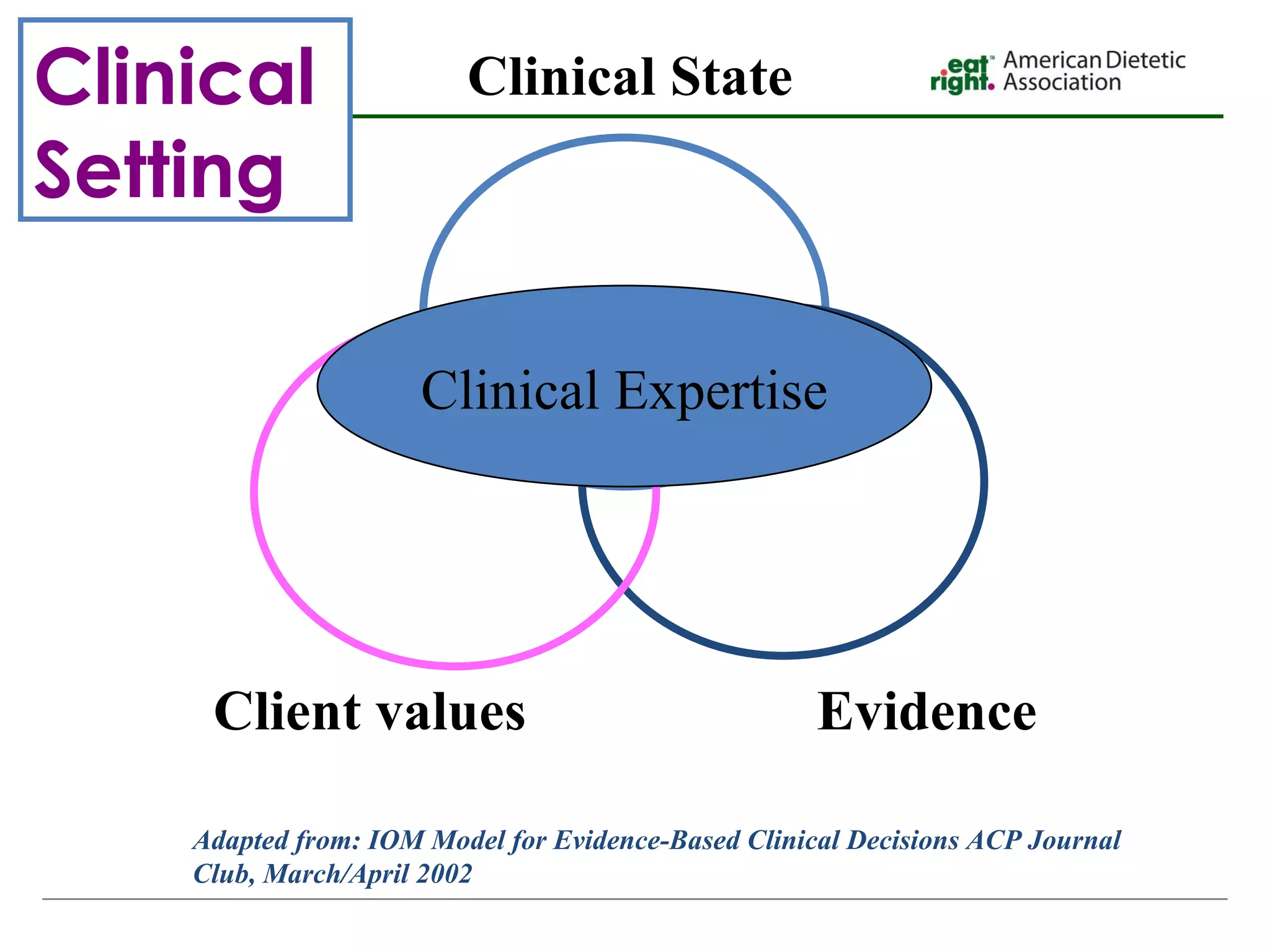
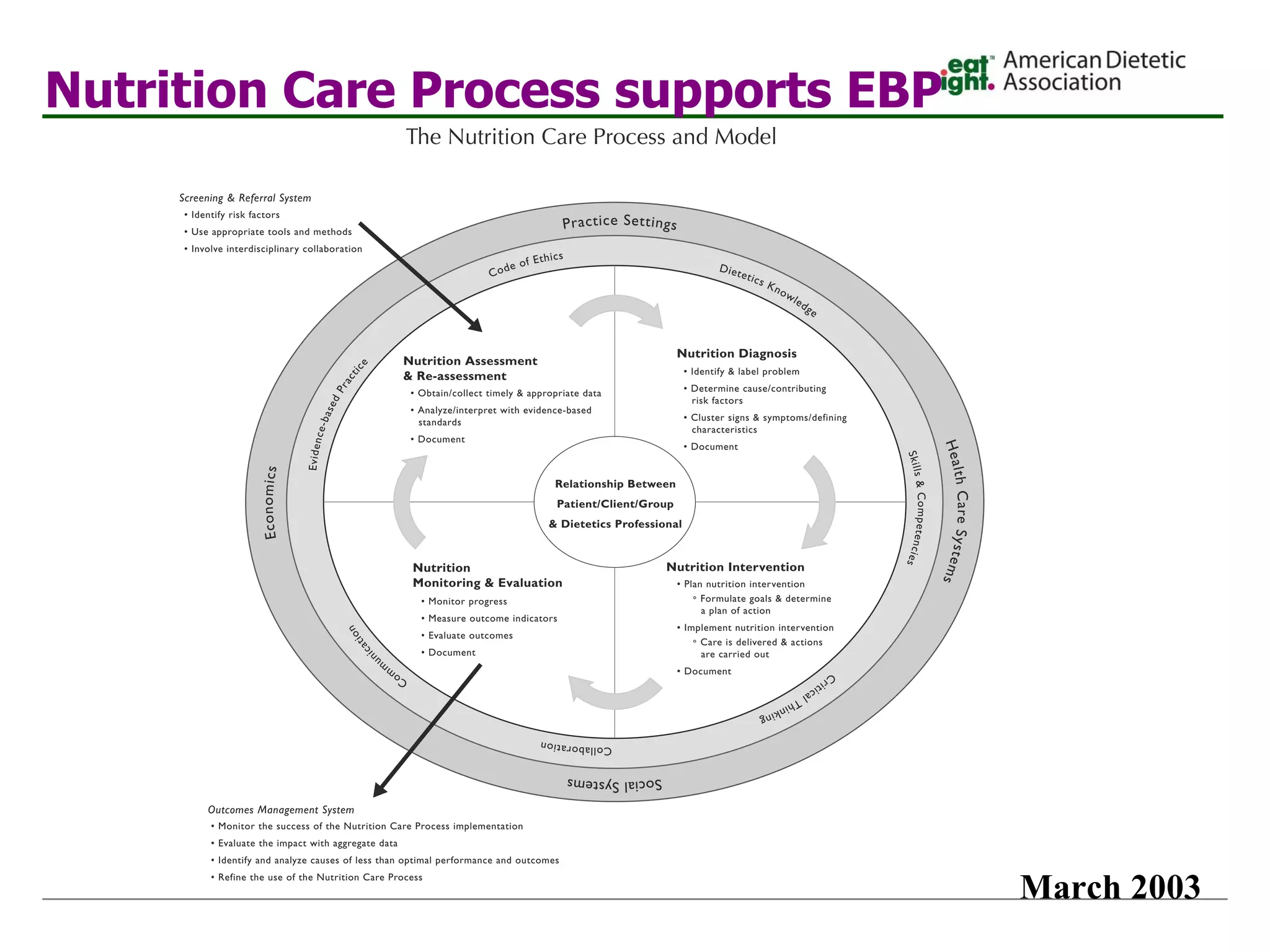
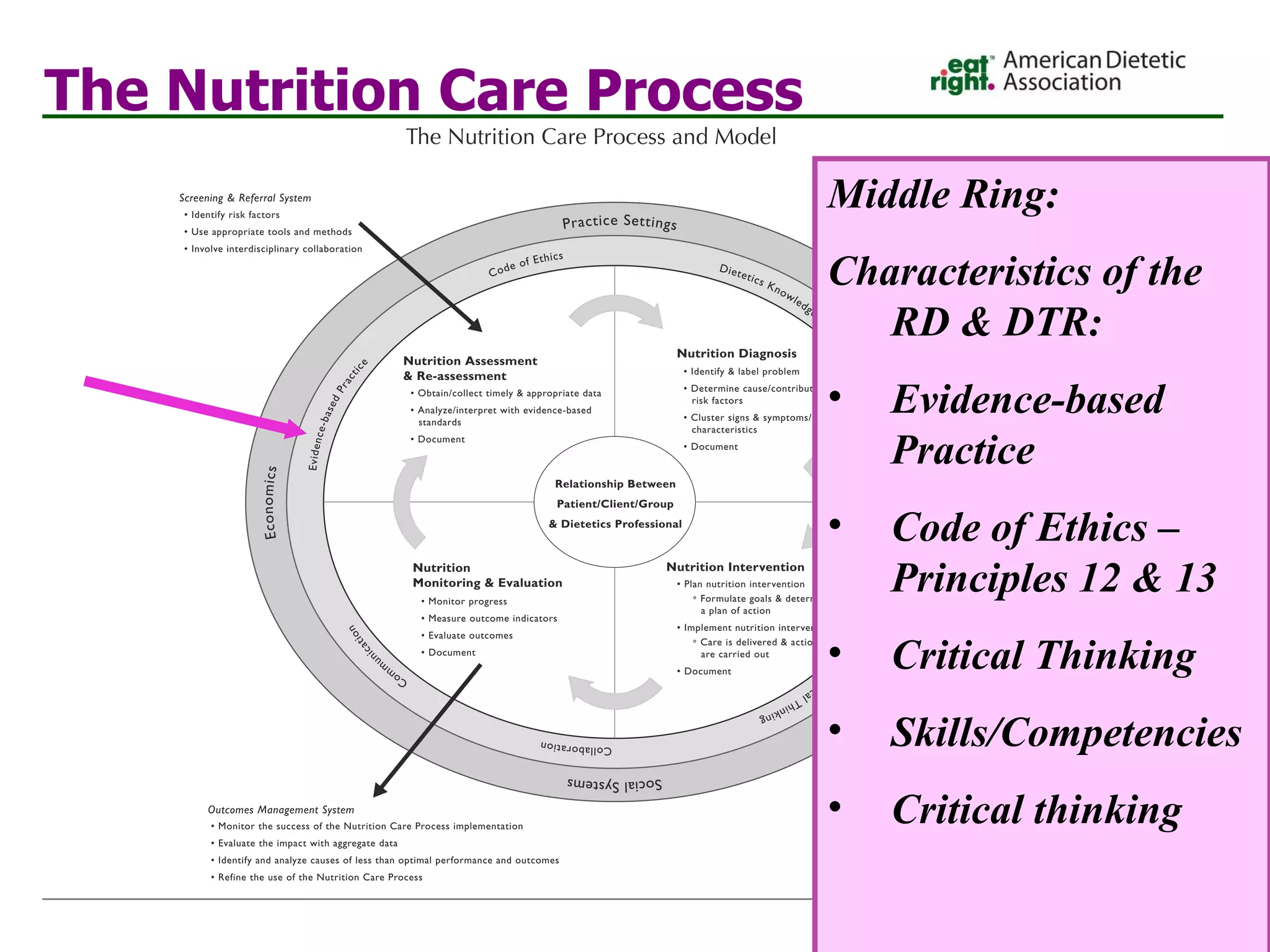
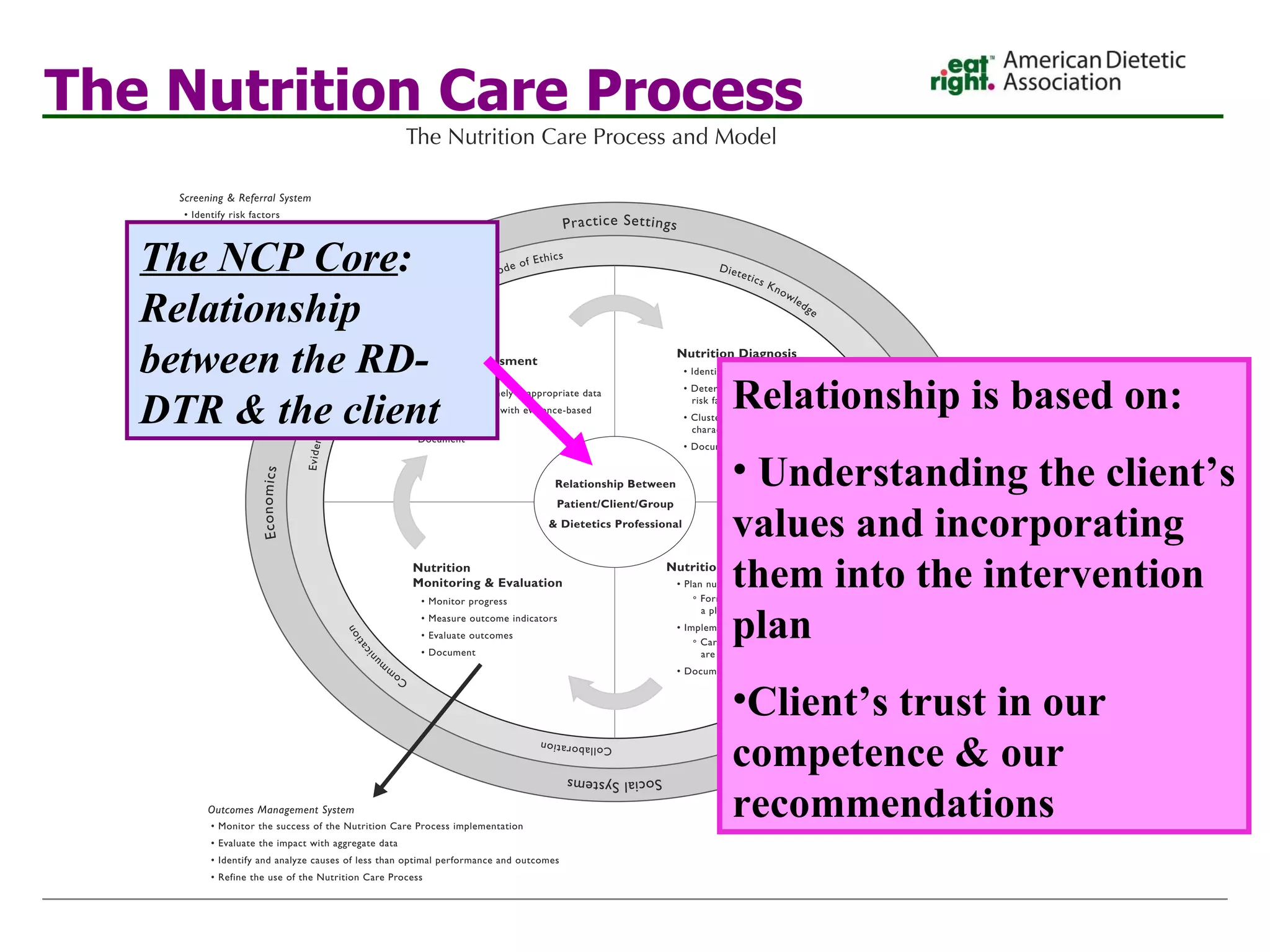
- Evidence-based practice uses systematically reviewed scientific evidence to make nutrition practice decisions by integrating best available evidence, professional expertise, and client values.
- Implementing evidence-based practice provides benefits like improved quality of care, increased patient safety, and enhanced professional status and confidence.
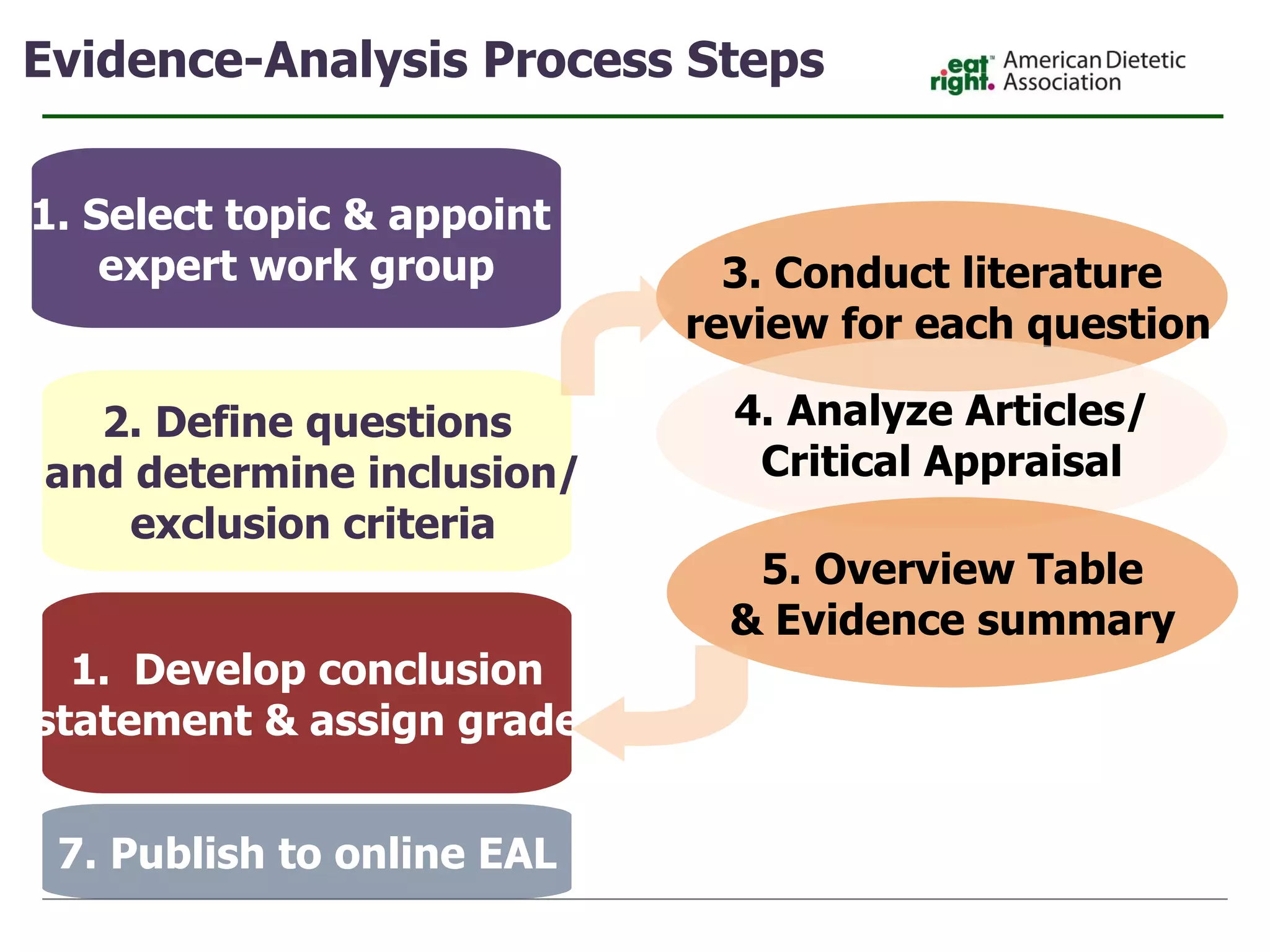
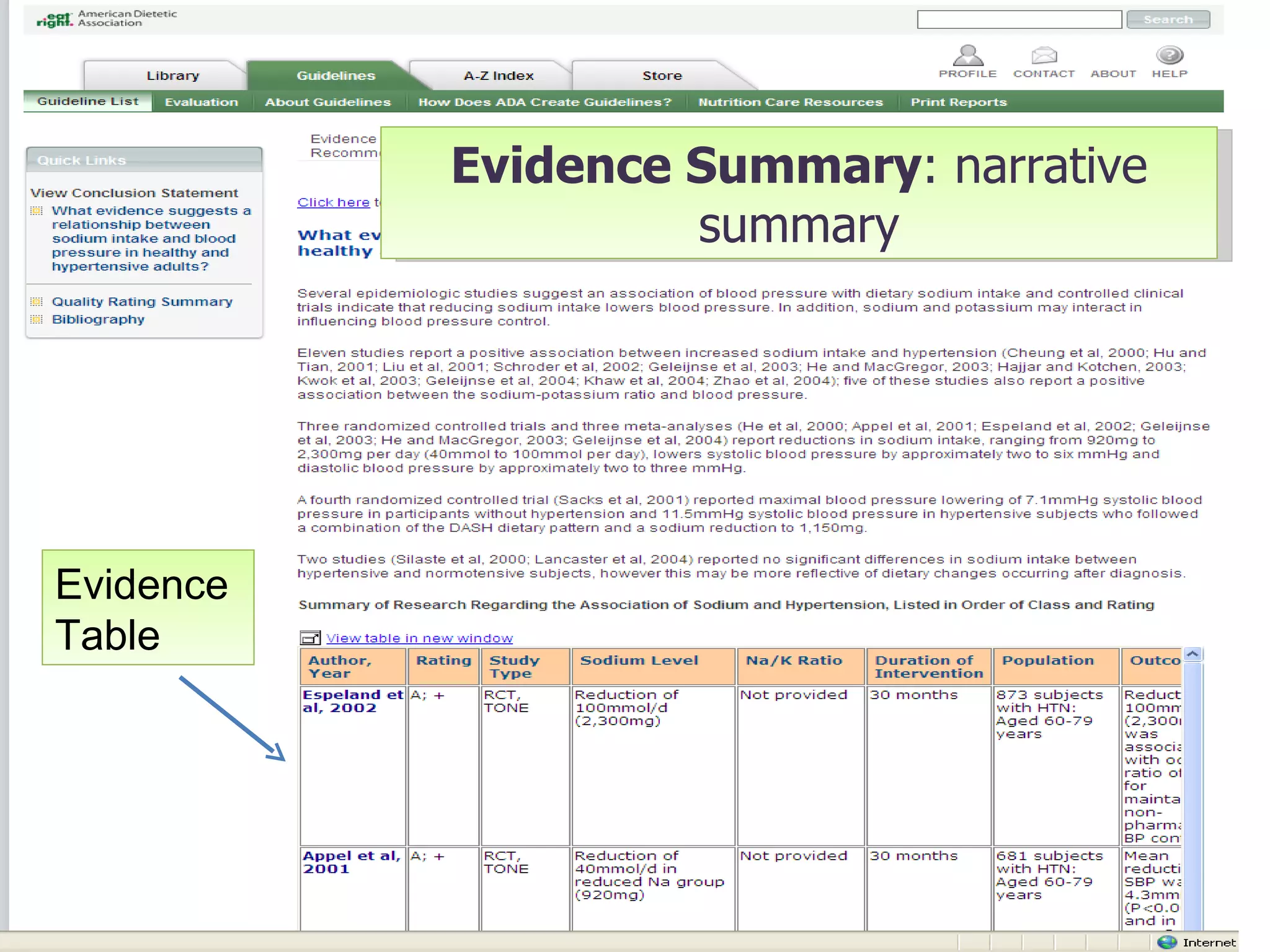
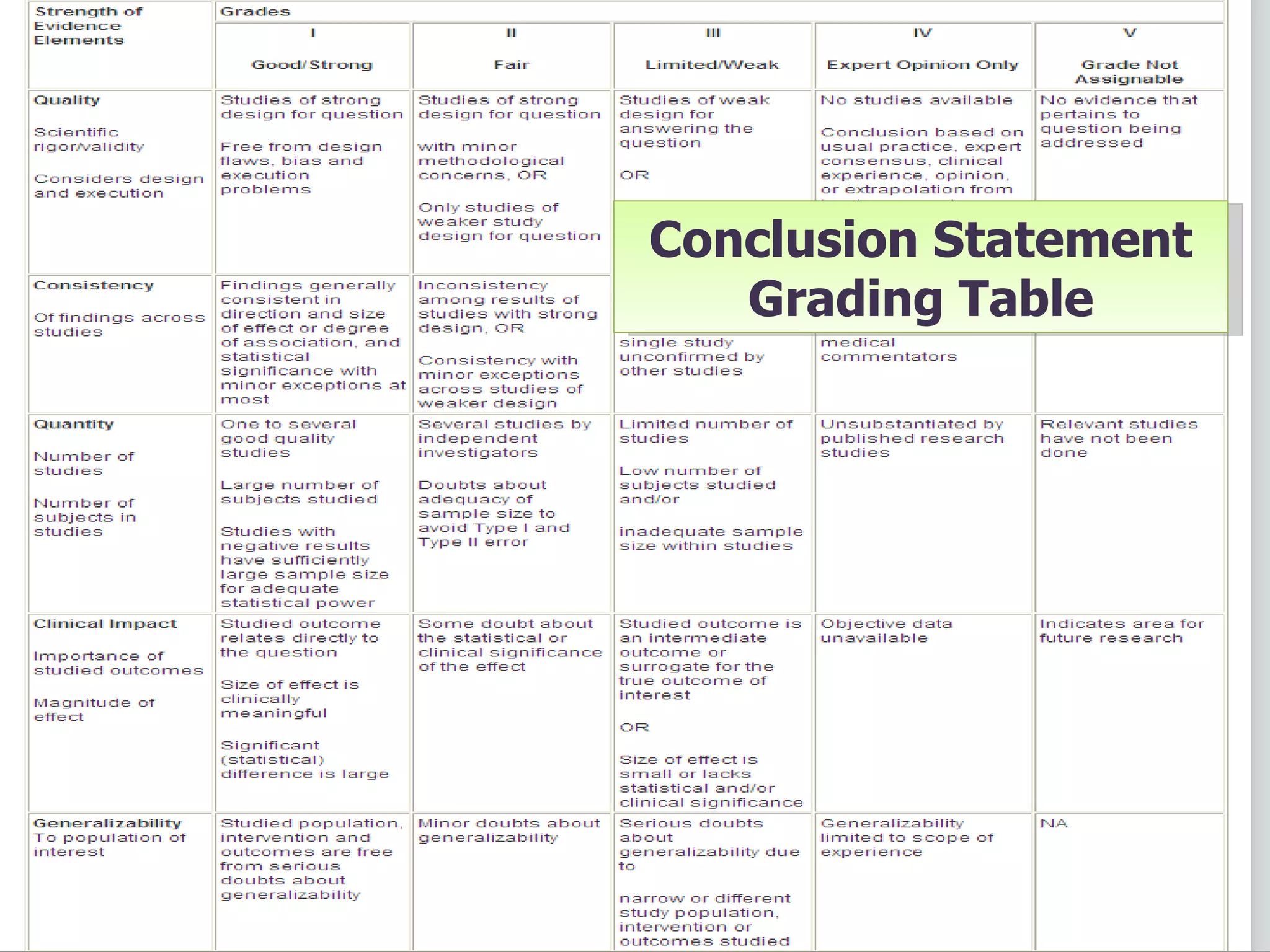
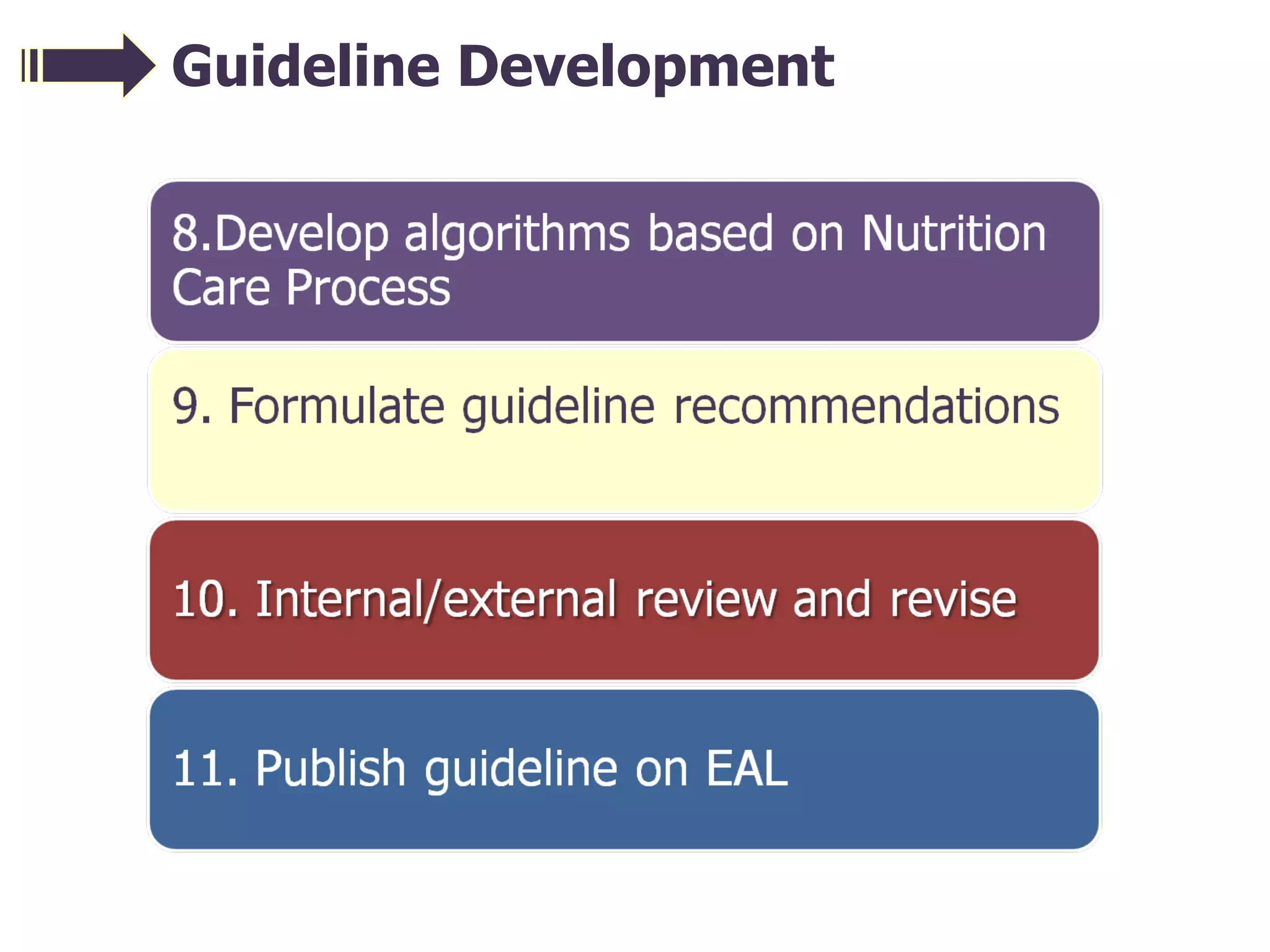
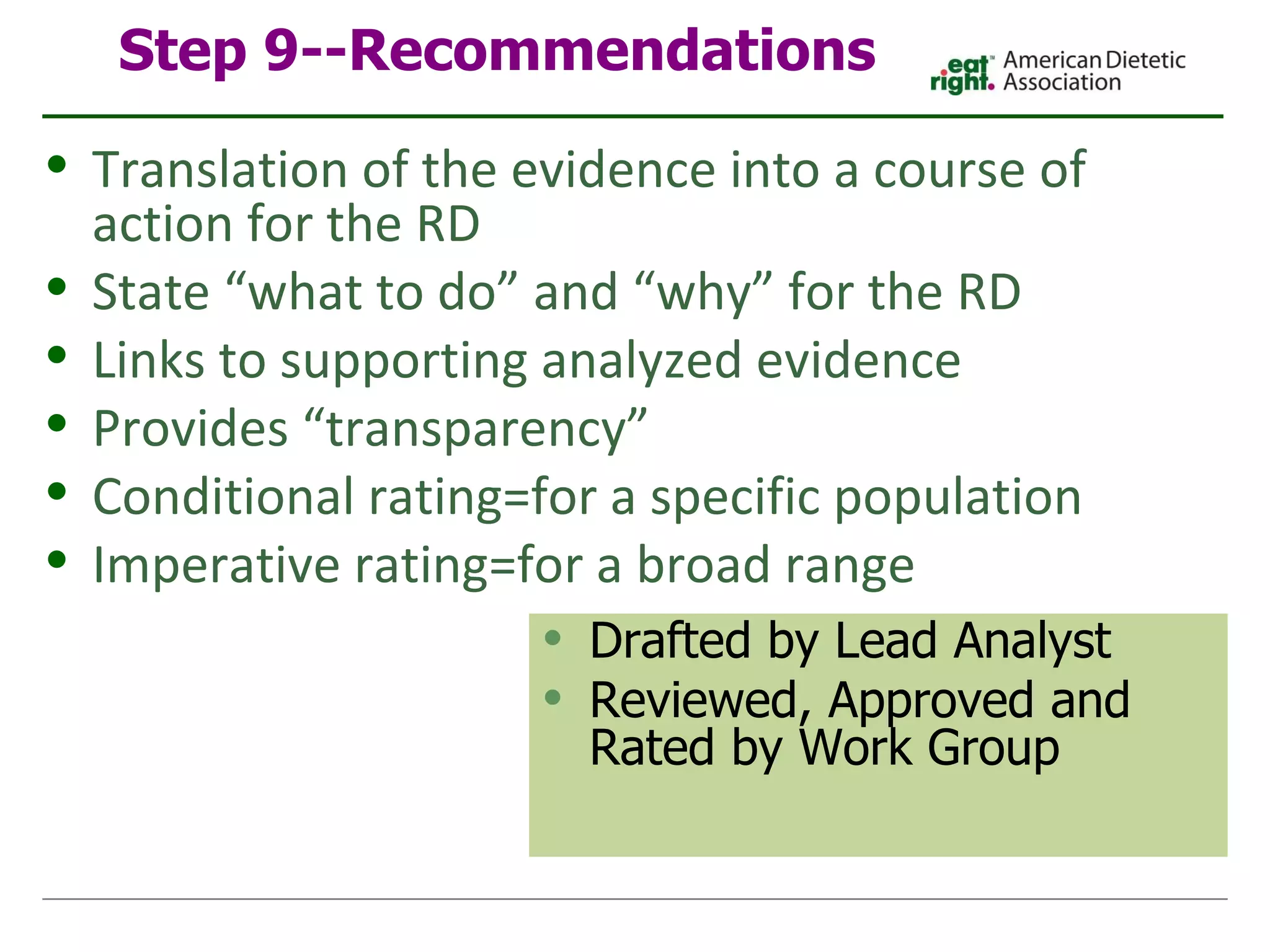
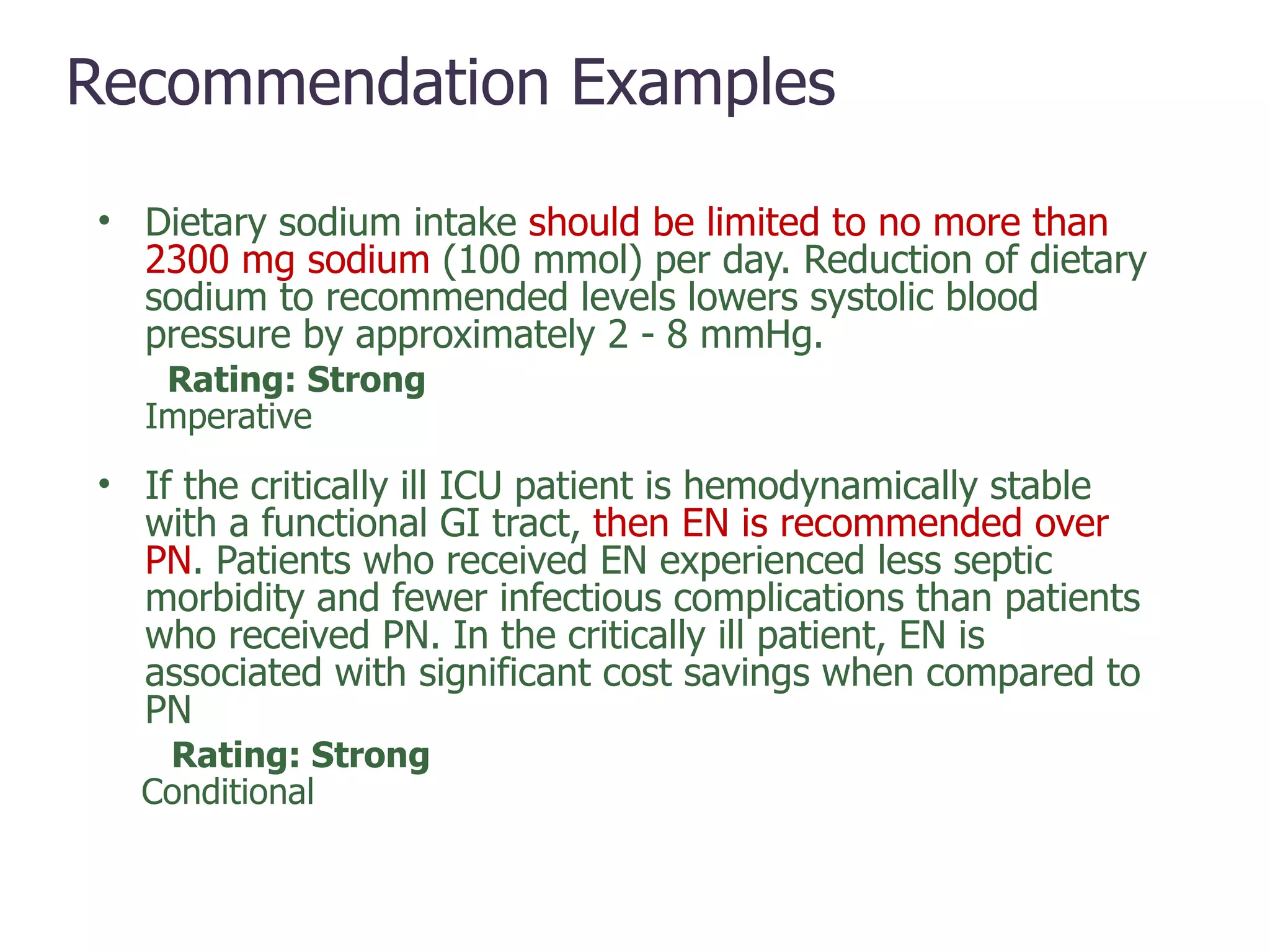
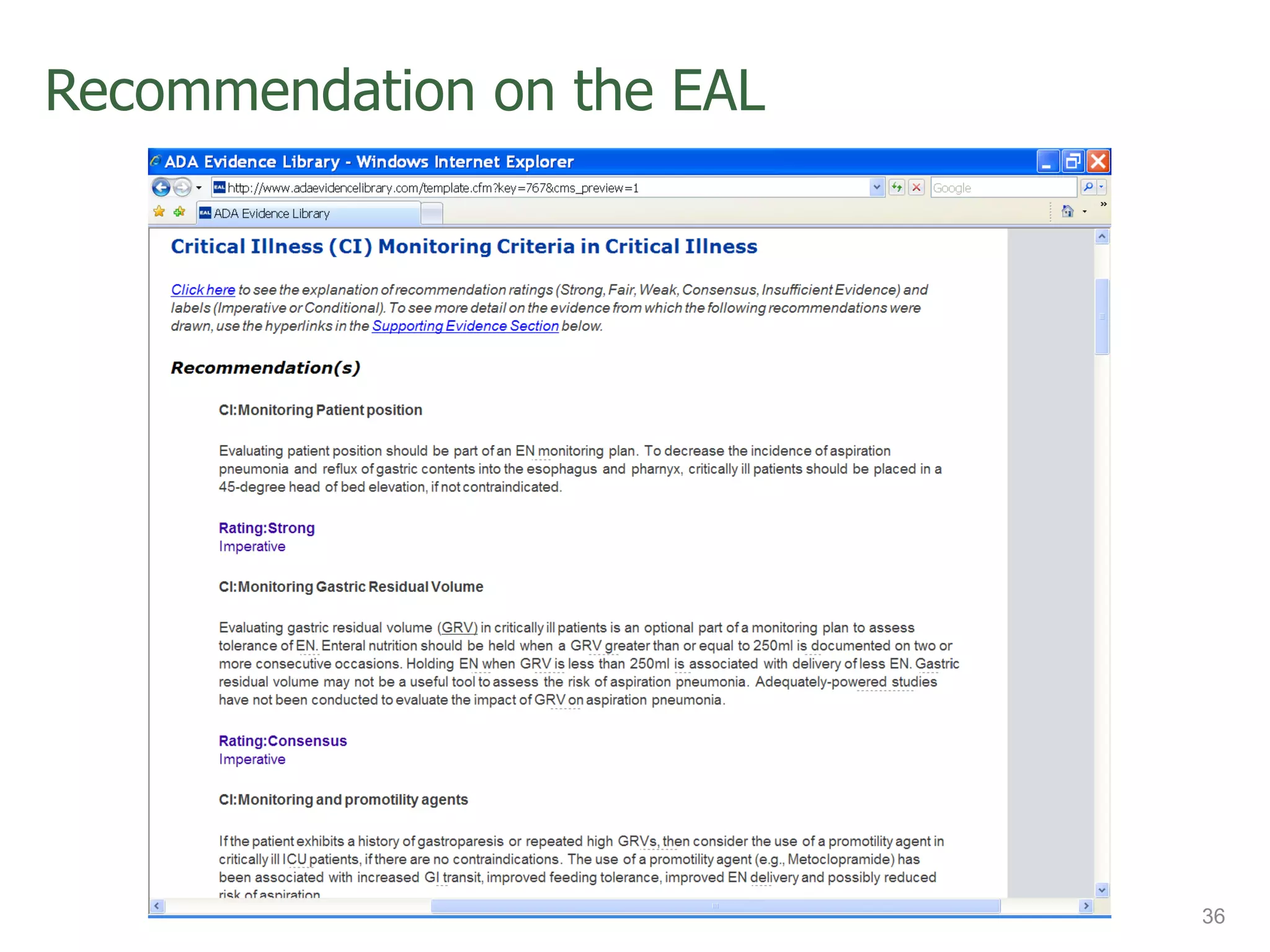
- The evidence-based practice process involves defining questions, reviewing literature, analyzing evidence, developing conclusions and recommendations, and disseminating results.
![Building Evidence-Based Practice into All Areas of Dietetics Linda Farr RD/LD TDA Delegate 2007-2012 Owner Nutrition Associates of San Antonio 210-735-2402 [email_address]](https://image.slidesharecdn.com/10-12935564023163-phpapp02/75/Evidence-Based-Practice-in-All-1-2048.jpg)

![Evidence Analysis Training Workshops VOLUNTEERS NEEDED! If you know someone who is interested in becoming an evidence analyst, please ask them to submit an application. If you have questions, contact Toni Acosta at [email_address] .org Benefits: Professional Development Professional Exposure Continuing Education Hours](https://image.slidesharecdn.com/10-12935564023163-phpapp02/75/Evidence-Based-Practice-in-All-52-2048.jpg)