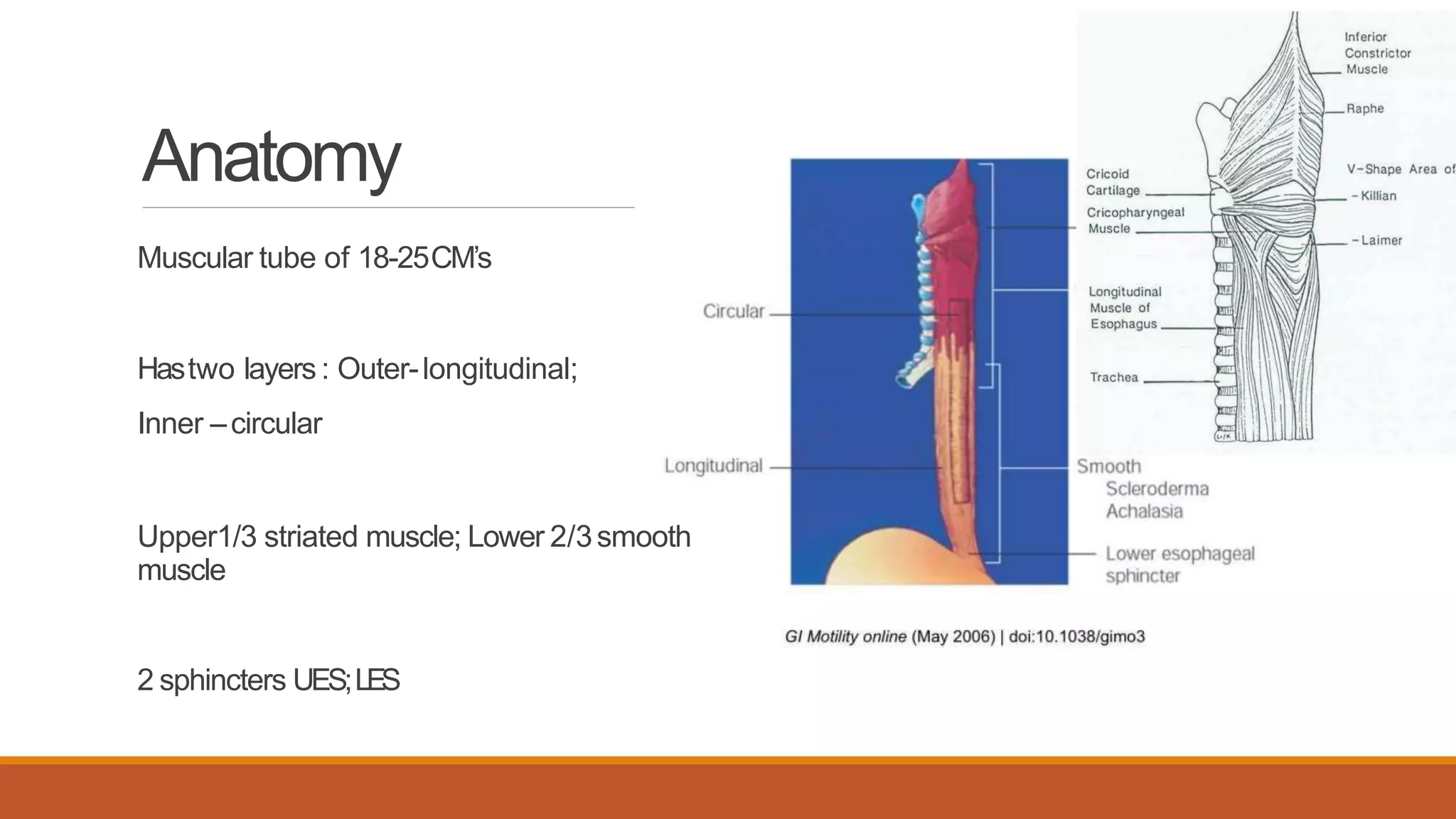
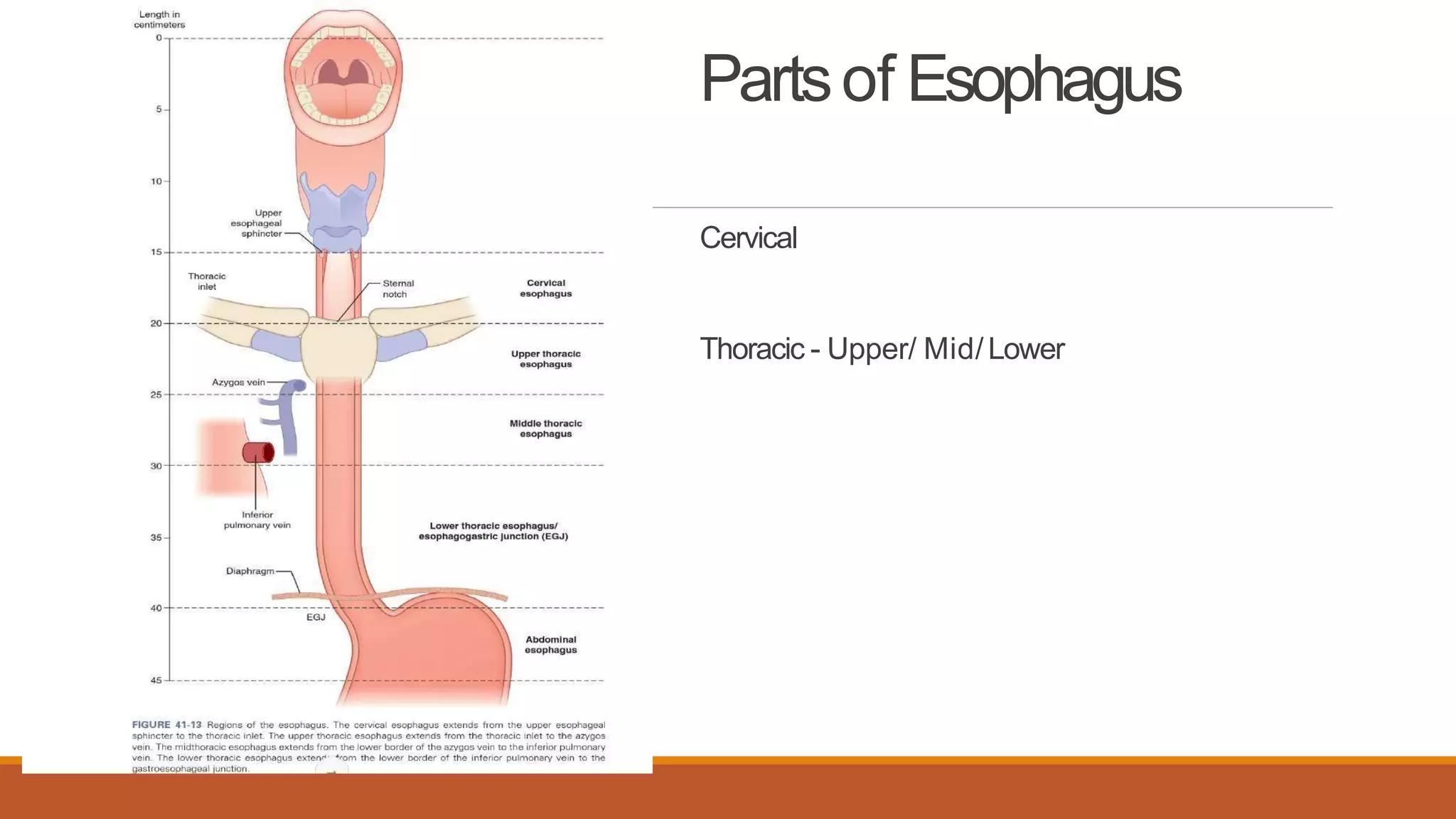
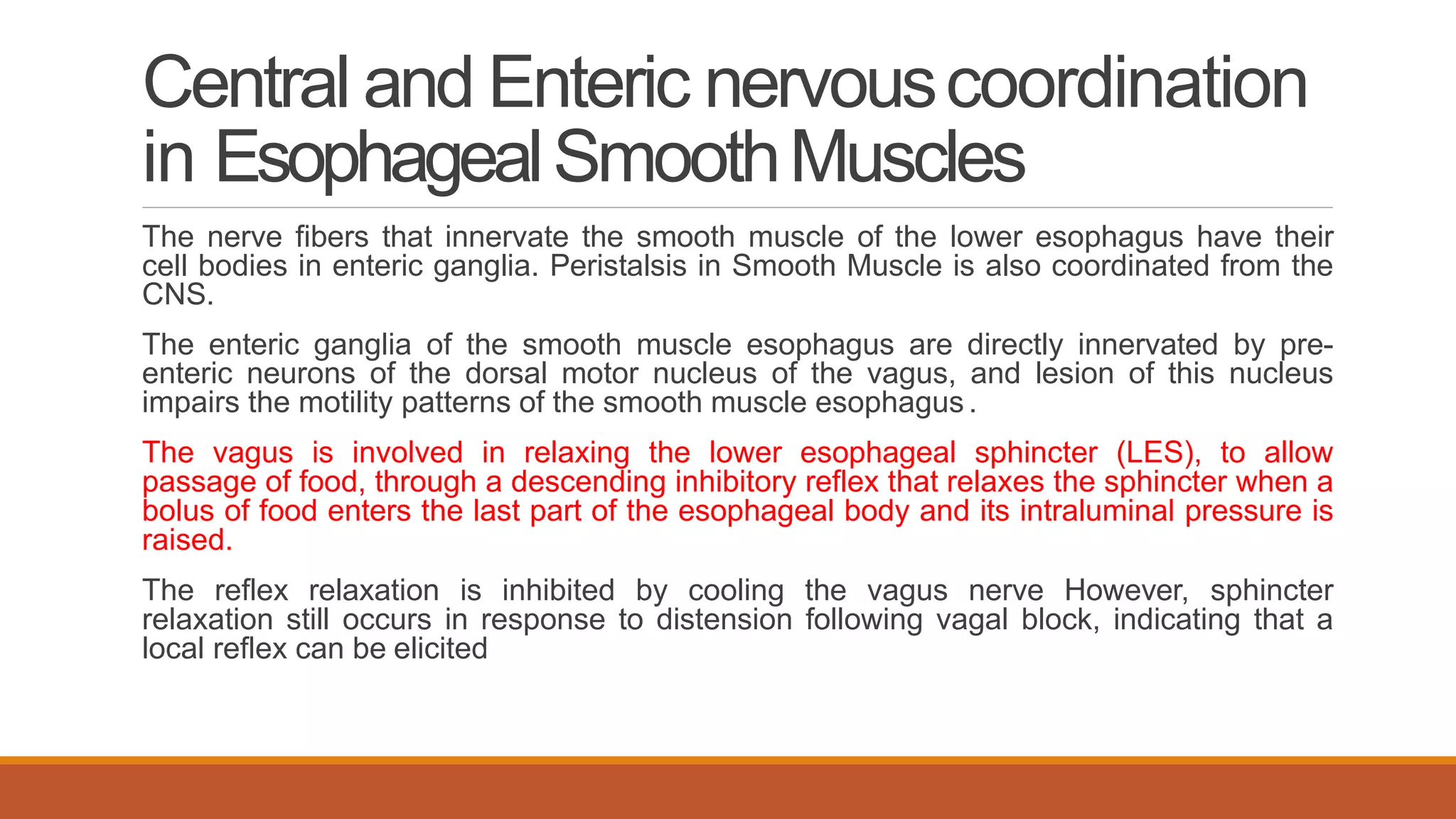
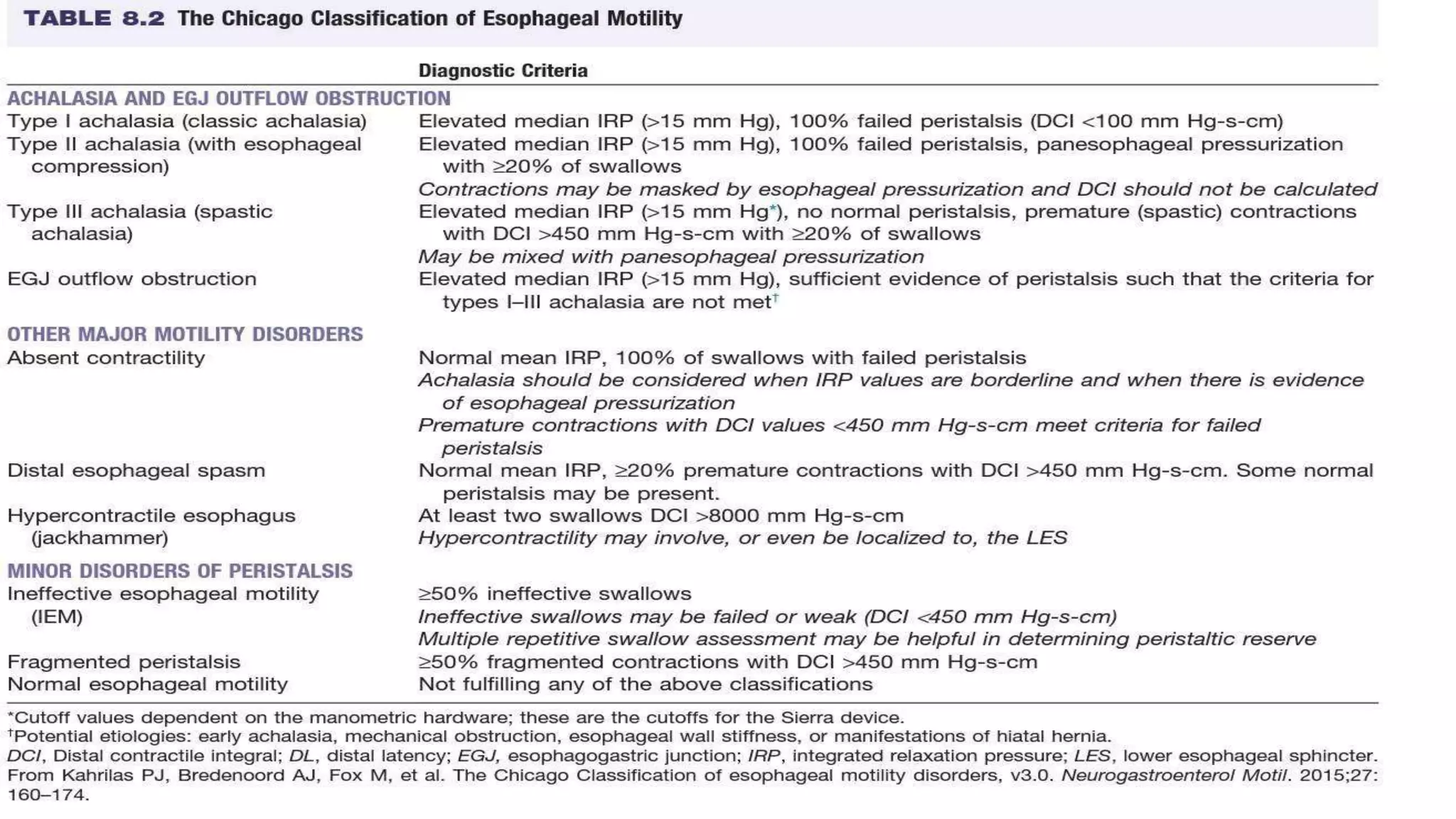
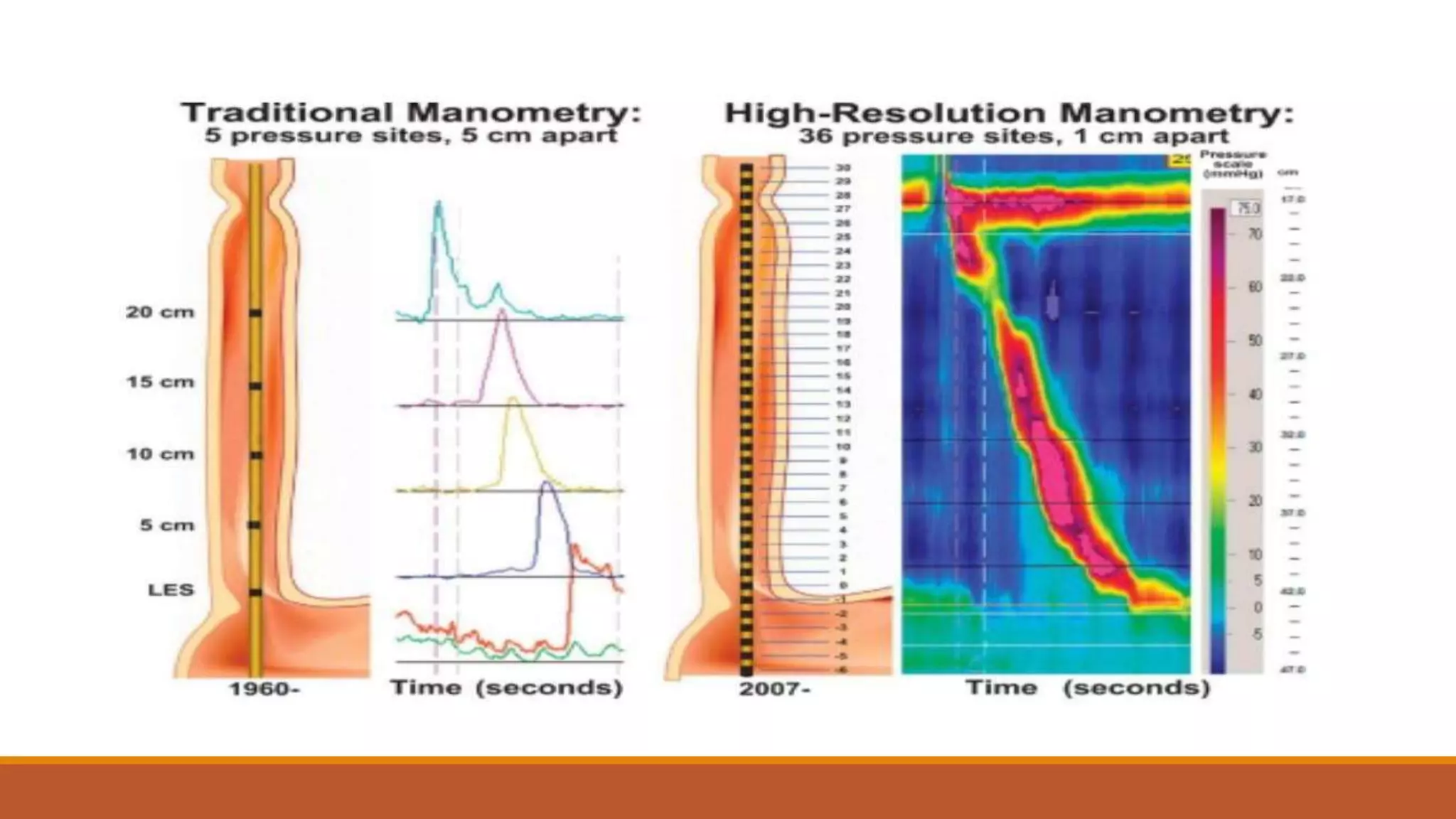
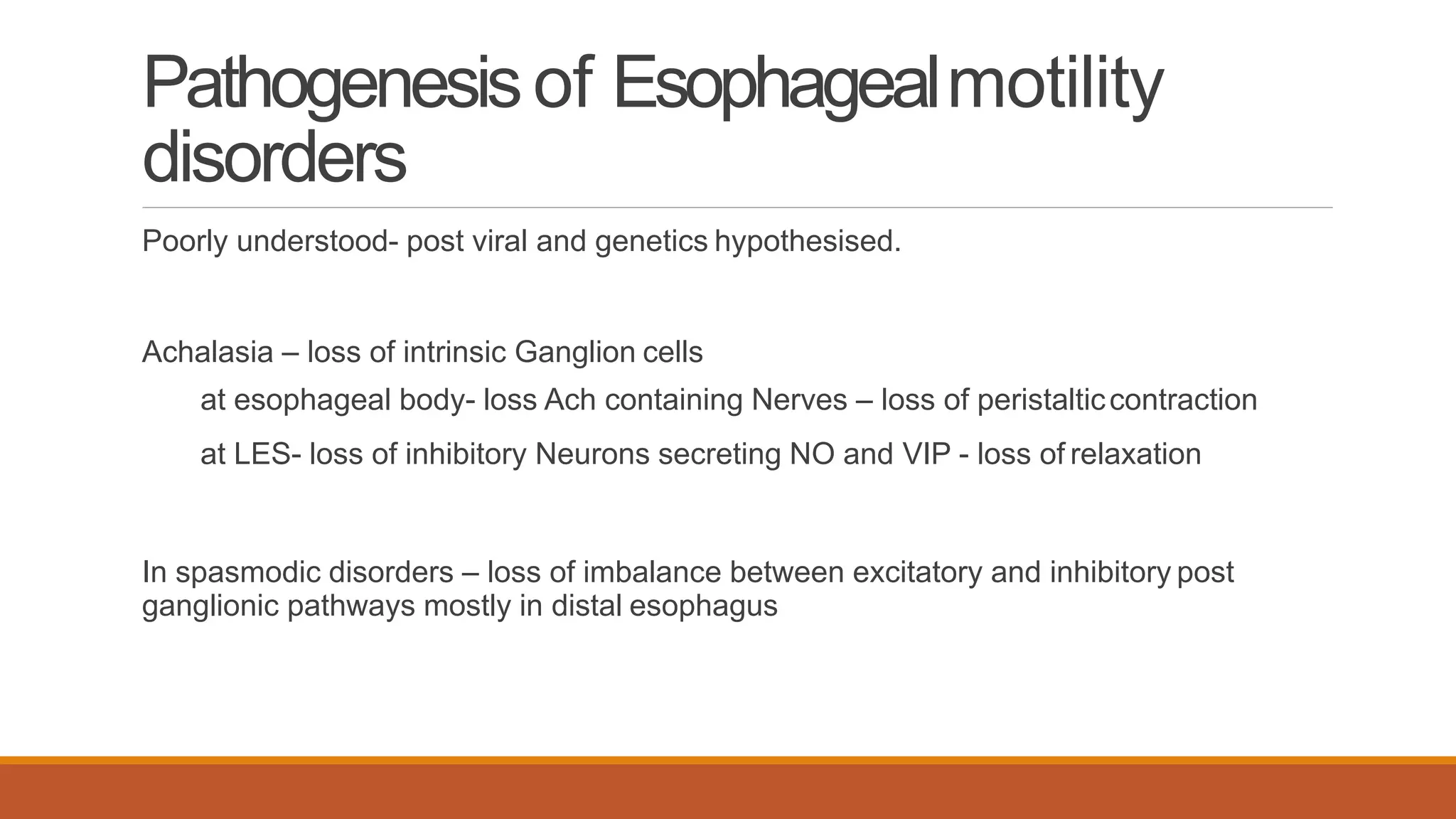
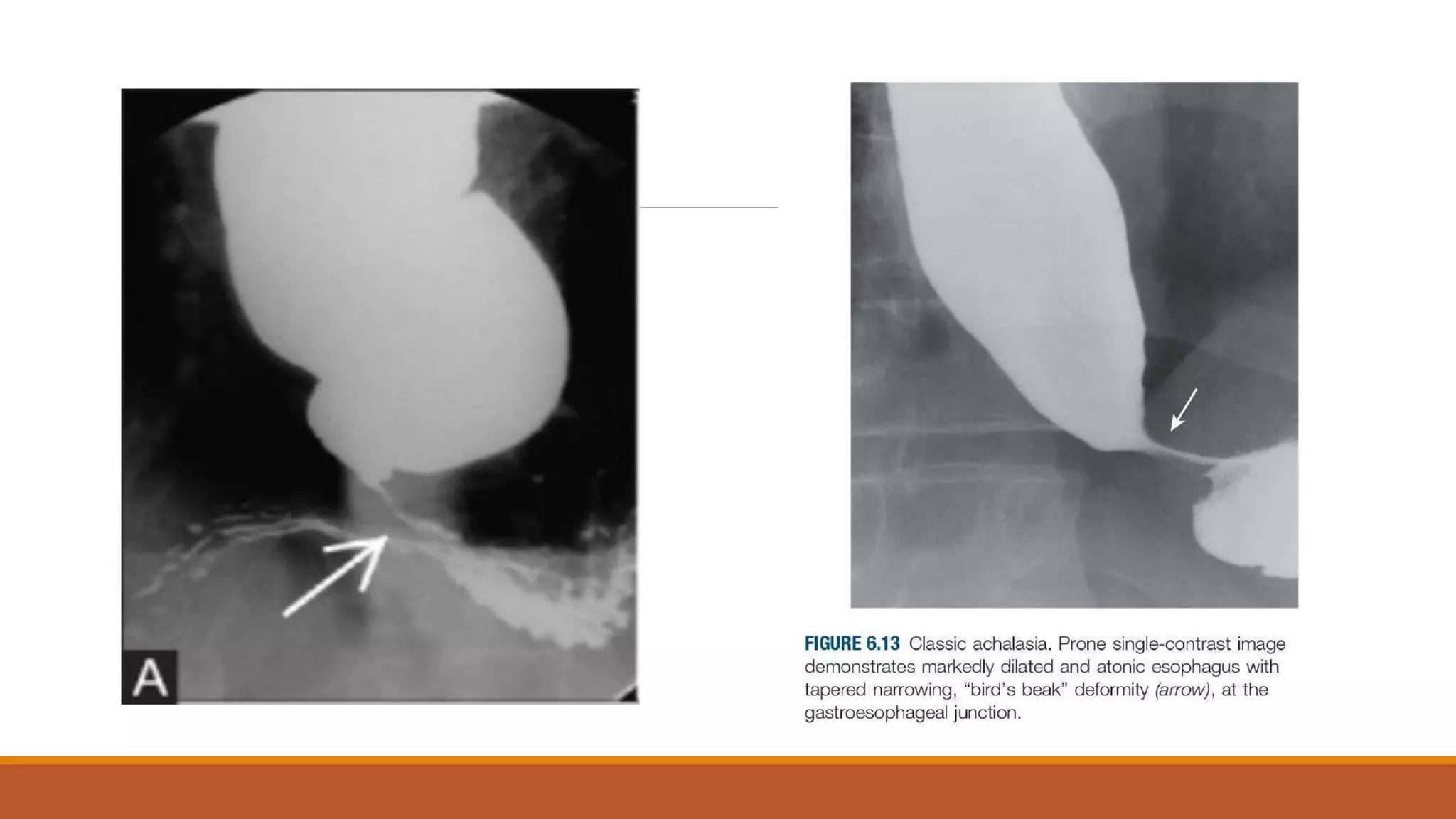
This document provides an overview of esophageal motility disorders. It describes the anatomy and physiology of normal esophageal function, including peristalsis. Esophageal motility disorders are classified as either relaxation disorders like achalasia or contraction disorders. Achalasia is characterized by impaired LES relaxation and absent peristalsis. It can be classified into 3 subtypes based on manometry findings. Treatment involves medications, botulinum toxin injections, or pneumatic dilatation of the LES. Manometry, particularly high-resolution manometry, is the gold standard for diagnosing esophageal motility disorders.














































![ClinicalFeatures
Progressive dysphagia to both solids and liquids is the most common presenting
symptom (90%),
followed by regurgitation of undigested food (76% to 91%),
respiratory complications (nocturnal cough [30%] and aspiration [8%]),
chest pain (25% to 64%),
heartburn (18% to 52%), and
weight loss (35% to 91%)](https://image.slidesharecdn.com/esophagealmotilitydisorderscopy-converted-compressed1-converted-200703121904/75/Esophageal-motility-disorders-60-2048.jpg)


































