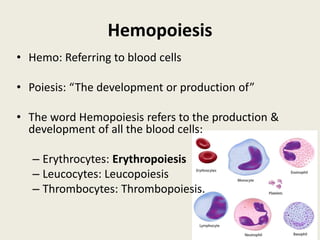
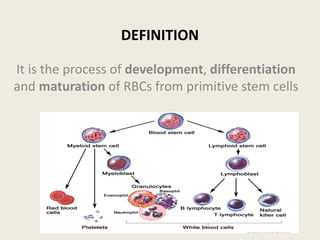
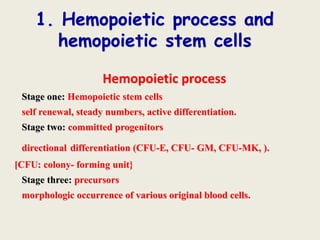
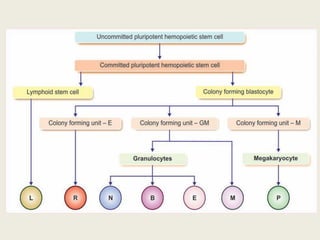
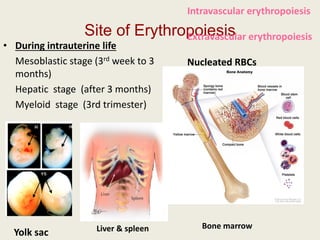
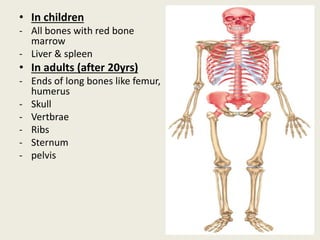
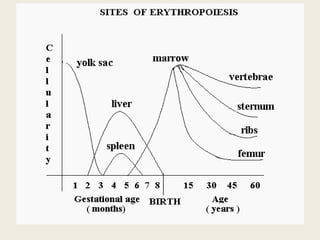
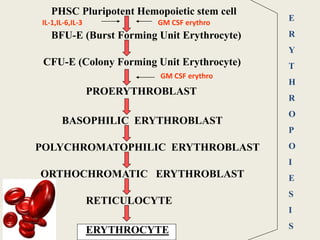
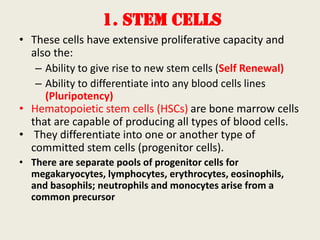
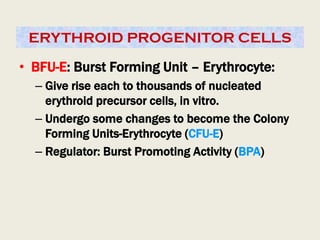
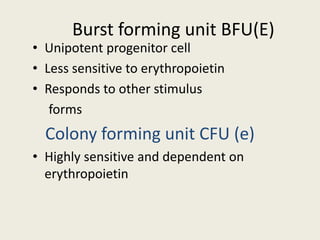
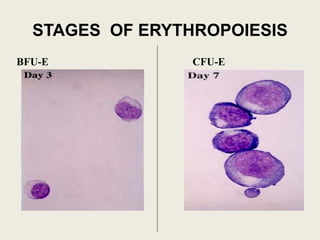
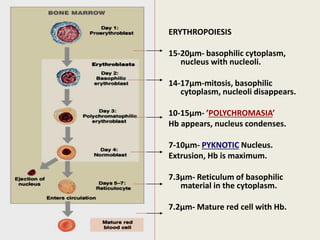
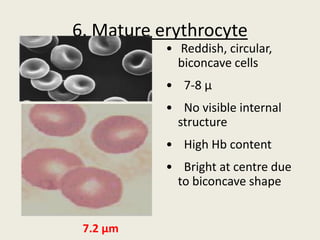
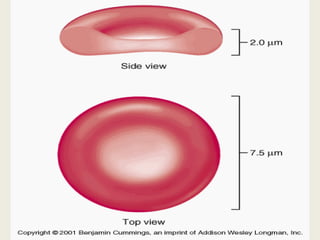
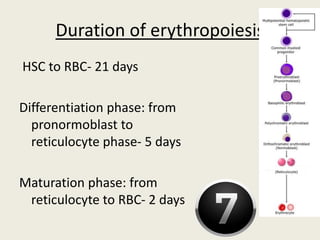
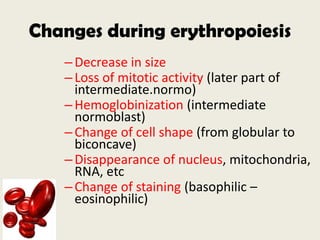
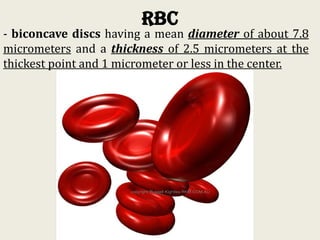
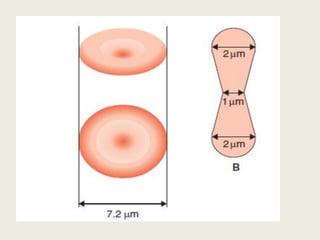
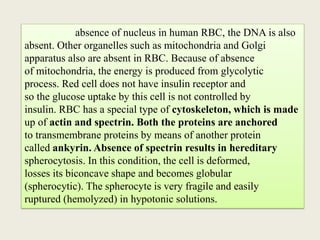
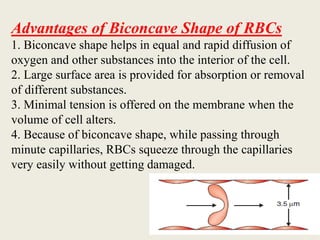
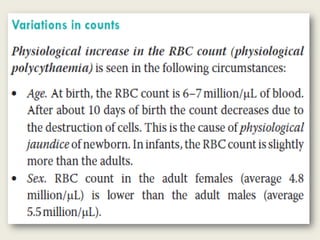
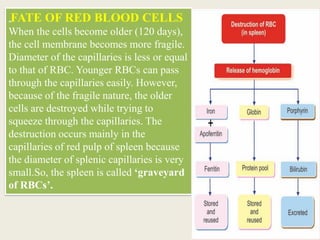
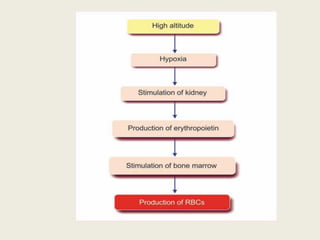
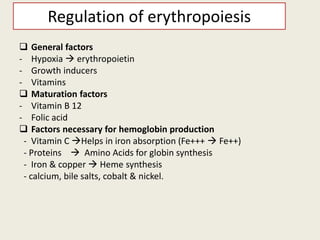
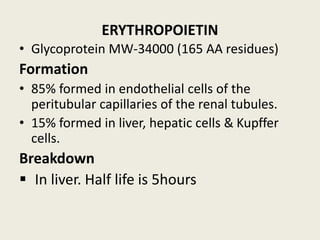
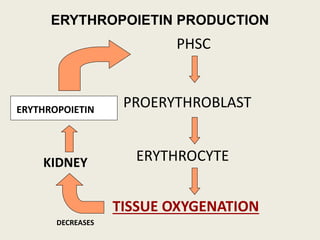
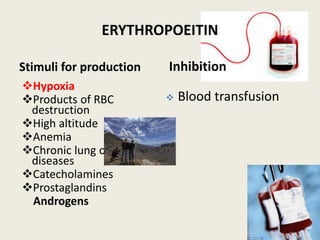
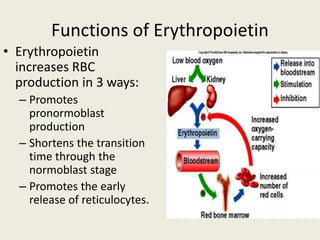
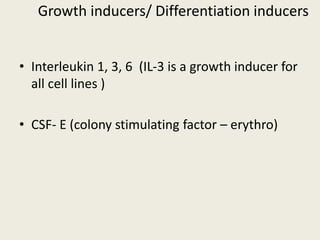
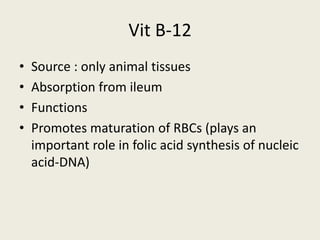
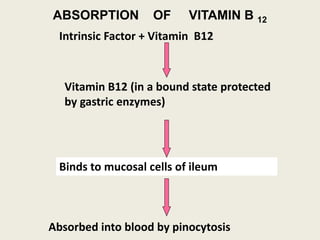
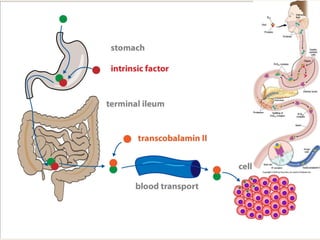
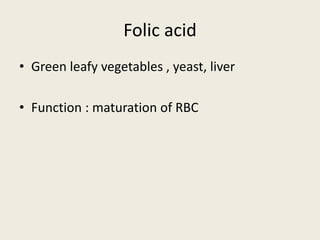
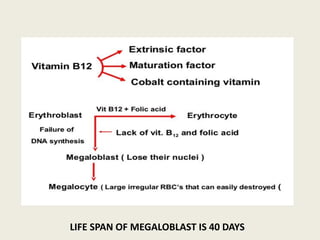
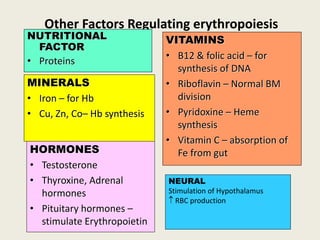
Red blood cells are formed through the process of erythropoiesis, where hemopoietic stem cells in the bone marrow differentiate into mature red blood cells. This process is regulated by erythropoietin, which is released by the kidneys in response to low oxygen levels in the blood and promotes the production and release of reticulocytes from bone marrow. Other factors like iron, vitamin B12, and folic acid are also necessary for hemoglobin production and the maturation of red blood cells. Mature red blood cells are biconcave disks that transport oxygen and carbon dioxide throughout the body and have a lifespan of approximately 120 days before being destroyed by the spleen and liver.