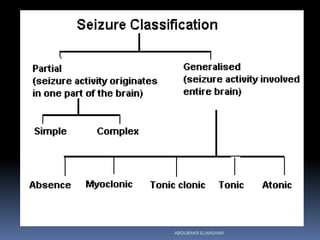
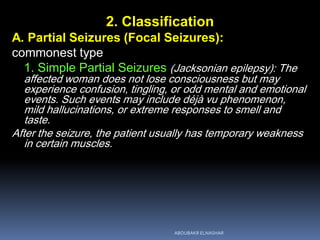
This document discusses epilepsy and pregnancy. It begins with an introduction that covers the incidence of epilepsy in women of childbearing age and classifications of seizures. It then discusses how pregnancy can affect epilepsy and how epilepsy can affect pregnancy, including risks to the mother and fetus. It covers the teratogenic risks of antiepileptic drugs and their mechanisms. The management section discusses diagnosis, differential diagnosis, and considerations in the prenatal, antenatal, intrapartum, and postpartum periods. Fetal outcomes are also addressed.



![4. Antenatal care
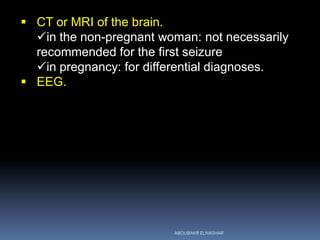
Investigations:
Serum glucose, urea, electrolytes, Ca & Mg
EEG
MRI/CT scan of the head.
Screening for congenital abnormalities:
nuchal translucency scanning
detailed ultrasound at 18 to 20 w
fetal cardiology assessment.
Serial growth scans are required for detection of a
small-for-gestational-age fetus and to plan 479 further
management in women with epilepsy onAEDs. [A]
480 481There is no role for routine antepartum fetal
surveillance with cardiotocography (CTG) in women
482 with epilepsy onAEDs. [D]ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-50-320.jpg)
![2. Vit K
10-20 mg orally
in the last 4 w of pregnancy if taking hepatic
enzyme-inducing drugs.
{vit K-dependent clotting factors may be reduced
and the risk of hgic disease of the newborn is
increased}.
There is insufficient evidence to recommend routine use
of oral vitamin K inWWE on enzyme- 500 inducingAEDs to
prevent haemorrhagic disease of the newborn. [D]
3. Selenium supplementation:
200 µ/day
{minimize the free radical mediated damage}.
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-52-320.jpg)
![A baseline serum or salivary drug level:
{establish compliance and inform future changes in
drug doses}.
If a woman is seizure free:
no need to measure drug levels serially or adjust the
dose unless she has a seizure.
The exception to this is lamotrigine where profound
reduction in drug levels mean that prophylactic
increases in dose are appropriate in pregnancy.
Based on current evidence, routine monitoring of serum
AED levels in pregnancy is not 387 recommended.
Clinicians will need to take into account individual
circumstances for therapeutic 388 drug monitoring. [C]
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-59-320.jpg)
![5. Intrapartum care
Women with epilepsy should be reassured that most
women have an uncomplicated labour and
delivery. [C]
Pregnant women should be counselled that the risk of
seizures in labour is low. [C]
1. Deliver in hospital
WWE on AEDs and at risk of seizures should be
delivered in a consultant-led unit with facilities for
678 one-to-one midwifery care and maternal and
neonatal resuscitation. [GPP]
{risk of seizures increases around the time of delivery.
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-61-320.jpg)
![2. Do not leave unattended in labour or for the first 24
hs postpartum.
{One to two percent of women with epilepsy will have
a seizure during labour and 1-2% will have one in
the first 24 hours postpartum}.
3. Continue regular AEDs in labour. If this cannot be
tolerated orally, a 578 parenteral alternative should
be administered. [GPP]
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-62-320.jpg)
![4. Pain relief in labour
Early epidural analgesia.
{limit the risk of precipitating a seizure because of
pain and anxiety}
Pethidine should never be used
{metabolised to norpethidine, which is
epileptogenic}.
Diamorphine is an option.
Pain relief in labour should be prioritised inWWE, with
options including transcutaneous electrical 647 nerve
stimulation (TENS), entonox (nitrous oxide) and regional
analgesia. [GPP]
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-63-320.jpg)
![5. If seizures that are not rapidly self-limiting occur
in labour:
A. Oxygen
B. lorazepam IV(4 mg over two minutes) or
diazepam [10-20 mg (rectal gel) or
10-20 mg IV at 2 mg/min]
Continuous fetal monitoring is recommended
following a seizure and in women at high risk of a
612 seizure in labour. [GPP]
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-64-320.jpg)
![7. Mode of delivery
most women with epilepsy have normal vaginal
deliveries
CS:
recurrent generalised seizures in late pregnancy or
labour. or
when the mother is unable to cooperate.
There is no known contraindication for use of any
induction agents inWWE onAEDs. [GPP]
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-66-320.jpg)
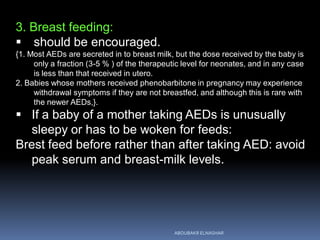
![ Mother
WWE and their caregivers need to be aware of the
increased risk of seizure deterioration during 703 and
immediately after delivery. [C]
1. AED:
{lamotrigine and phenobarbitone: cross in significant amounts
(30-50%) to breast milk
phenobarbitone, prirnidone and lamotrigine: accumulate in a
breastfed baby due to slow elimination.
Lamotrigine: metabolized mainly by glucuronidation and the
capacity to glucuronidate is not fully developed in
newborns}.
Lamotrigine should not be initiated in
breastfeeding mothers.
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-70-320.jpg)
![ If the mother's dose of AED was increased during
pregnancy: gradually decreased again over a few
weeks in the puerperium.
{Blood levels of phenytoin and lamotrigine increase rapidly
following delivery, but carbamazepine and valproate take
longer to return to pre-conception levels].
if doses of lamotrigine have been increased in
pregnancy they should probably be decreased
relatively rapidly postpartum.
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-71-320.jpg)
![2. Bathing:
never should be performed alone, as a brief
lapse in attention can result in a fatal drowning.
Wet sponge not water bath.
Mothers should be well supported in the postnatal
period to ensure that triggers of seizure 708
deterioration such as sleep deprivation, stress and
pain are minimised. [GPP]
WWE should be screened for depressive disorder in
the puerperium. Mothers should be informed 800
about the symptoms and provided with contact
details for any assistance. [D]
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-72-320.jpg)

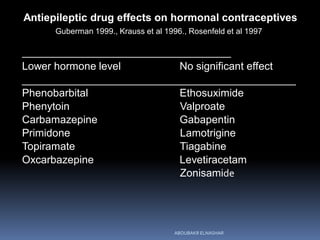
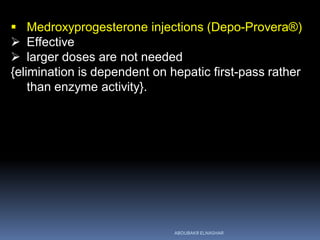
![ Women should be counselled that the efficacy of
oral contraceptives (combined hormonal
contraception, progestogen-only pills), transdermal
patches, vaginal ring and progestogen-only
implants may be affected if they are on enzyme-
inducing AEDs, such as carbamazepine,
phenytoin, 822 phenobarbitone, primidone,
oxcarbazepine and eslicarbazepine. [C]
COC:
pill containing 50 ug EE or
two pills containing 30 ug.
may still not be effective and an alternative method
of contraception may be appropriate.
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-75-320.jpg)
![ Women on lamotrigine monotherapy and combined
oral contraceptives (COC) should be informed 836 of
the potential increase in seizures due to a fall in the
levels of lamotrigine. [C]
POP:
The efficacy is also affected by enzyme-inducing
antiepileptic medication.
2 rather than one daily pill of
Micronor (norethisterone 350 ug) or
Microval (levonorgestrel 30 ug).
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-76-320.jpg)
![ The 'morning after pill'
can be used if required, but again a double dose is
advised.
An intrauterine device is the preferred choice for 833
emergency contraception. [D]
Barriers and IUDs are recommended.
Copper intrauterine devices, the levonorgestrel-
releasing intrauterine system (LNG-IUS)
ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/epilepsy2016-160313045821/85/EPILEPSY-AND-PREGNANCY-78-320.jpg)