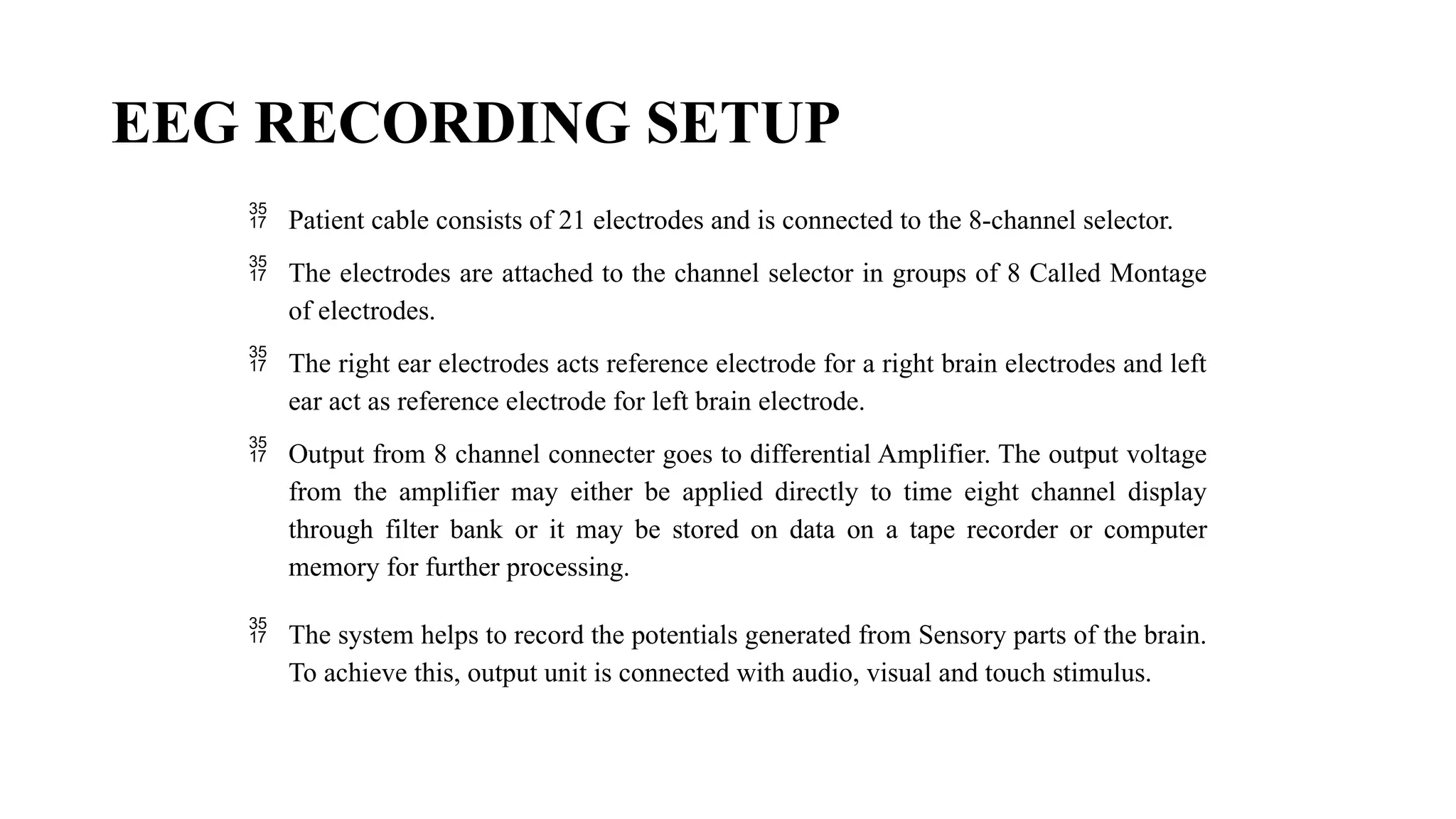
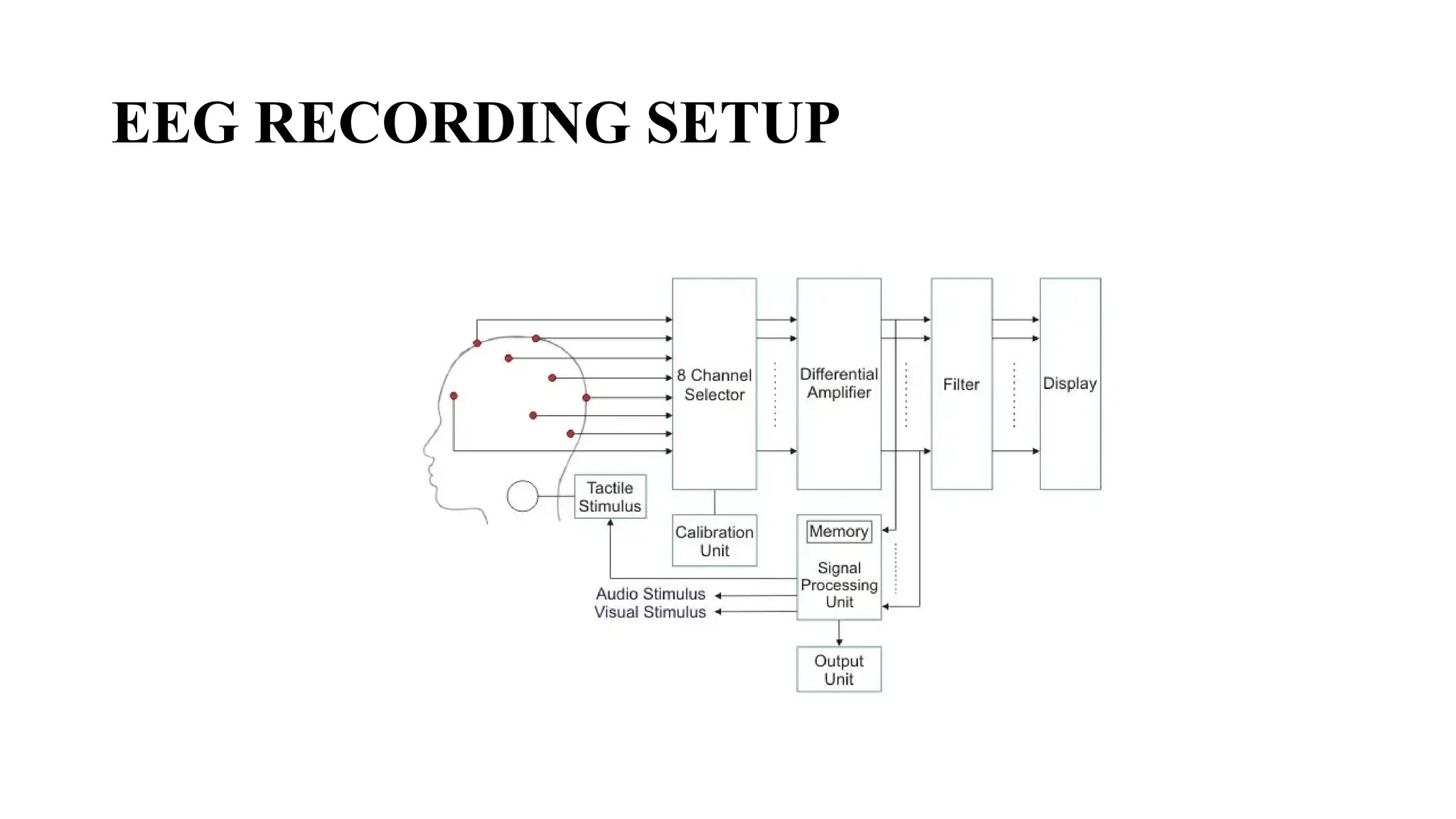
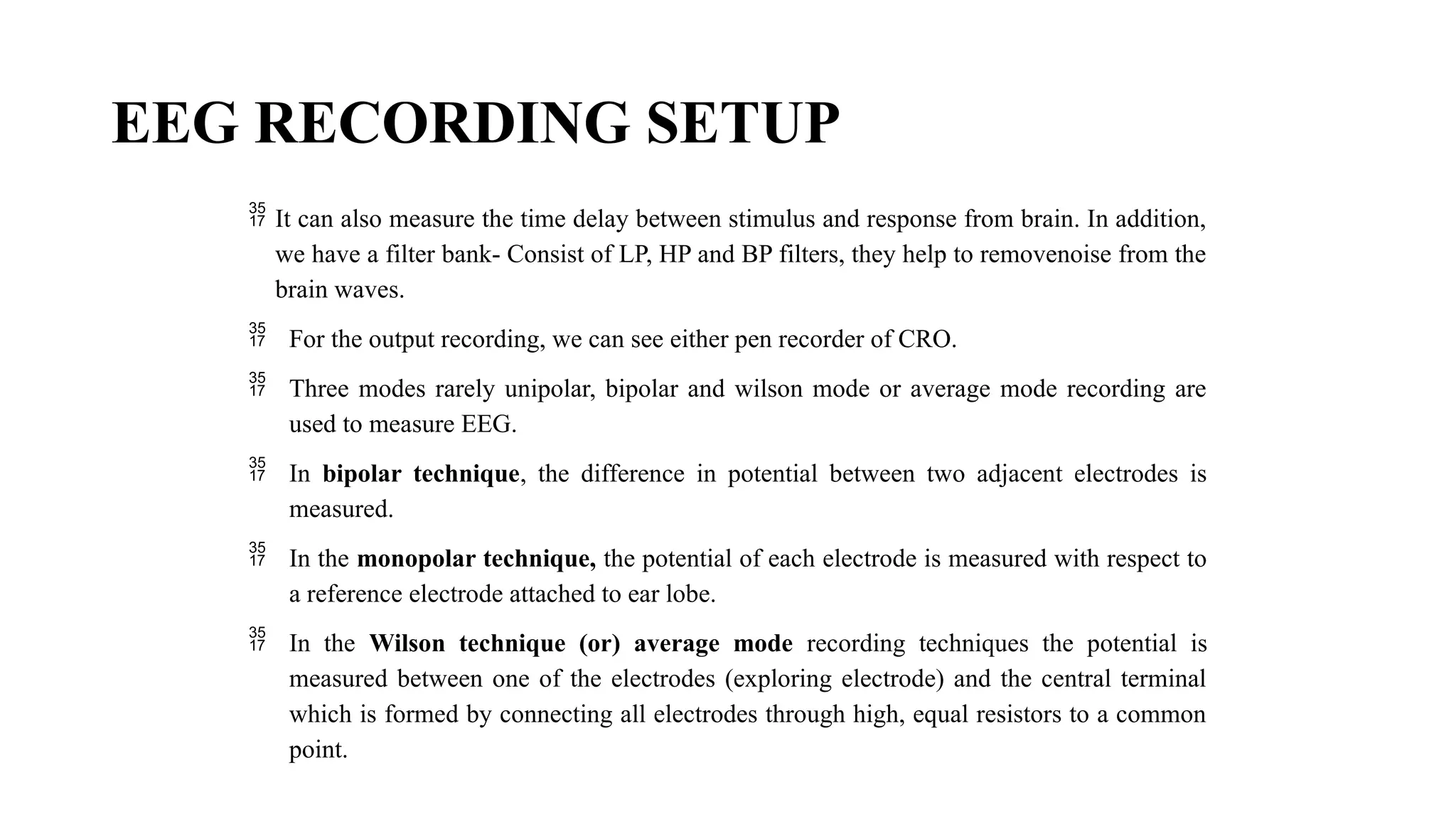
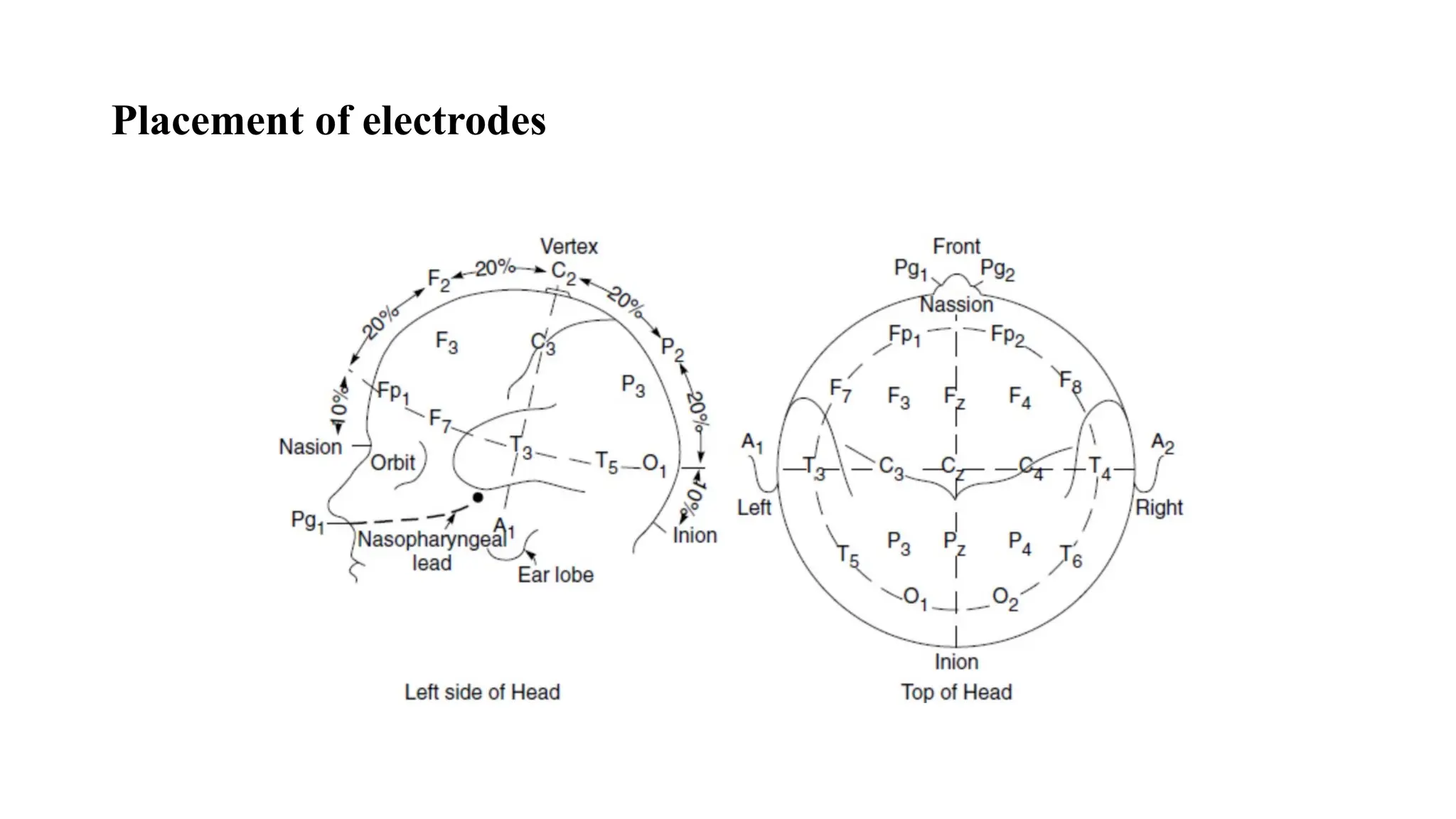
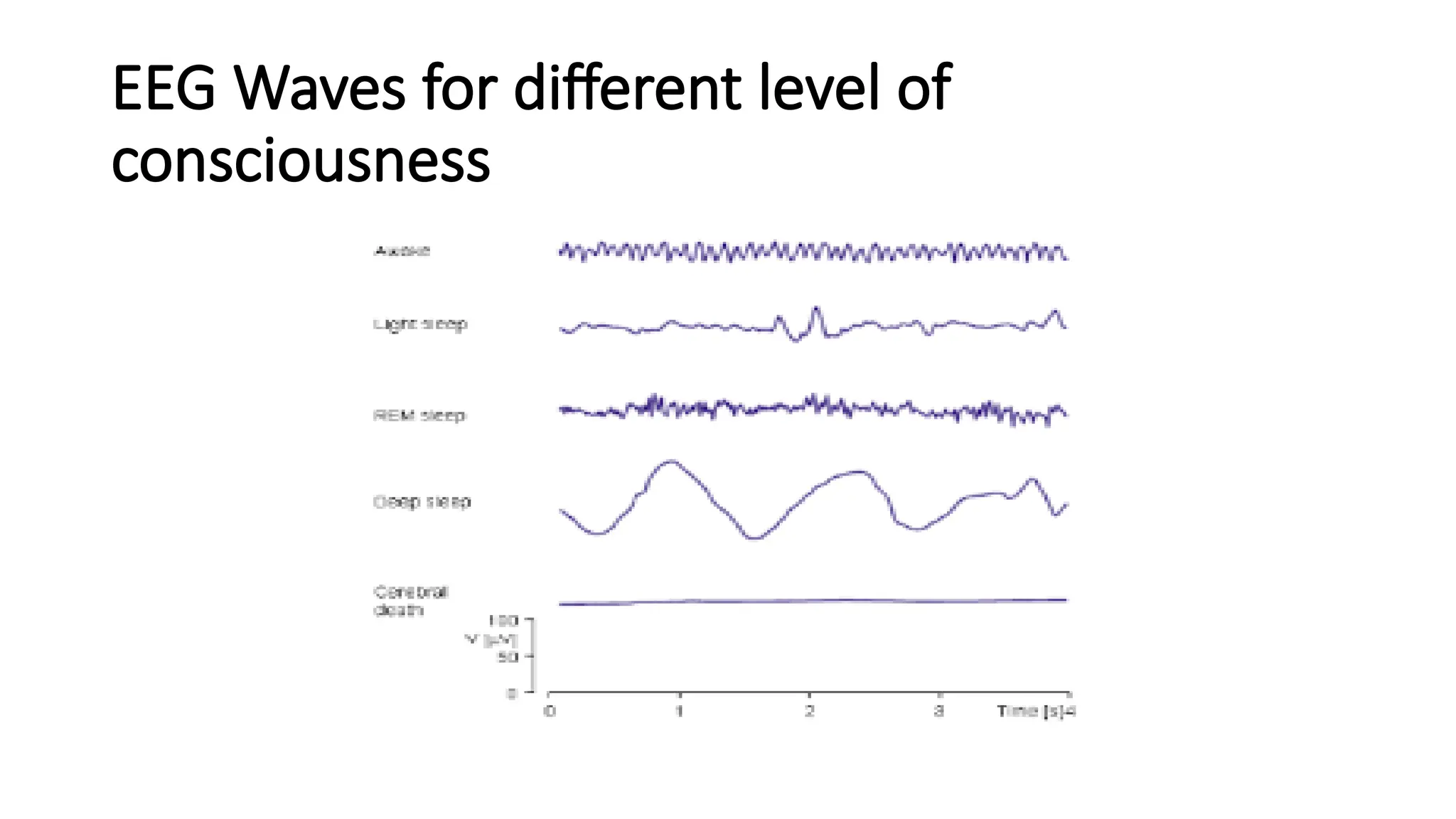
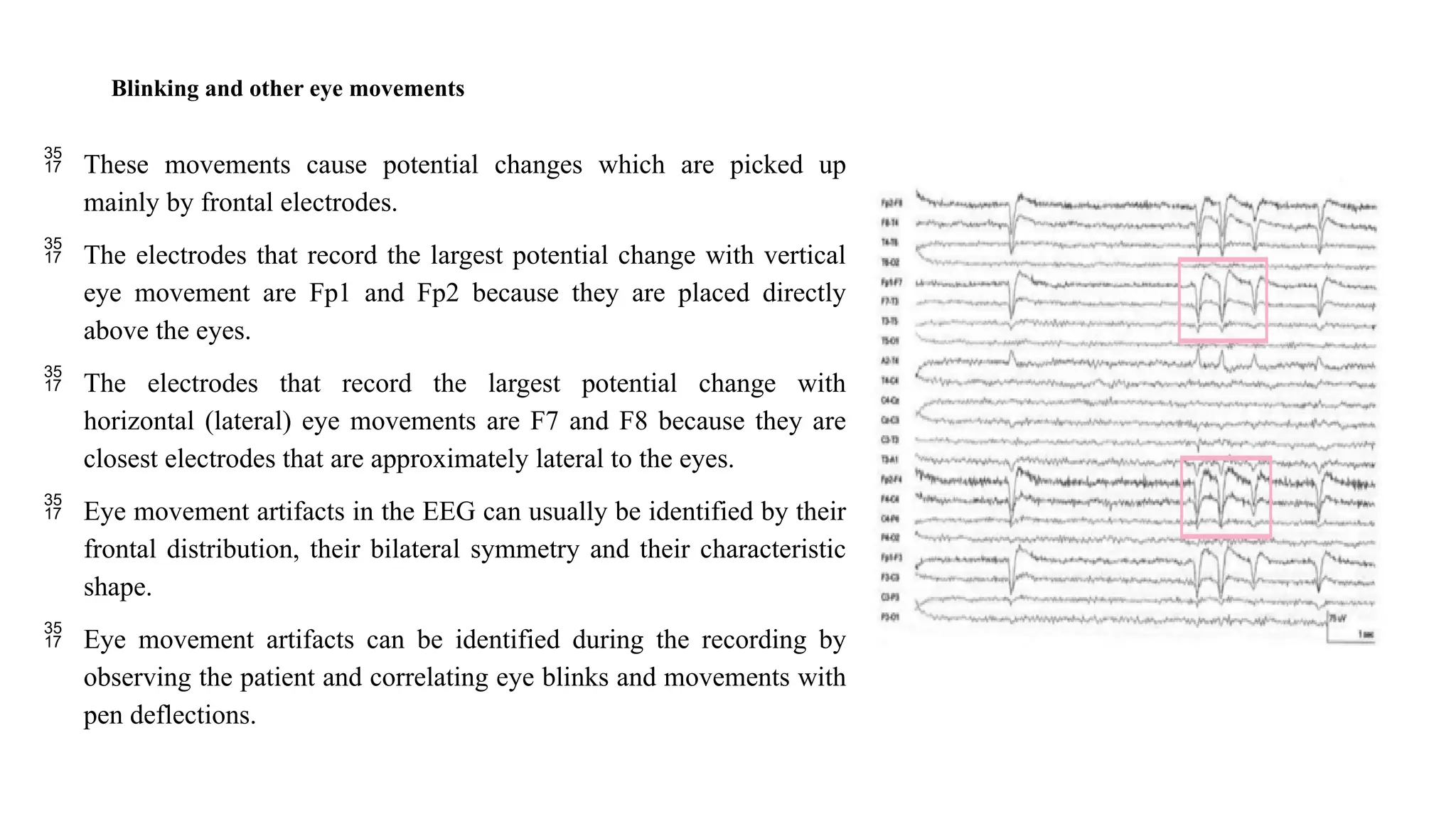
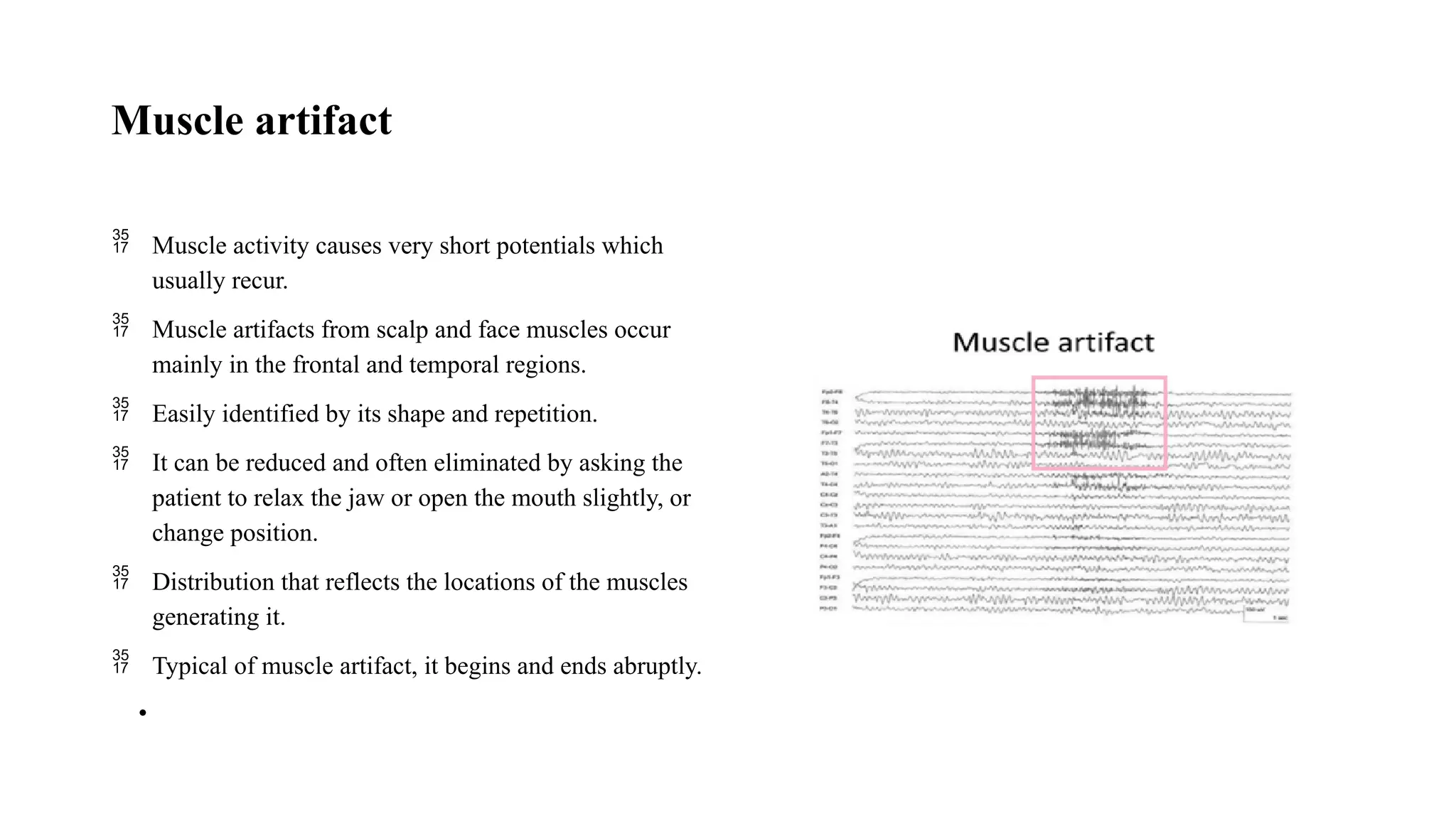
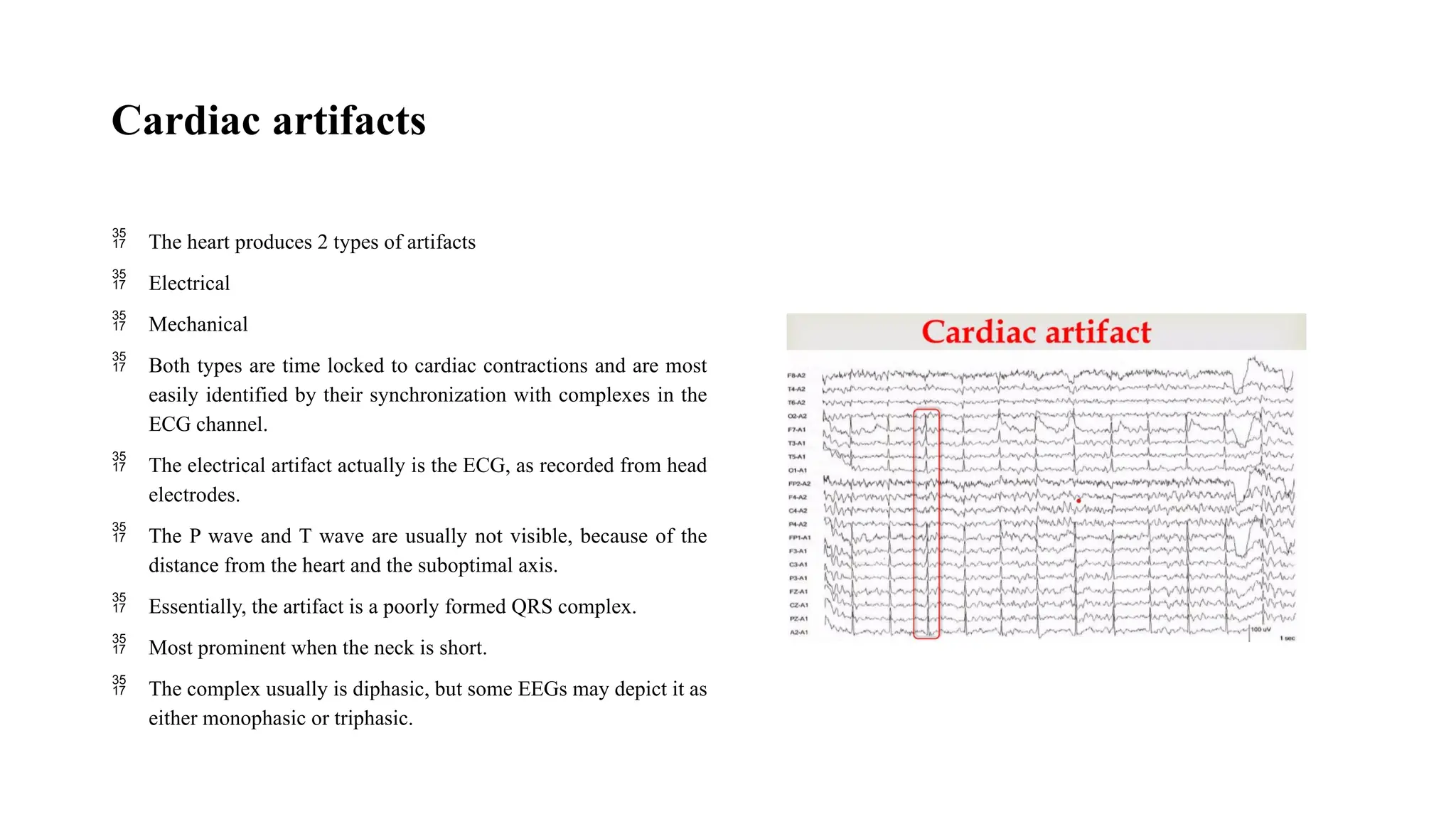
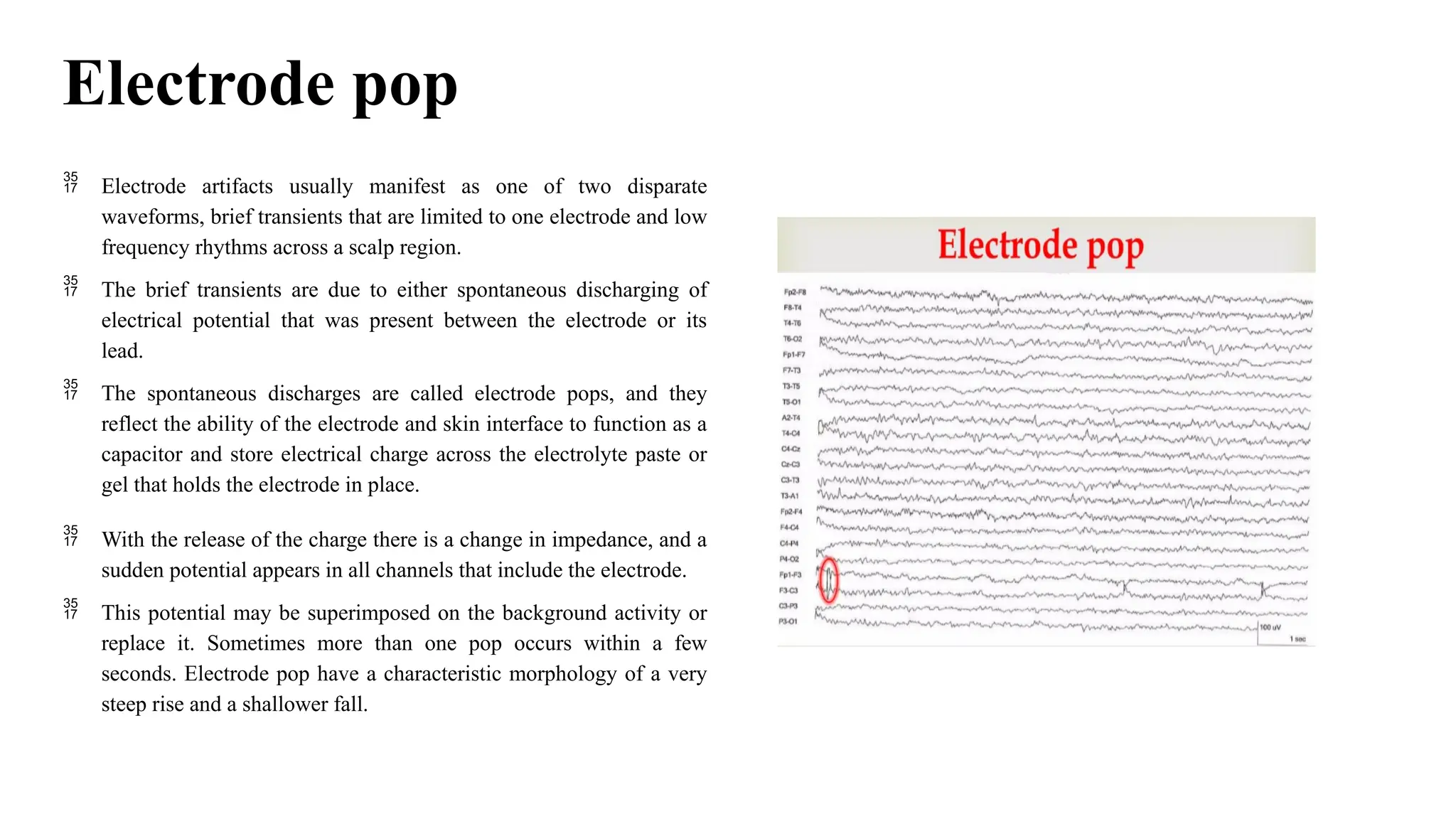
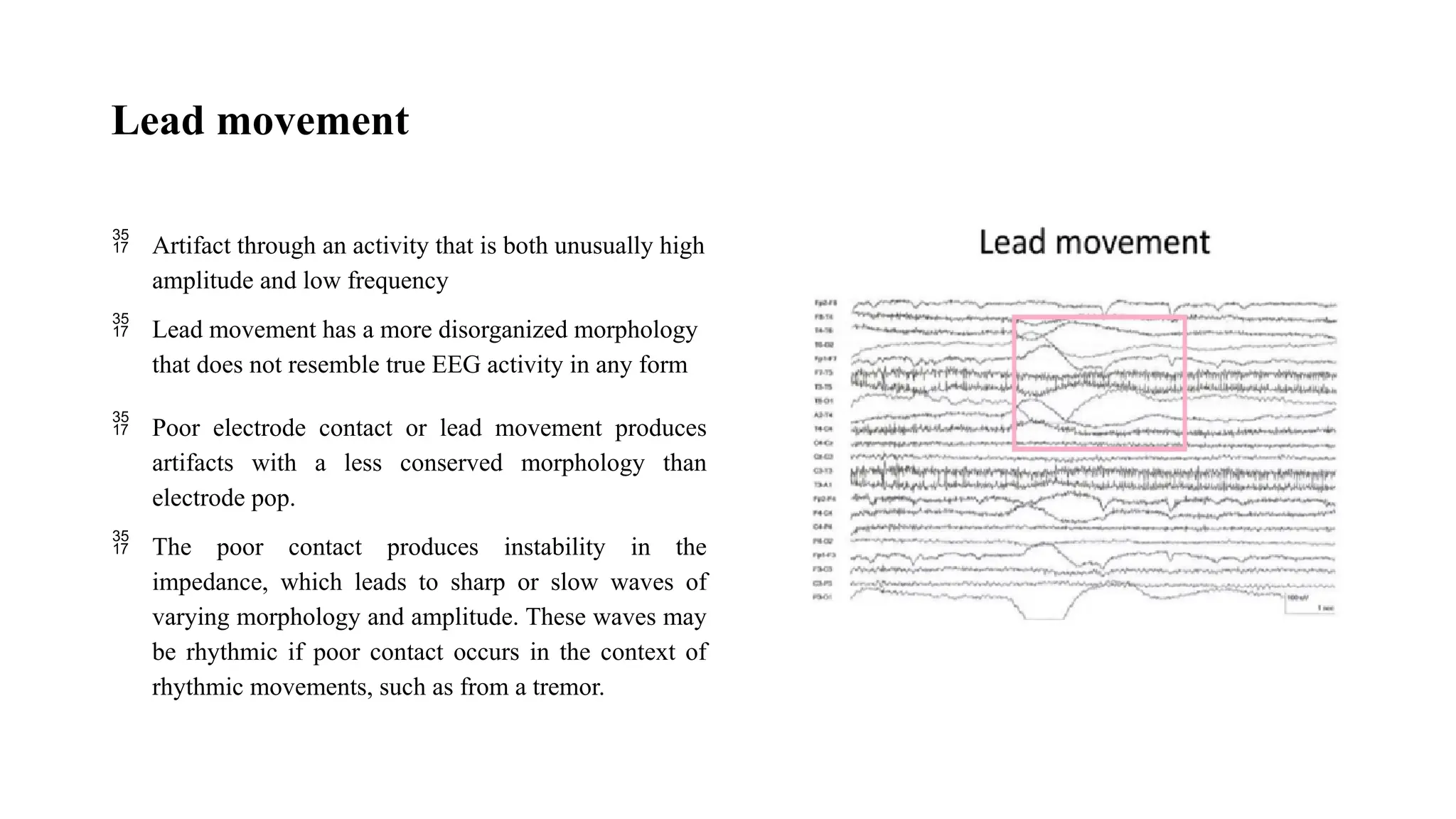
The document covers electroencephalography (EEG), detailing its principles, applications, and technical aspects, especially in relation to diagnosing brain disorders such as epilepsy and assessing brain health in neonatal and pediatric populations. It describes EEG setup, including electrode placement using the 10-20 system, the effect of various physiological and non-physiological artifacts on recordings, and benign variants found in EEG readings. The content emphasizes the importance of EEG in diagnosing conditions like sleep disorders, brain tumors, and monitoring brain activity during medical procedures.