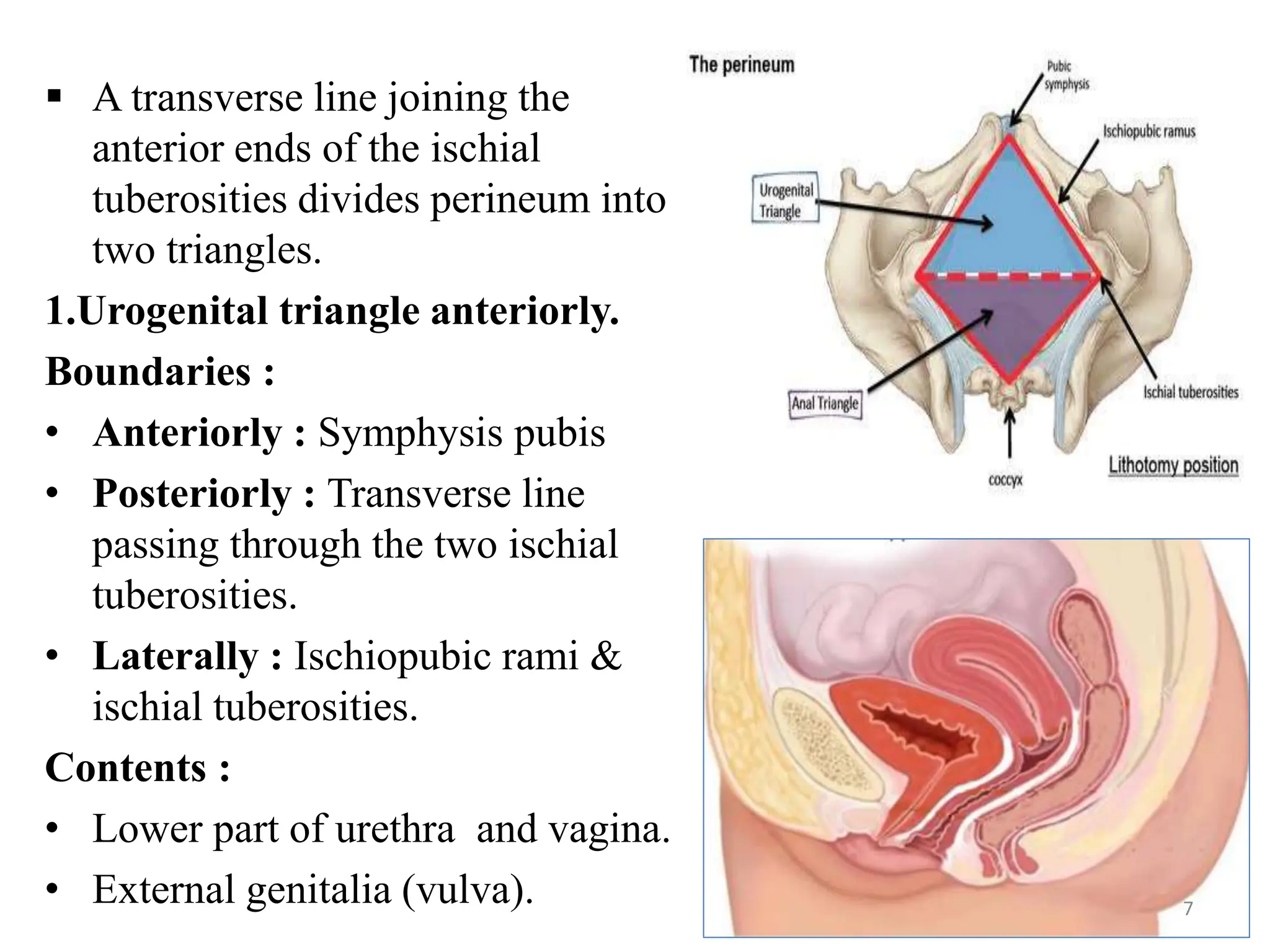
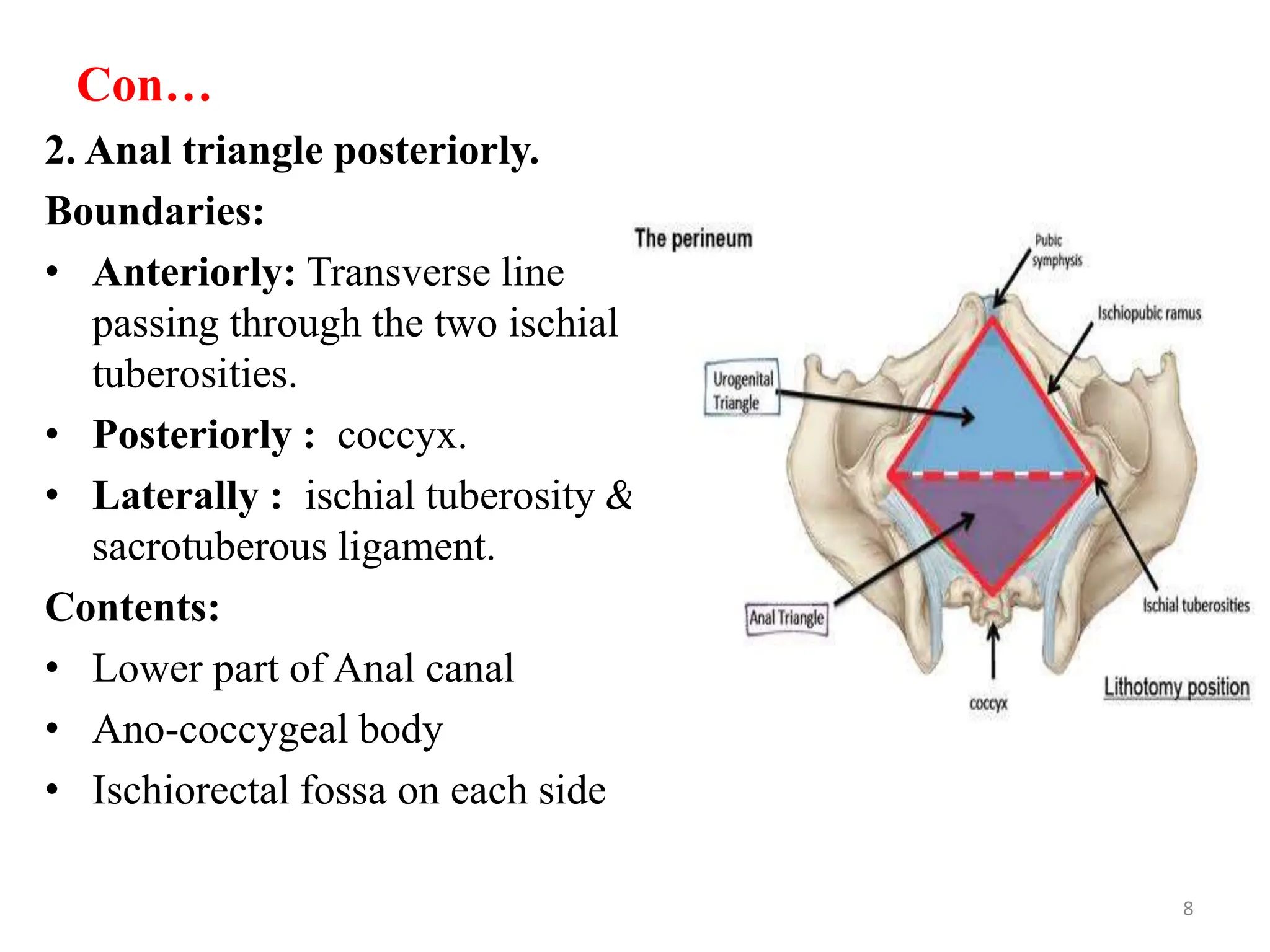
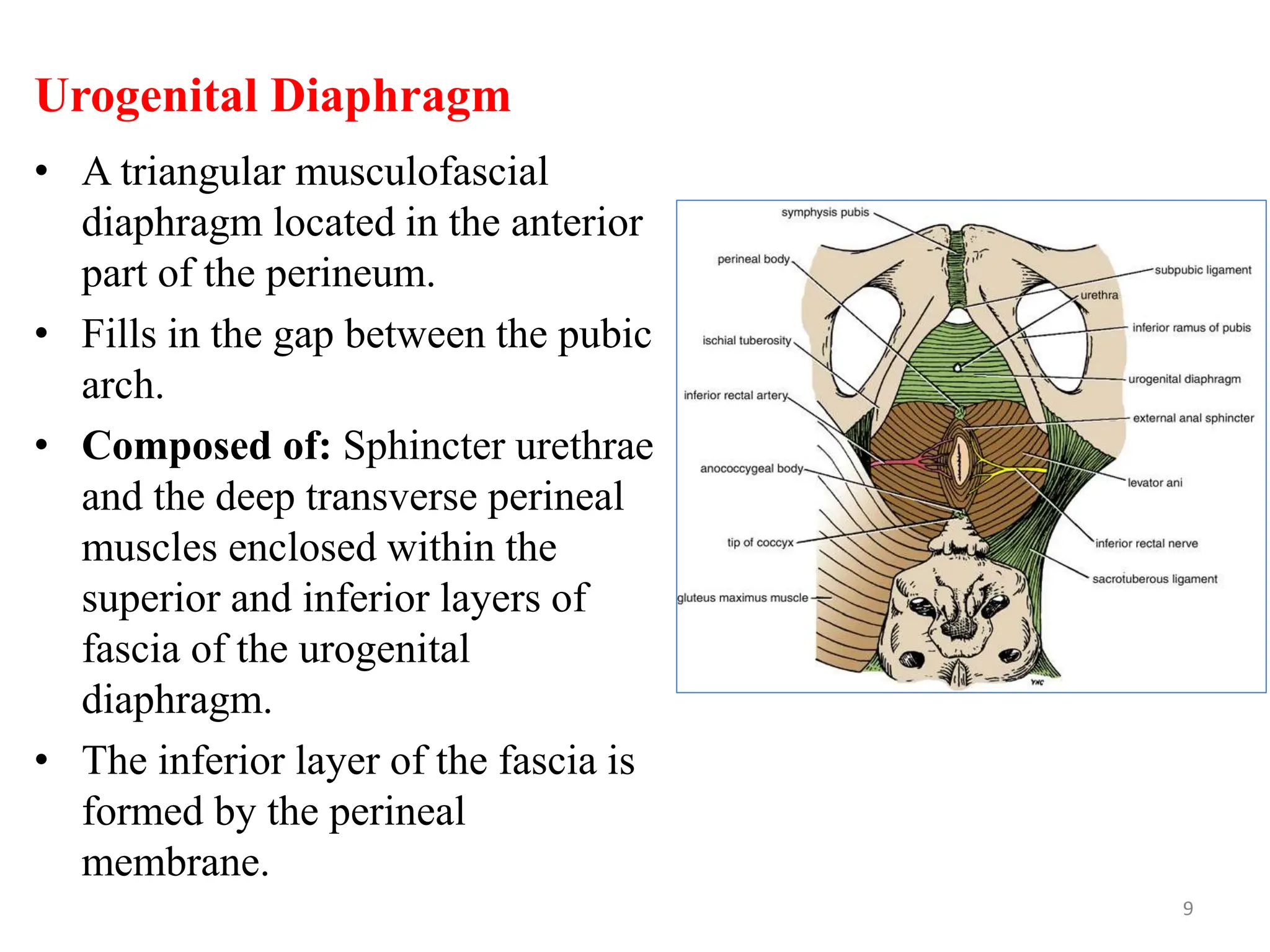
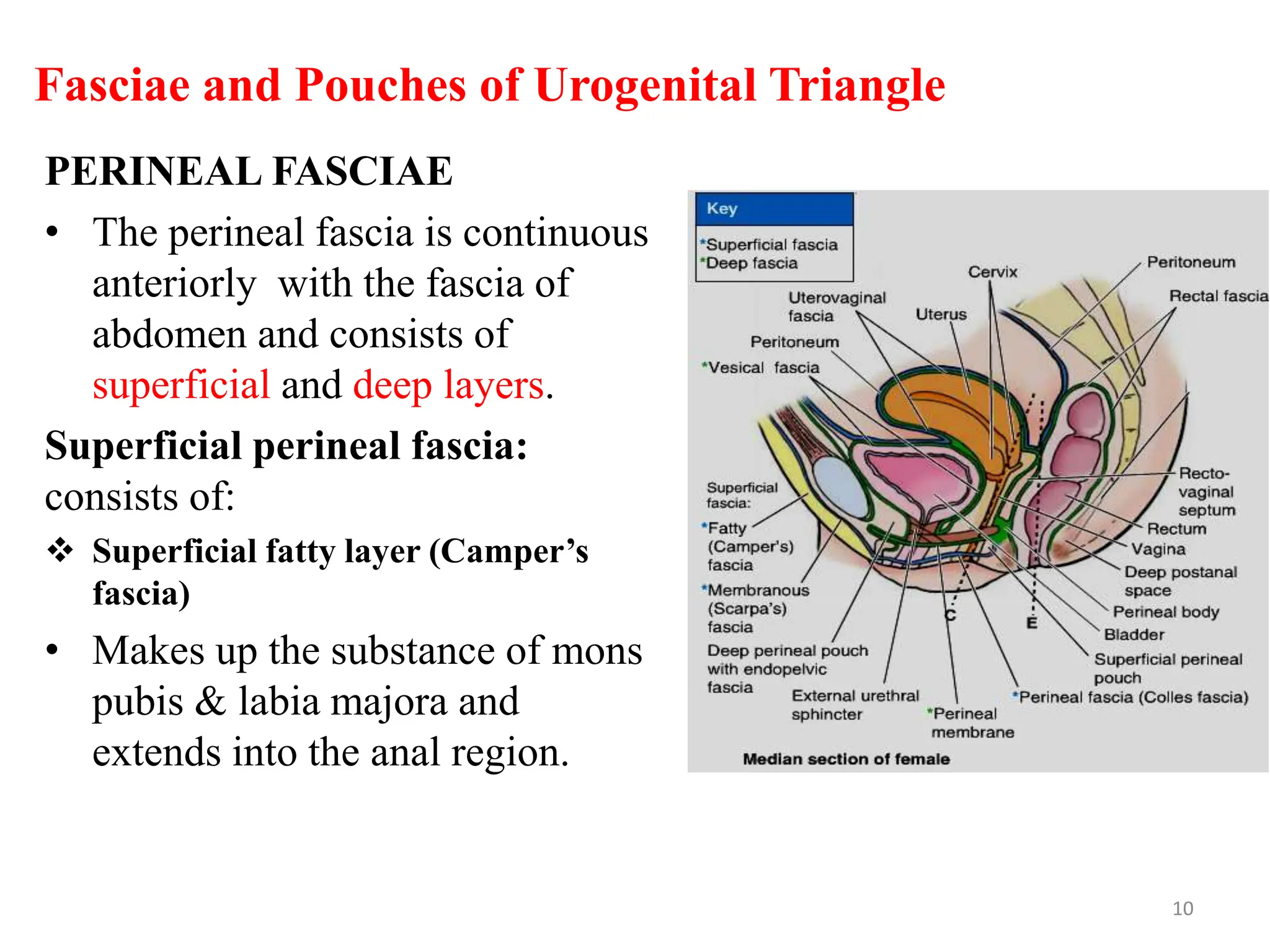
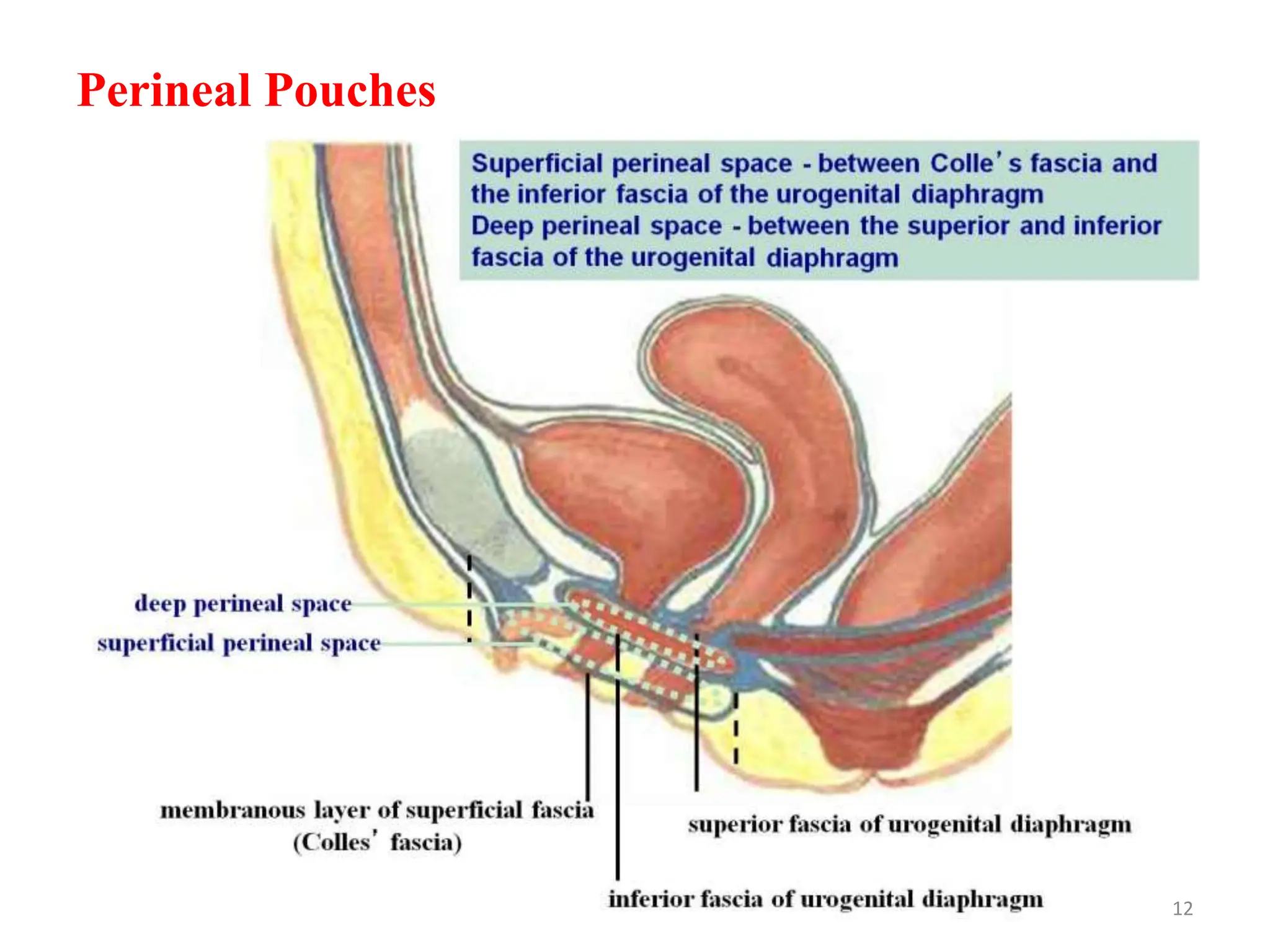
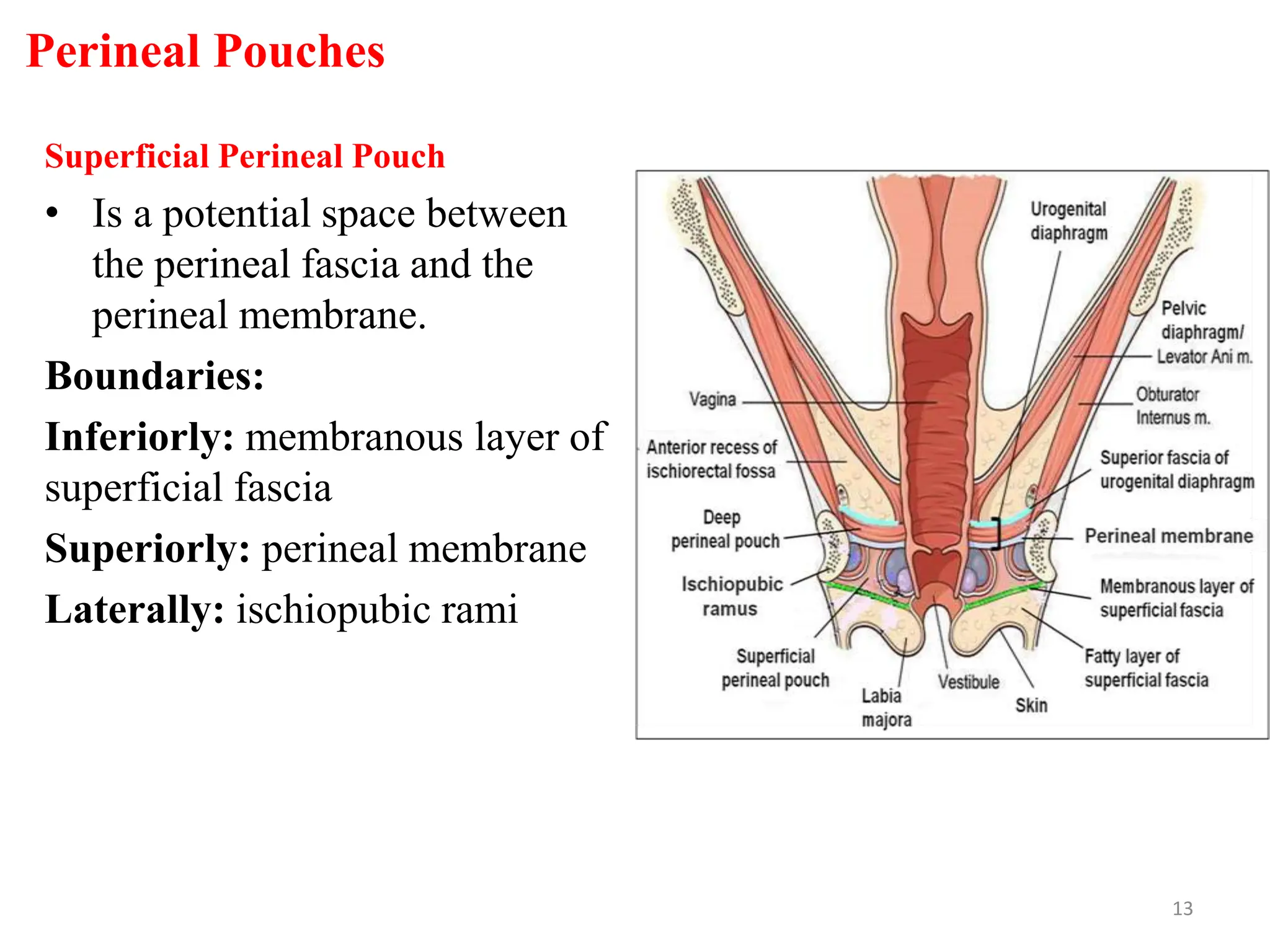
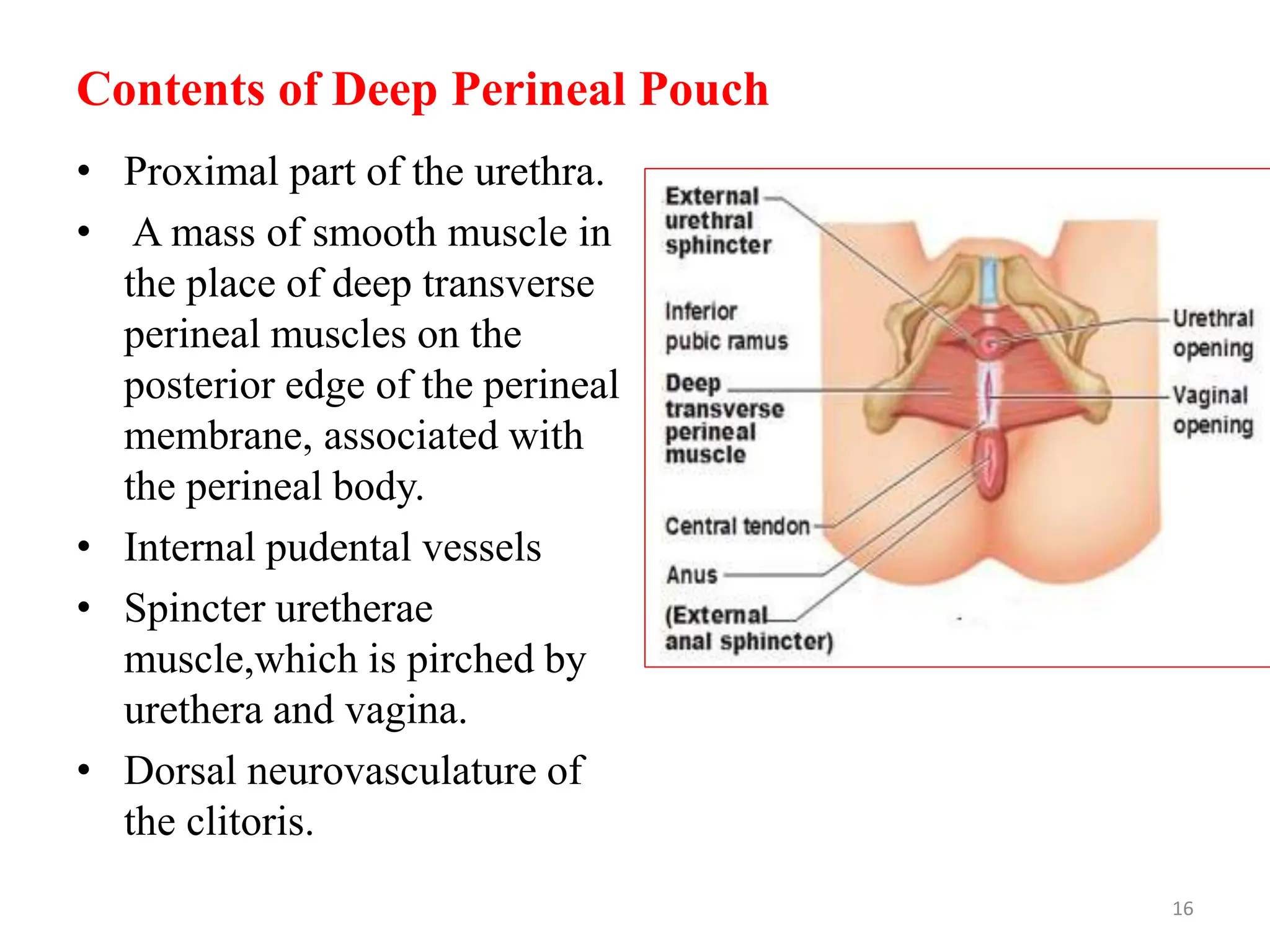
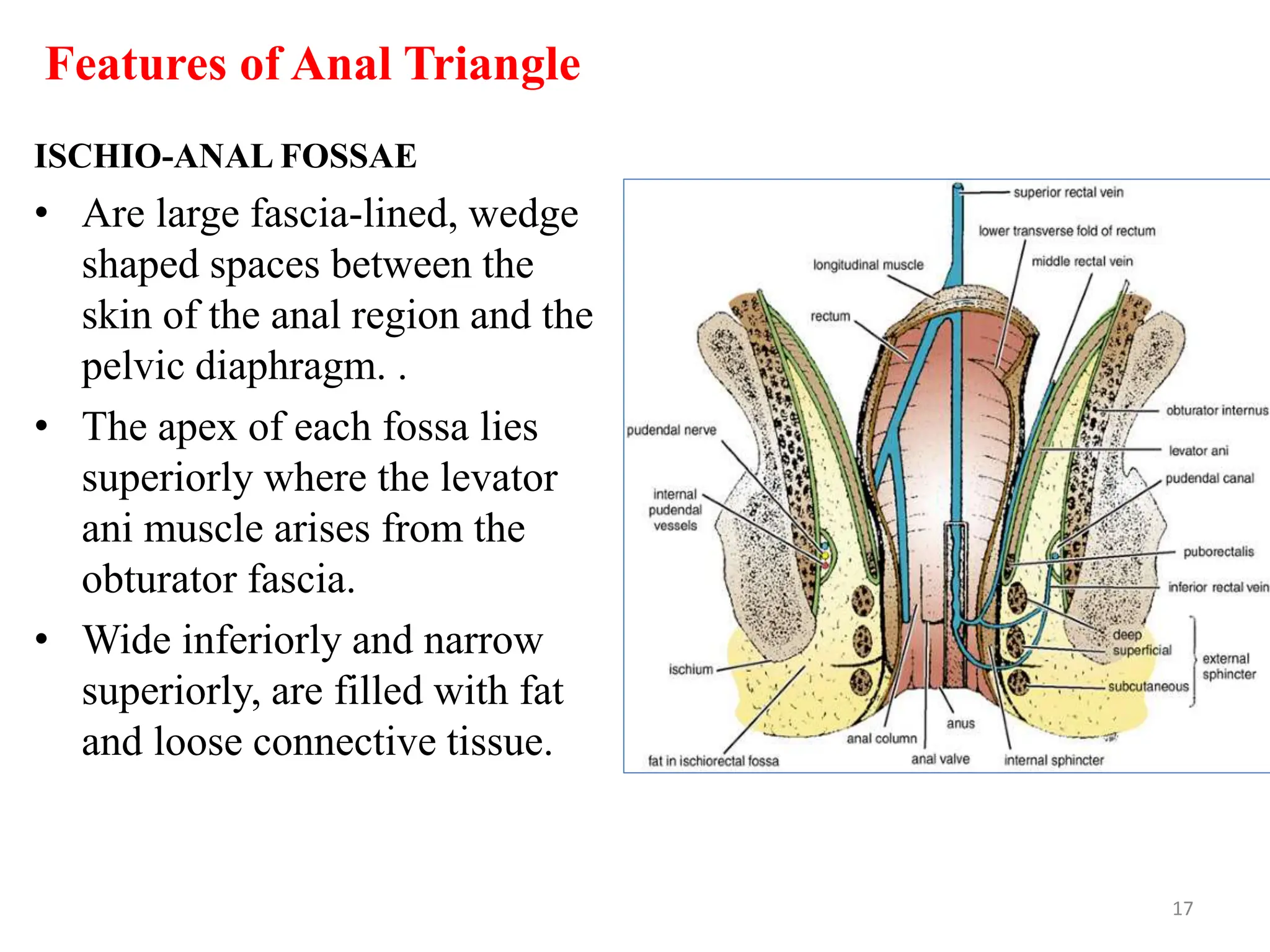
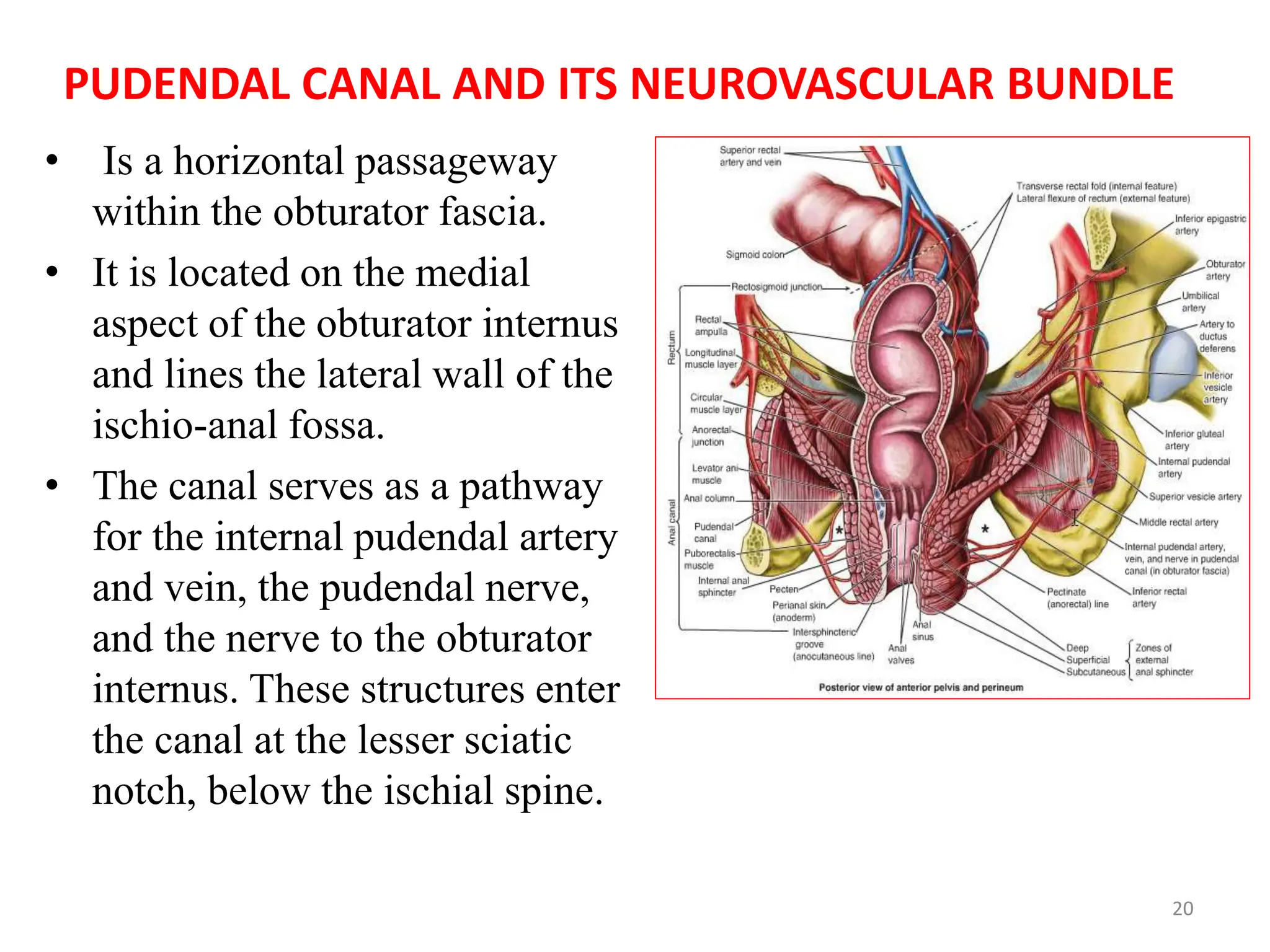
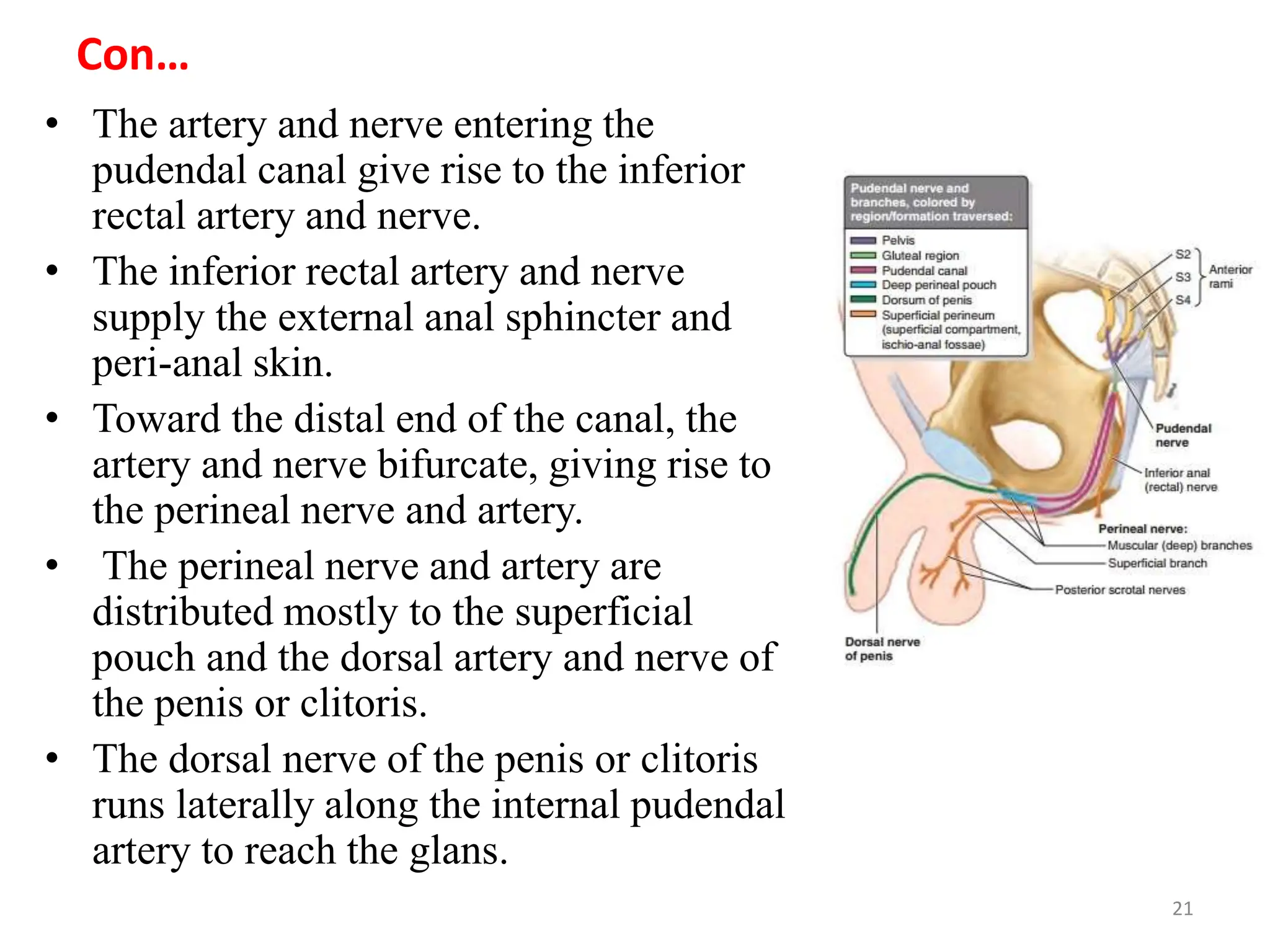
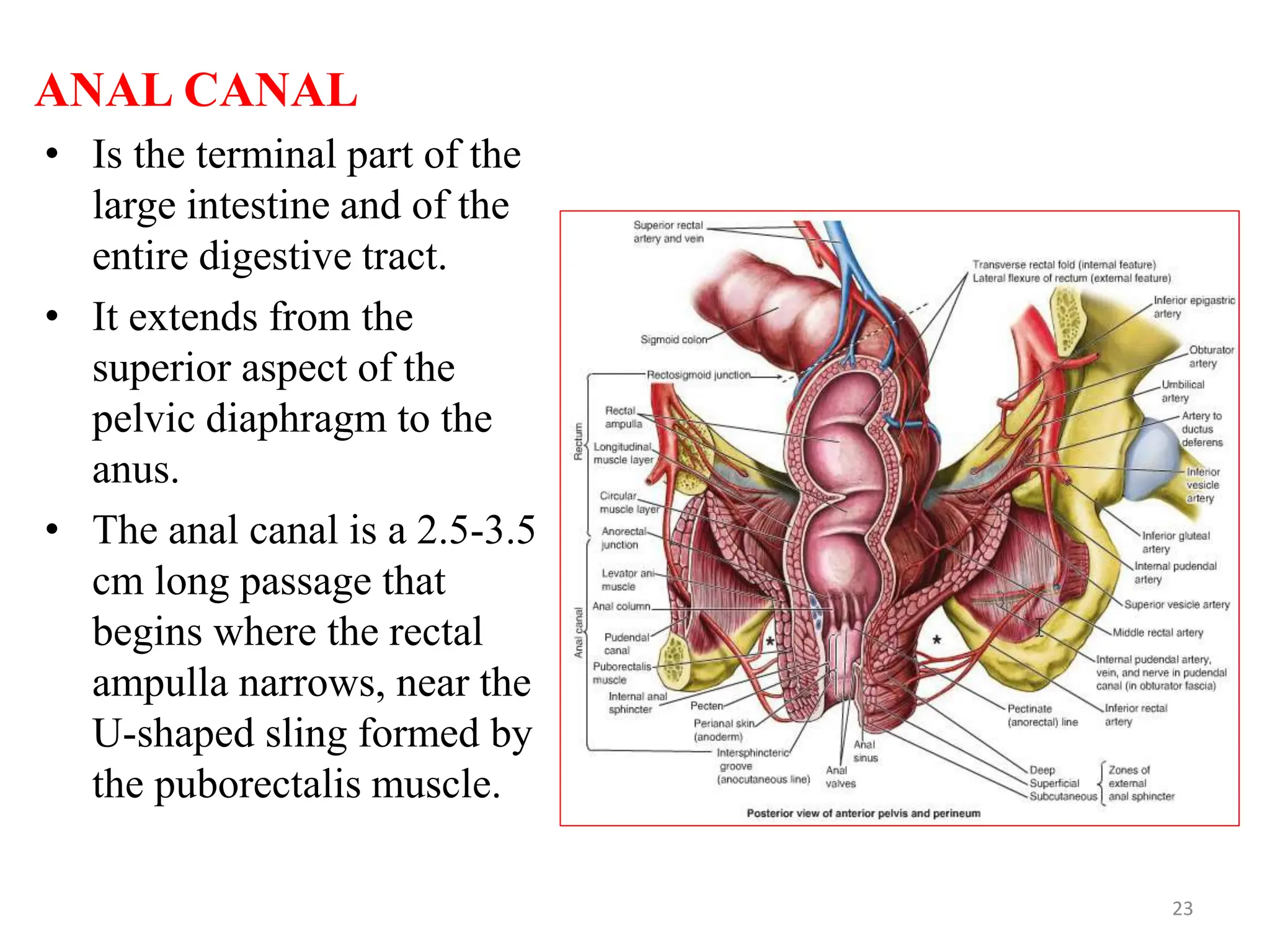
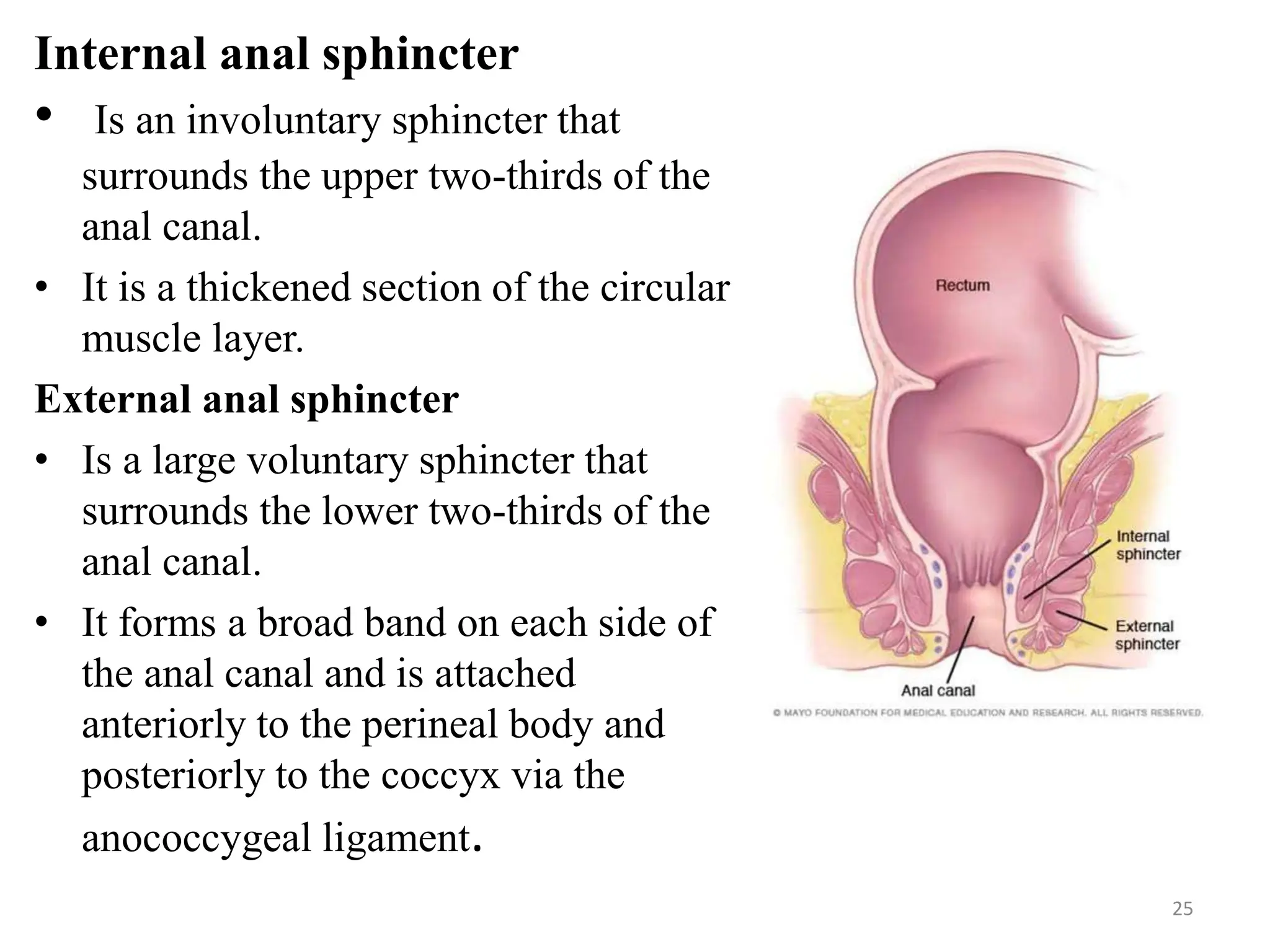
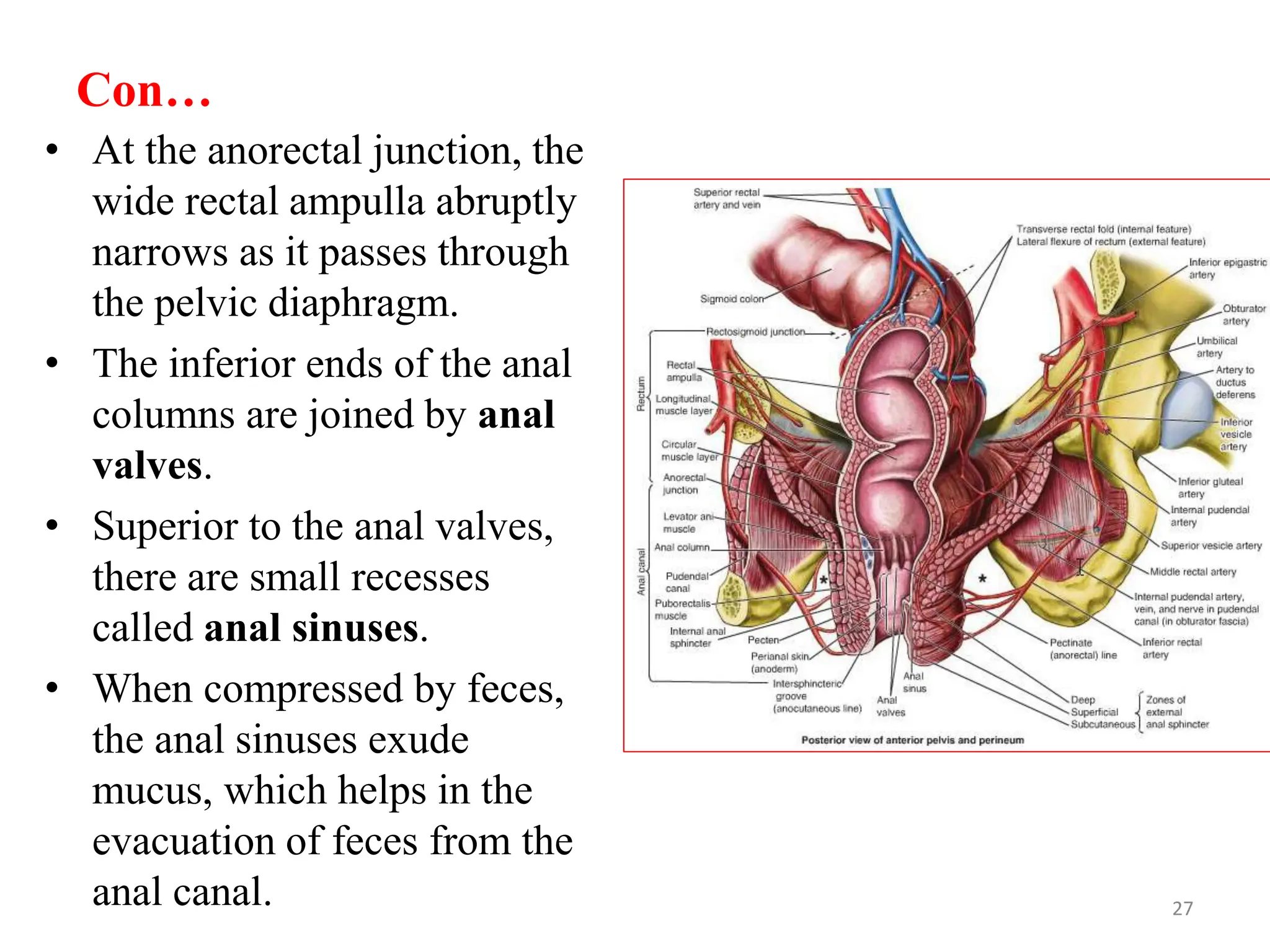
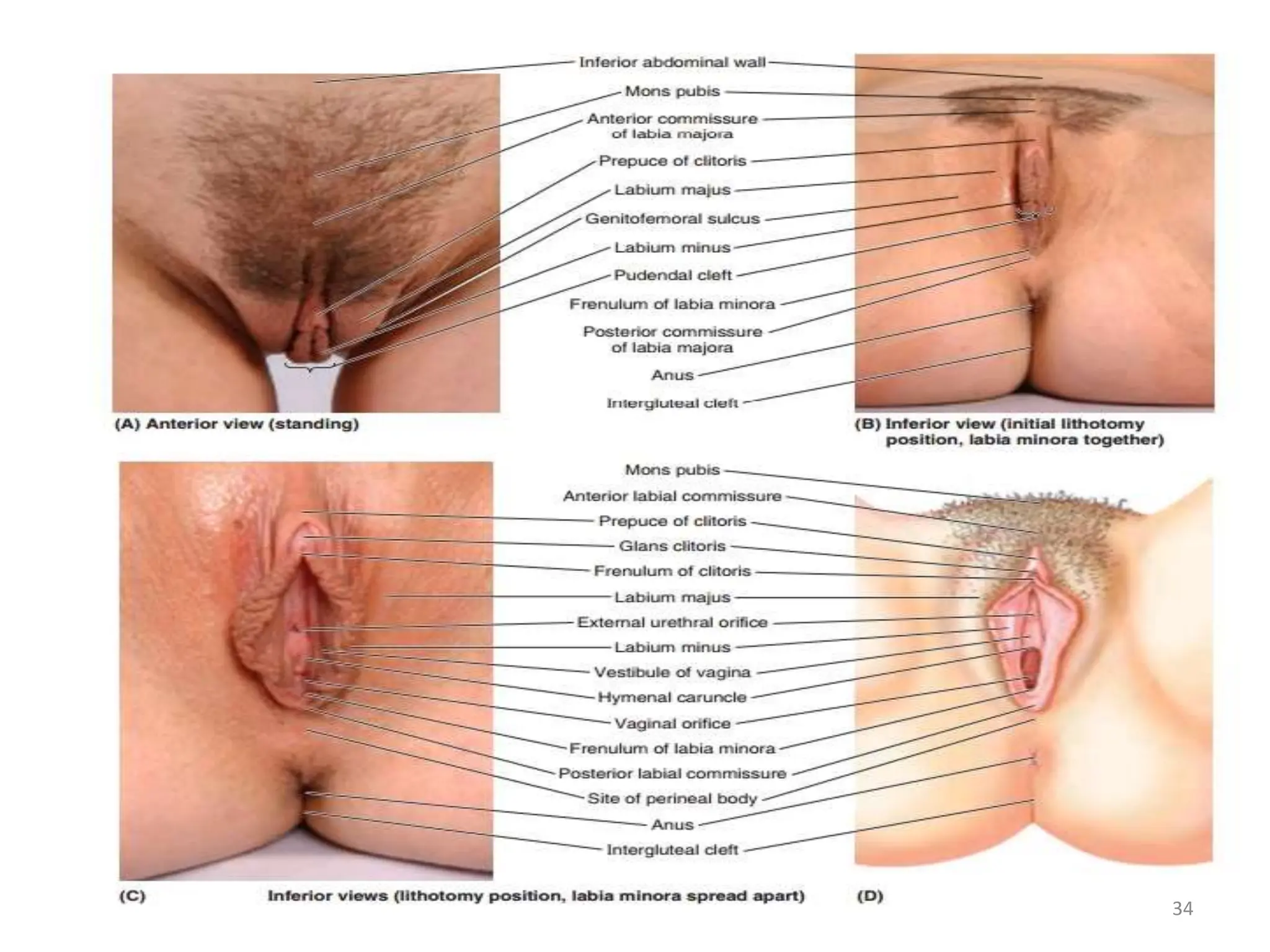
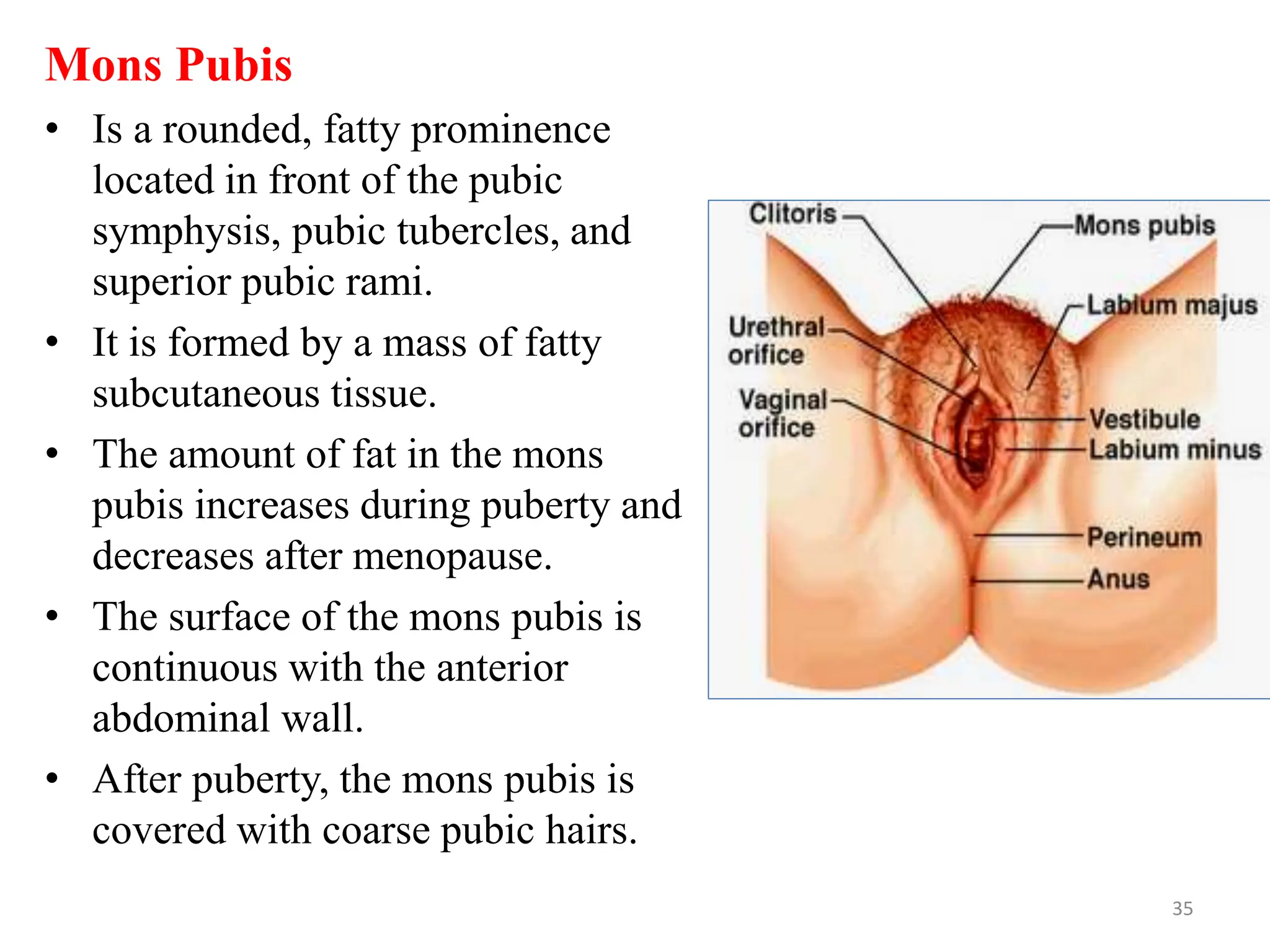
The document discusses the anatomy of the female perineum. It describes the boundaries and contents of the perineum, perineal body, urogenital diaphragm, and perineal pouches and fasciae. It also outlines the features of the anal triangle, including the ischio-anal fossae and pudendal canal. Finally, it covers the anatomy of the anal canal, internal and external anal sphincters, and their nerve and blood supply.