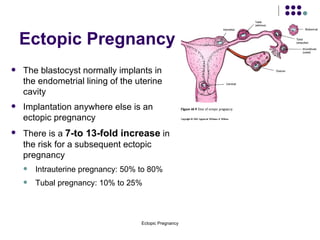
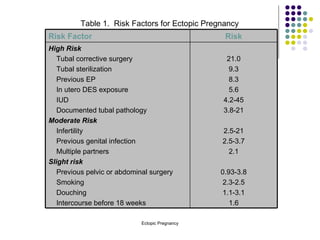
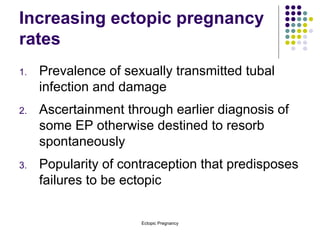
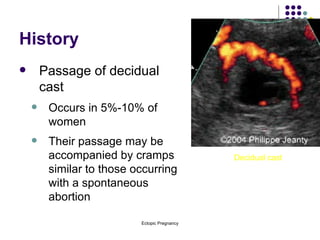
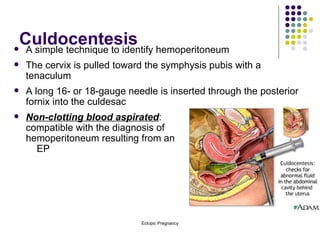
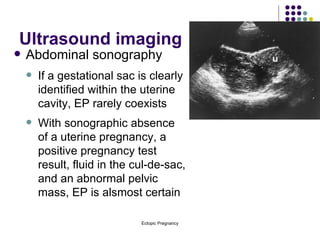
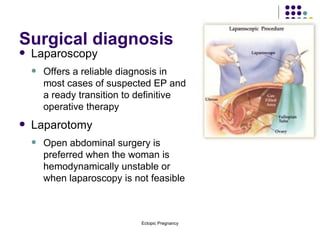
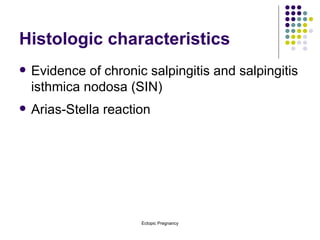
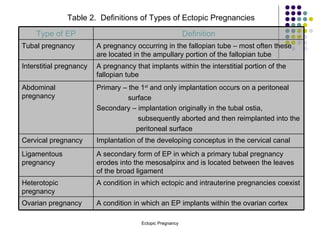
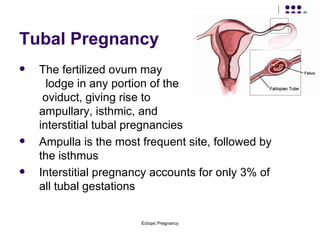
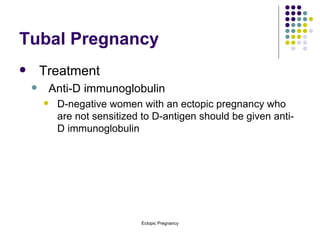
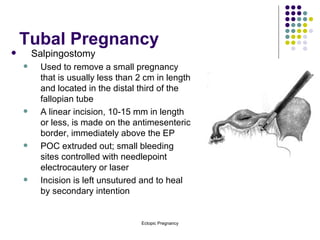
The document discusses various types of ectopic pregnancies, their risk factors, symptoms, diagnosis, and treatment options. The main types discussed are tubal, cervical, ovarian, abdominal, interstitial, interligamentous, and heterotopic pregnancies. Tubal pregnancies are the most common type and usually implant in the fallopian tube ampulla. Diagnosis involves ultrasound, hCG levels, and laparoscopy. Treatment depends on factors like size and includes surgery like salpingostomy/salpingectomy or medical management with methotrexate.