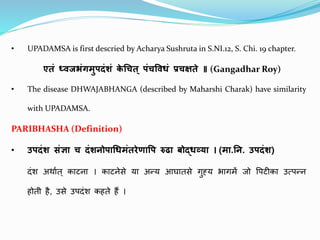
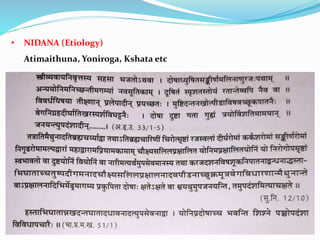
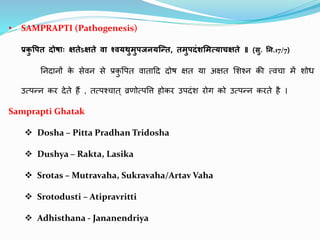
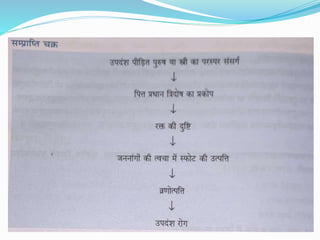
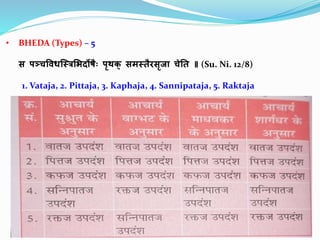
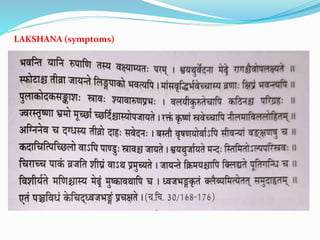
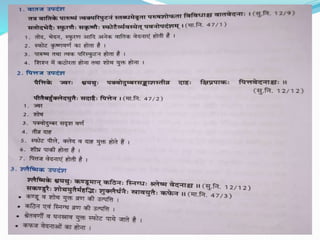
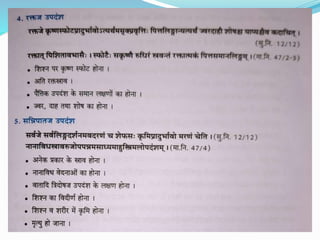
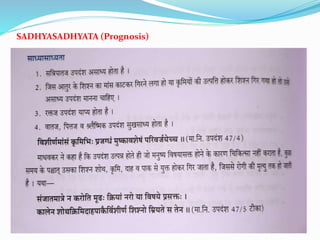
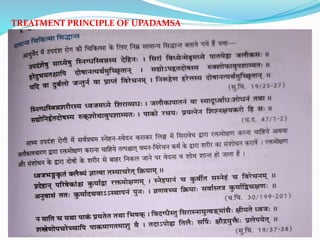
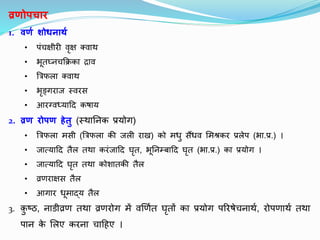
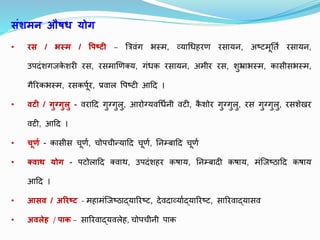
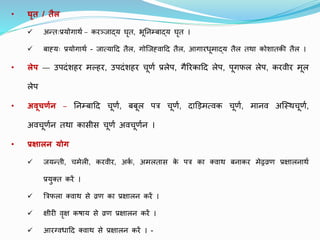
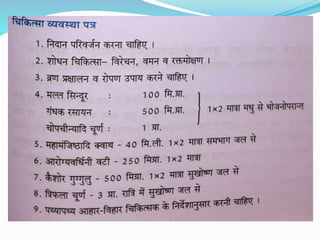
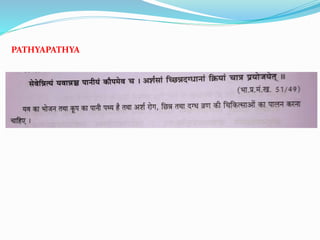
Upadamsa is an Ayurvedic condition characterized by painful genital ulcers. It is caused by vitiation of the doshas, especially pitta, from factors like excessive sexual intercourse. The doshas then produce inflammation and ulceration on the genitals. Upadamsa presents as tender papules that become pustular and erode into painful ulcers, which may merge. Treatment focuses on cleansing and healing the ulcers through topical applications and oral medications aimed at pacifying the aggravated doshas.