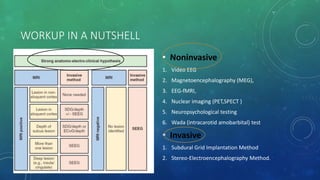
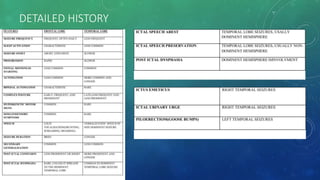
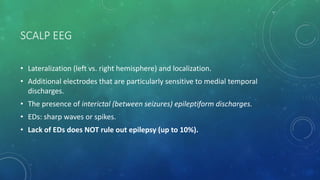
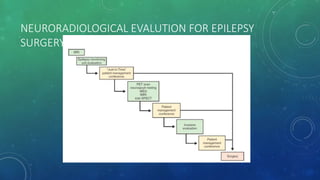
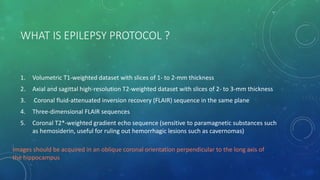
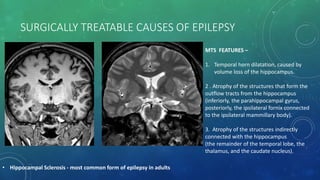
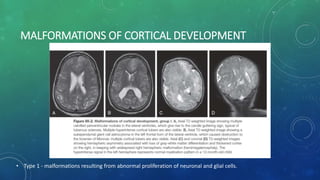
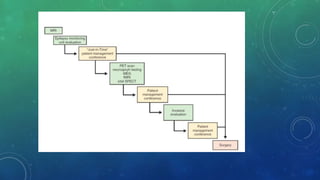
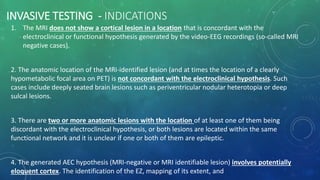
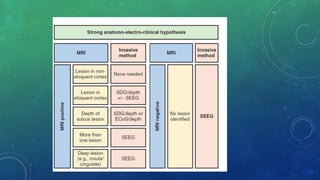
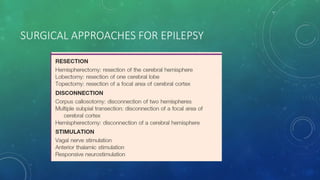
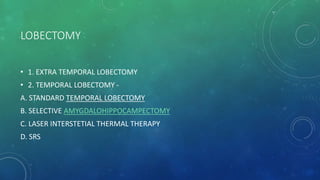
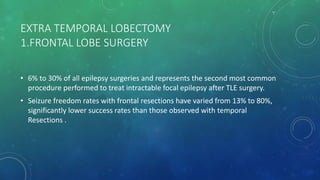
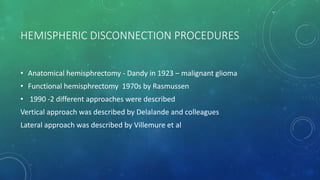
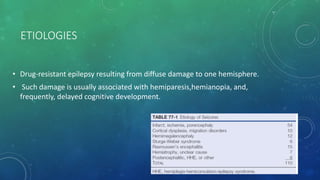
This document discusses various aspects of evaluating and surgically treating epilepsy. It begins by outlining when epilepsy surgery should be considered, such as when seizures persist despite adequate medication. The aim of presurgical evaluation is to accurately map the epileptogenic zone and completely resect or disconnect the area responsible for seizures. Noninvasive and invasive testing methods are described to localize the seizure focus. Common surgical approaches like temporal lobectomy and extra-temporal lobectomy are explained. Outcomes of different procedures and factors influencing prognosis are also summarized.

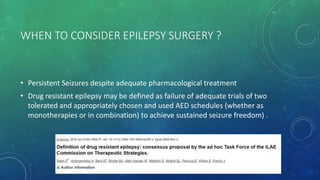
![AIM OF PRESURGICAL WORKUP
• Complete resection (or disconnection) of the cortical areas or networks
responsible for the generation of seizures (epileptogenic zone [EZ]), leading to
complete seizure control in patients in whom multiple antiepileptic
medications have failed.
• Accurate and comprehensive mapping of the anatomo-electro-clinical (AEC)
network](https://image.slidesharecdn.com/epilepsysurgery-190420070646/85/Epilepsy-surgery-3-320.jpg)