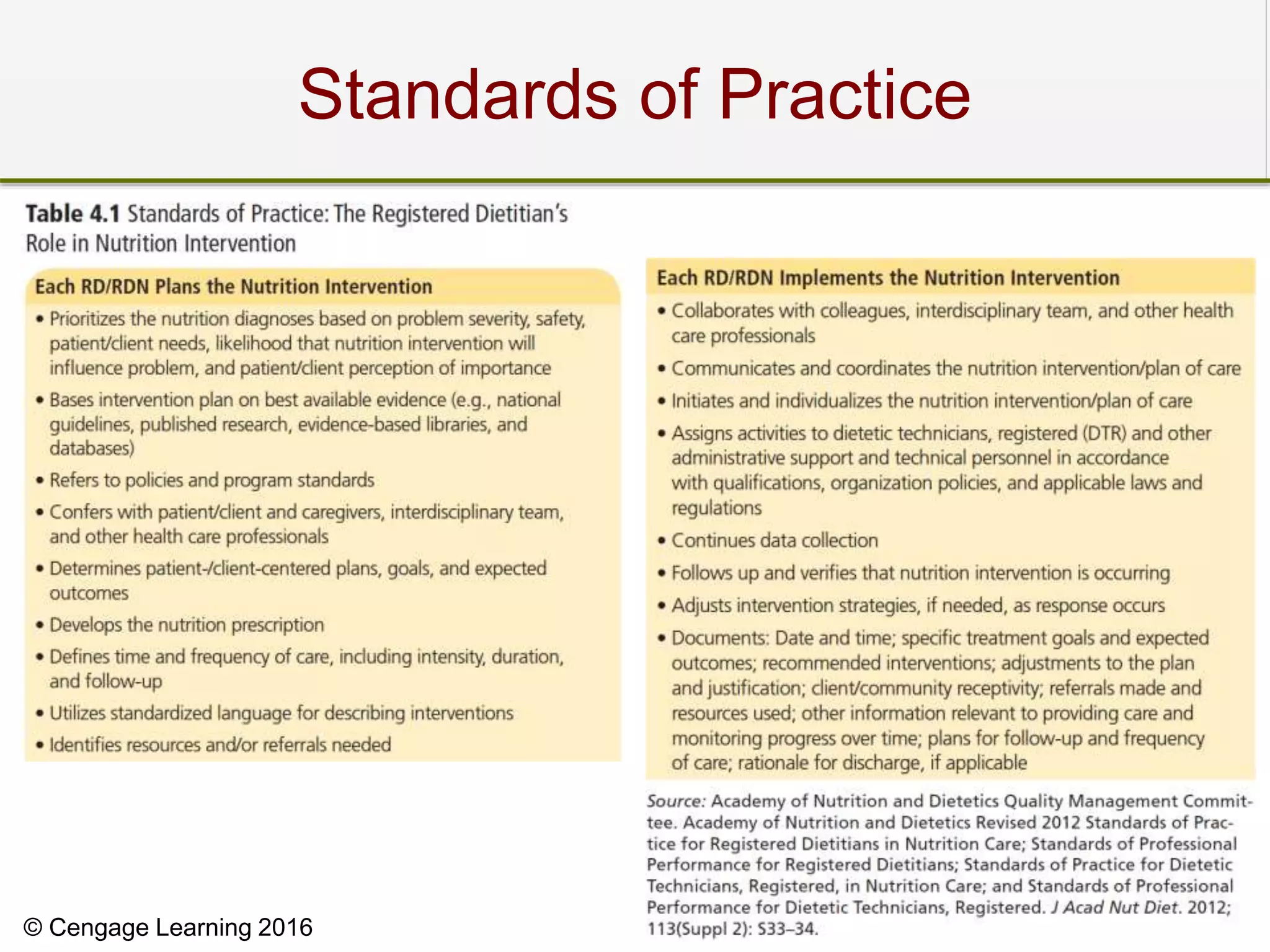
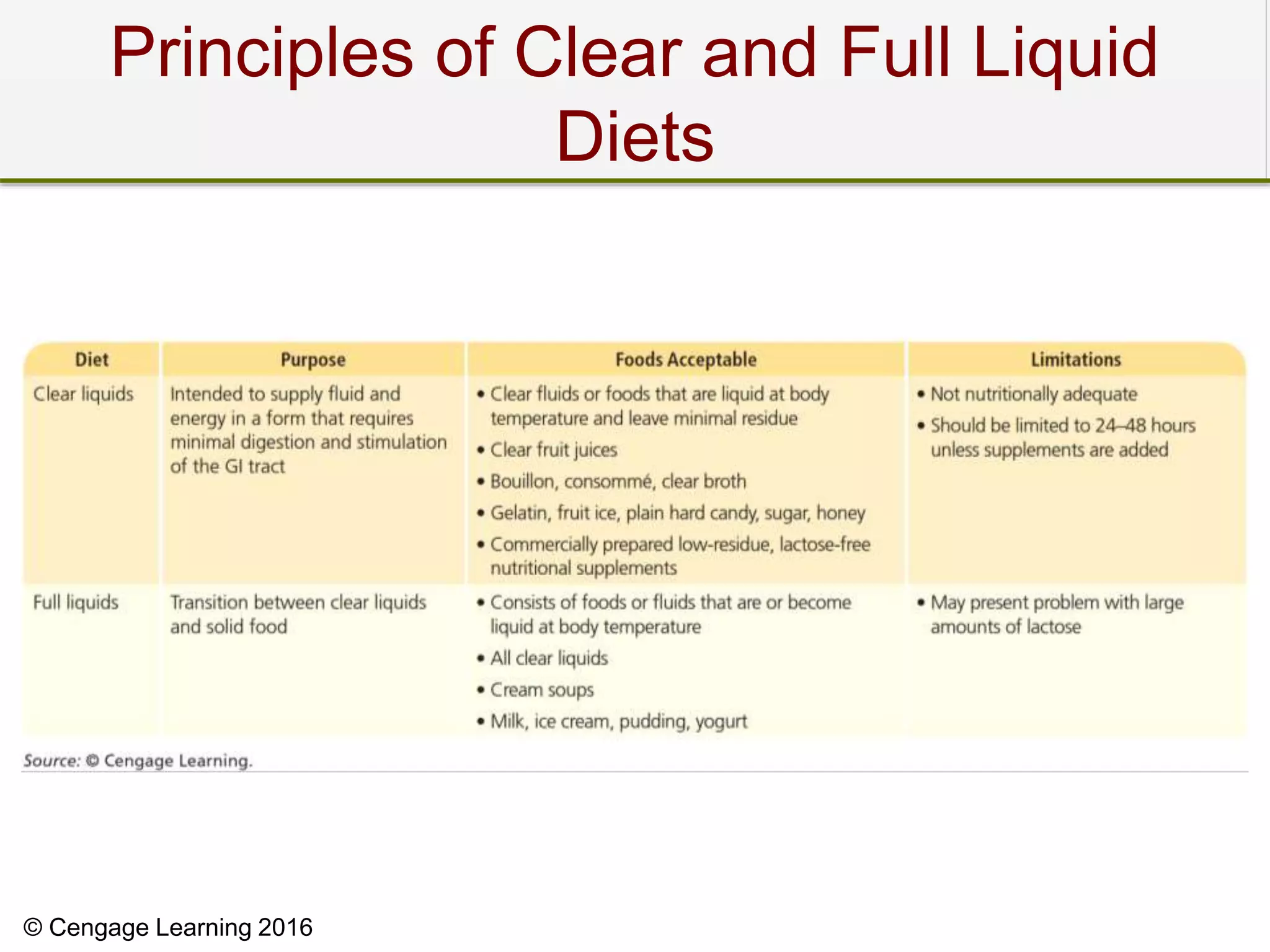
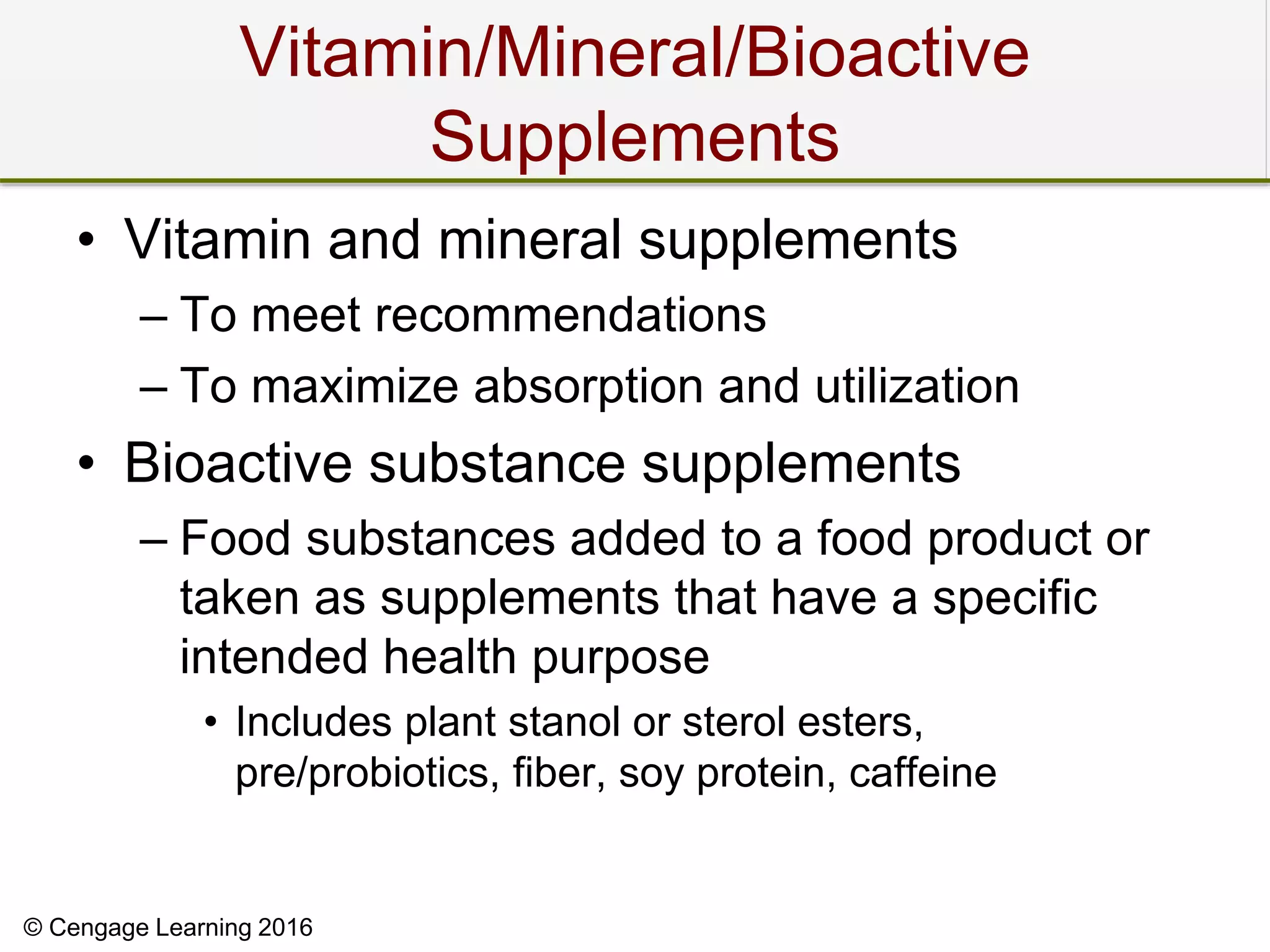
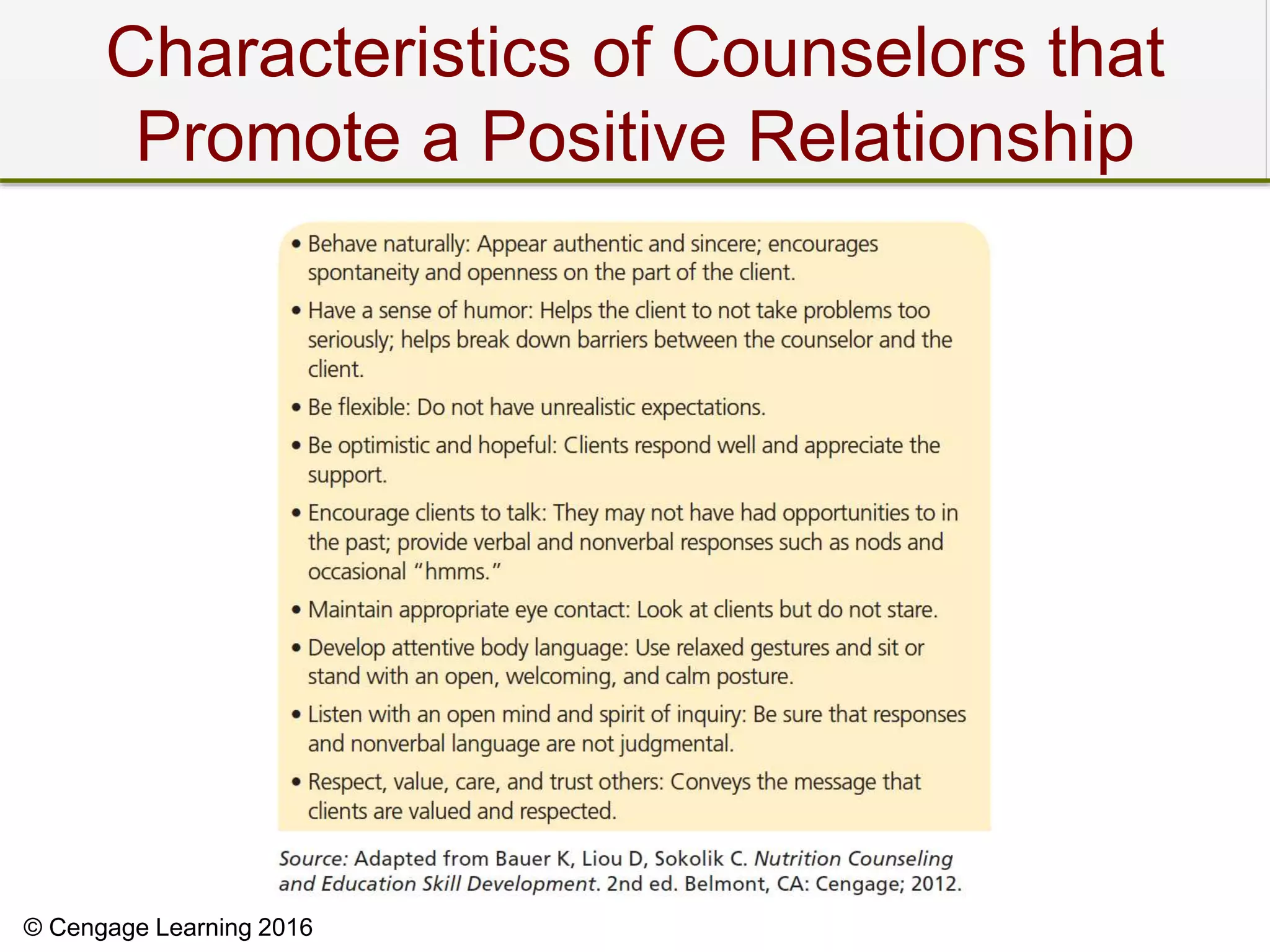
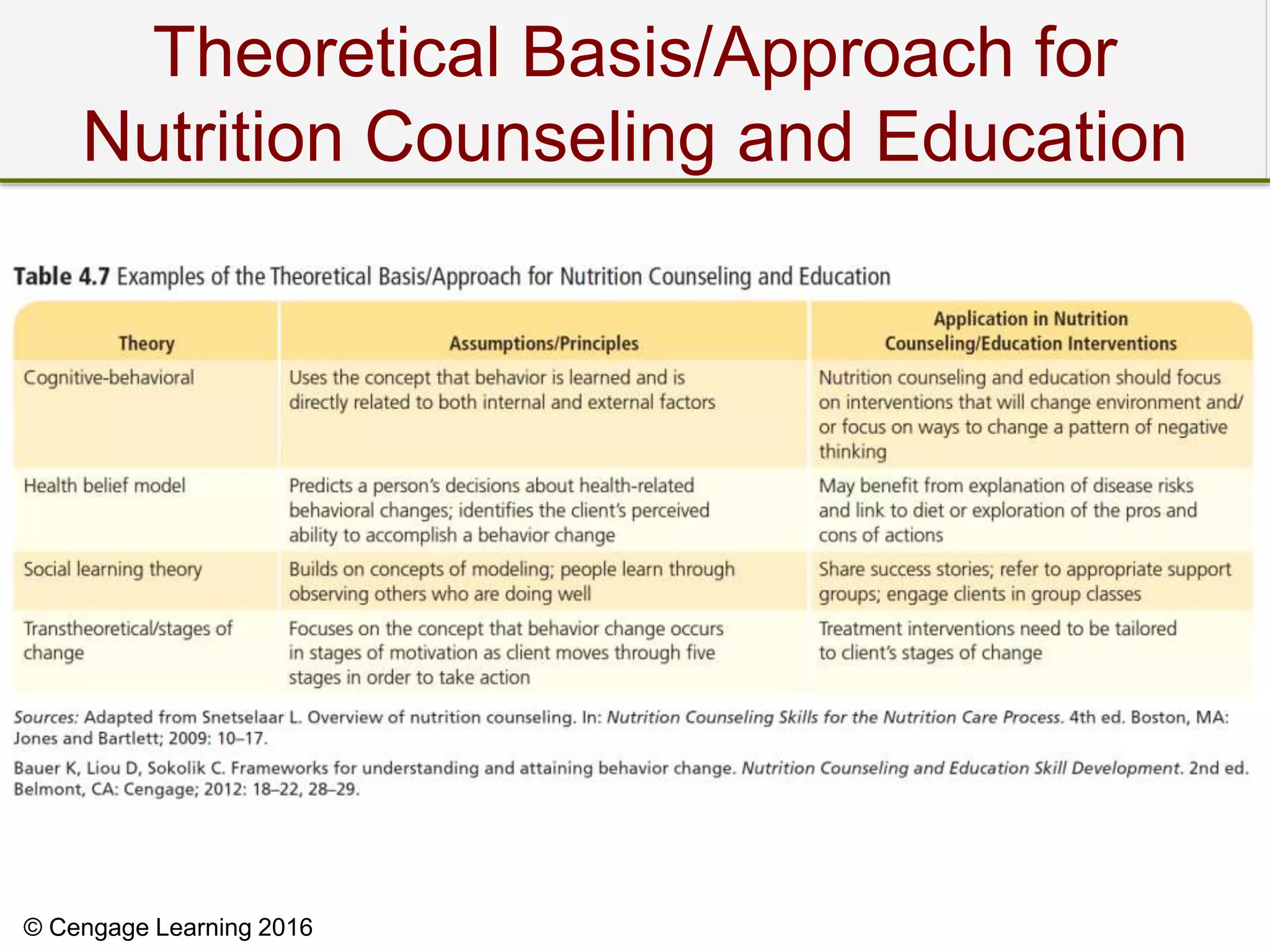
This document discusses various nutrition interventions including nutrition prescriptions, oral diets, modifications to regular diets, clear and full liquid diets, increasing nutrient density, supplements, feeding assistance, medication management, education, counseling, coordination of care, and monitoring and evaluation. The interventions are based on standards of practice and aim to best meet individual nutritional needs based on diagnoses and conditions. Counseling focuses on developing collaborative and individualized plans to help patients take responsibility for behaviors.