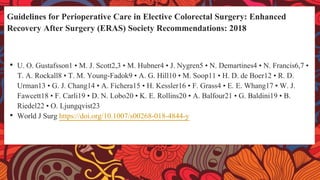
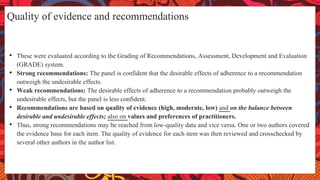
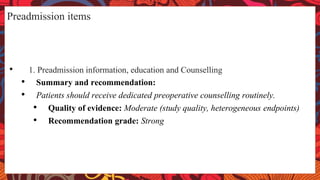
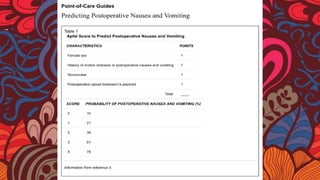
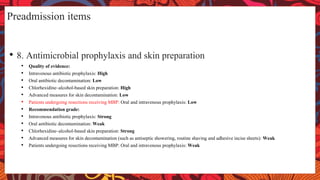
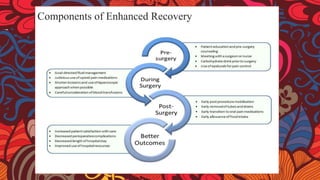
This document provides guidelines for perioperative care in elective colorectal surgery as part of an Enhanced Recovery After Surgery (ERAS) protocol. It makes recommendations for several preadmission items including preadmission counselling and education, preoperative optimization of medical conditions, prehabilitation, preoperative nutrition, management of anemia, and prevention of postoperative nausea and vomiting. The recommendations are based on reviews of the available evidence and are intended to reduce complications and facilitate early recovery after colorectal surgery.