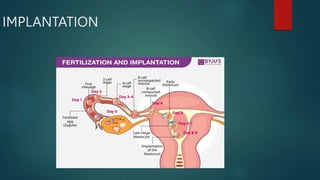
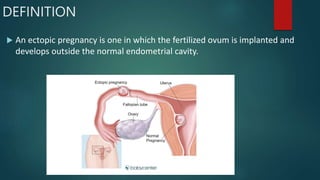
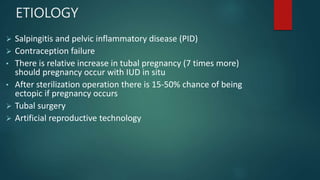
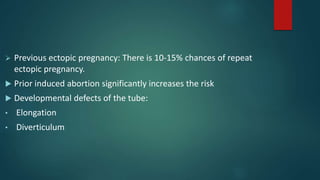
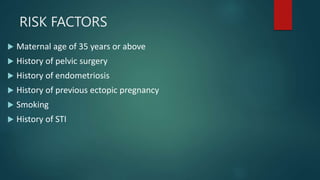
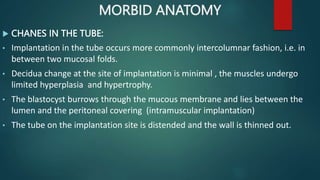
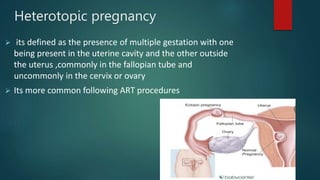
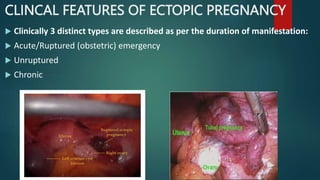
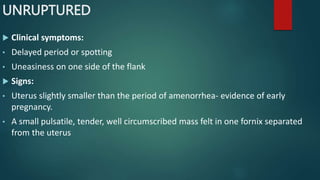
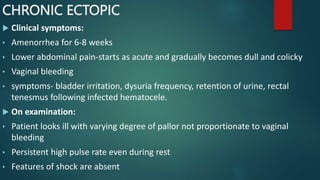
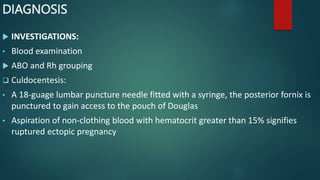
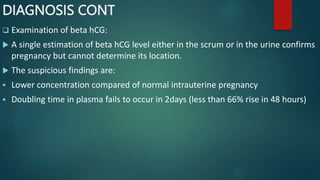
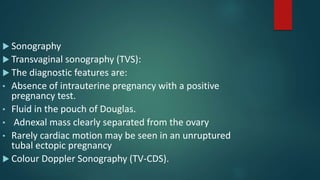
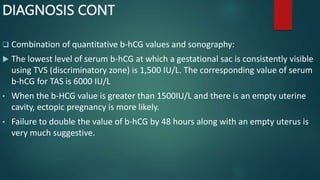
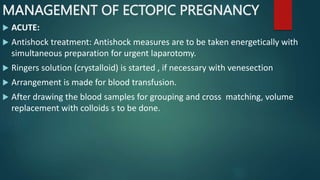
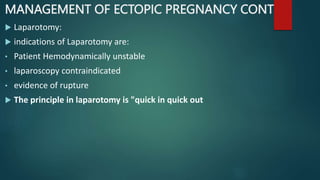
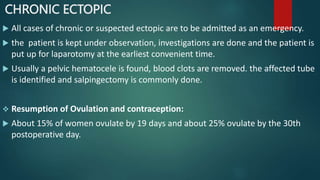
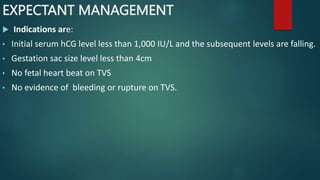
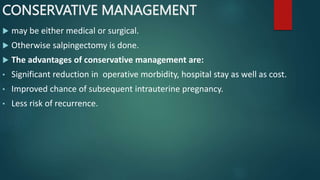
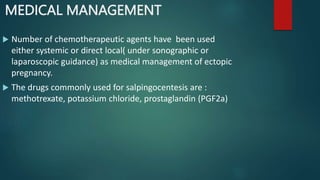
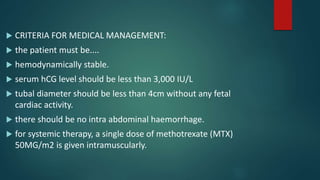
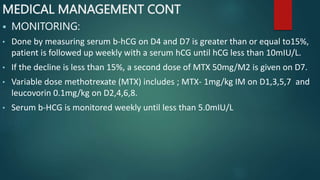
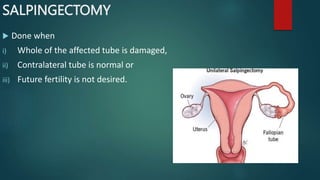
This document discusses ectopic pregnancy, which occurs when a fertilized egg implants outside the uterus, most commonly in the fallopian tubes. It defines ectopic pregnancy and outlines the various sites it can occur. It identifies risk factors like STIs, previous pelvic infections or surgeries. Signs and symptoms depend on whether the ectopic pregnancy has ruptured or not. Diagnosis involves blood tests, ultrasound and laparoscopy. Treatment options include expectant management for early, stable ectopics or surgery like salpingectomy if ruptured or unstable. The goal is to resolve the ectopic pregnancy while preserving future fertility when possible.