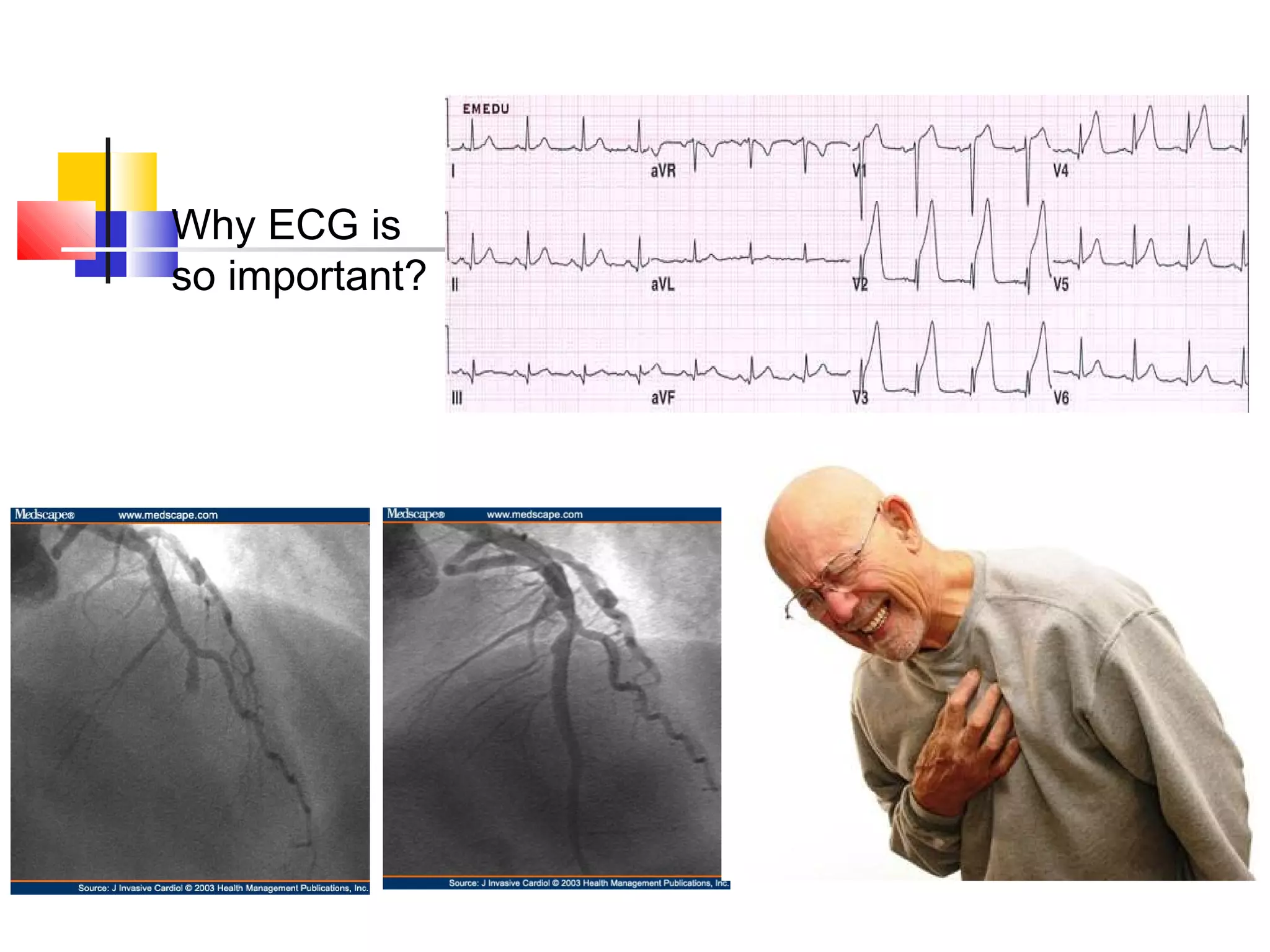
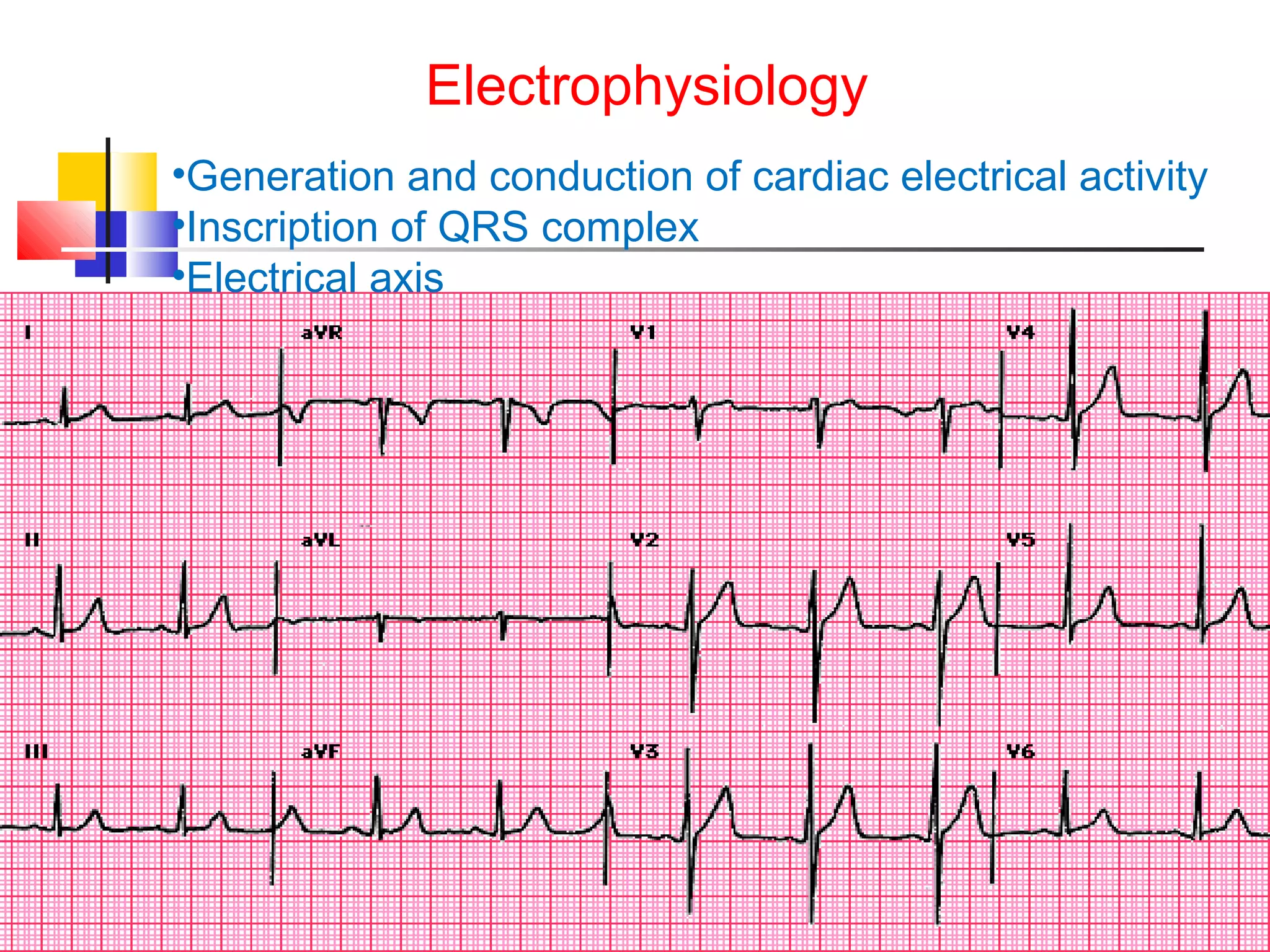
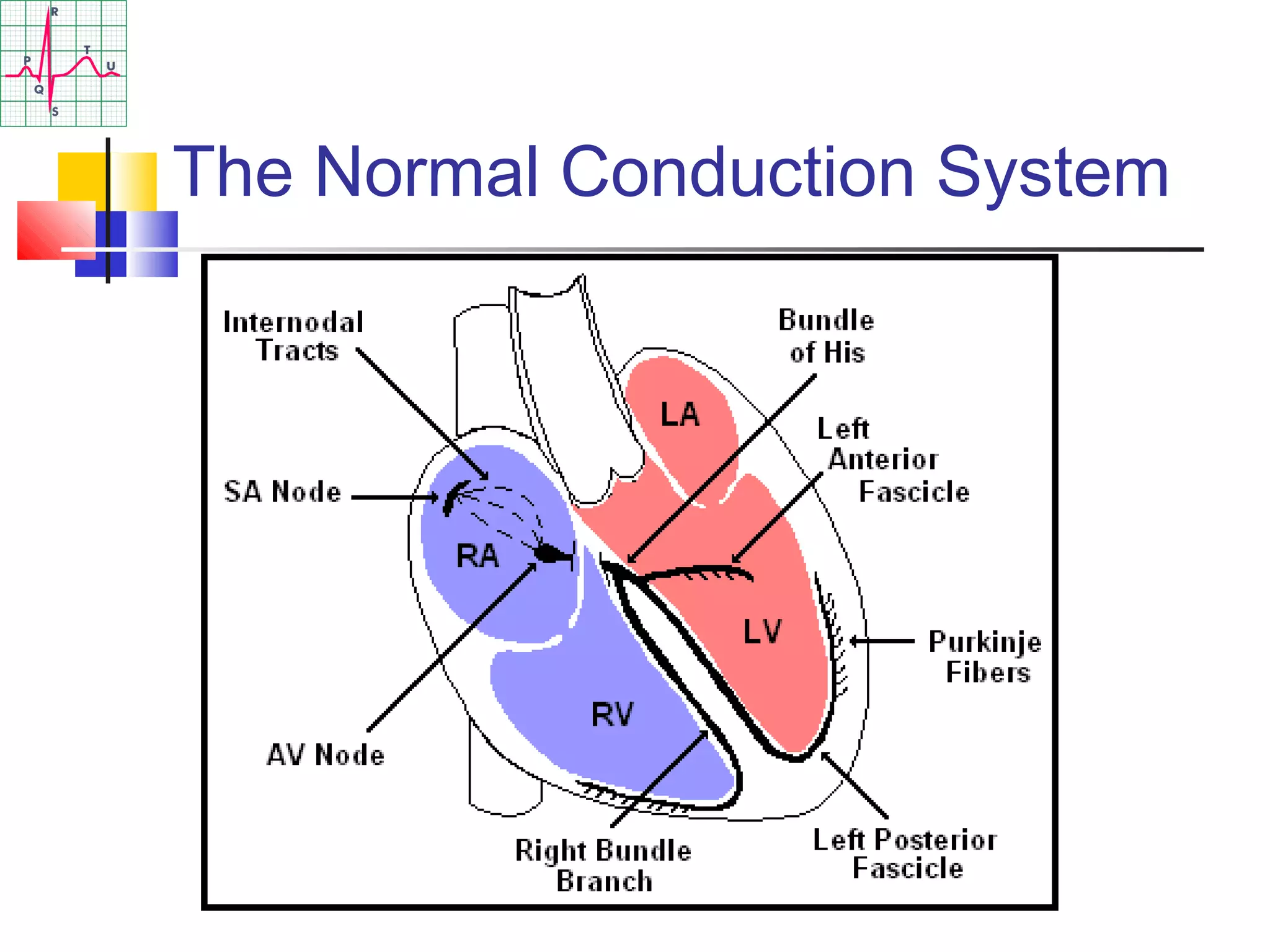
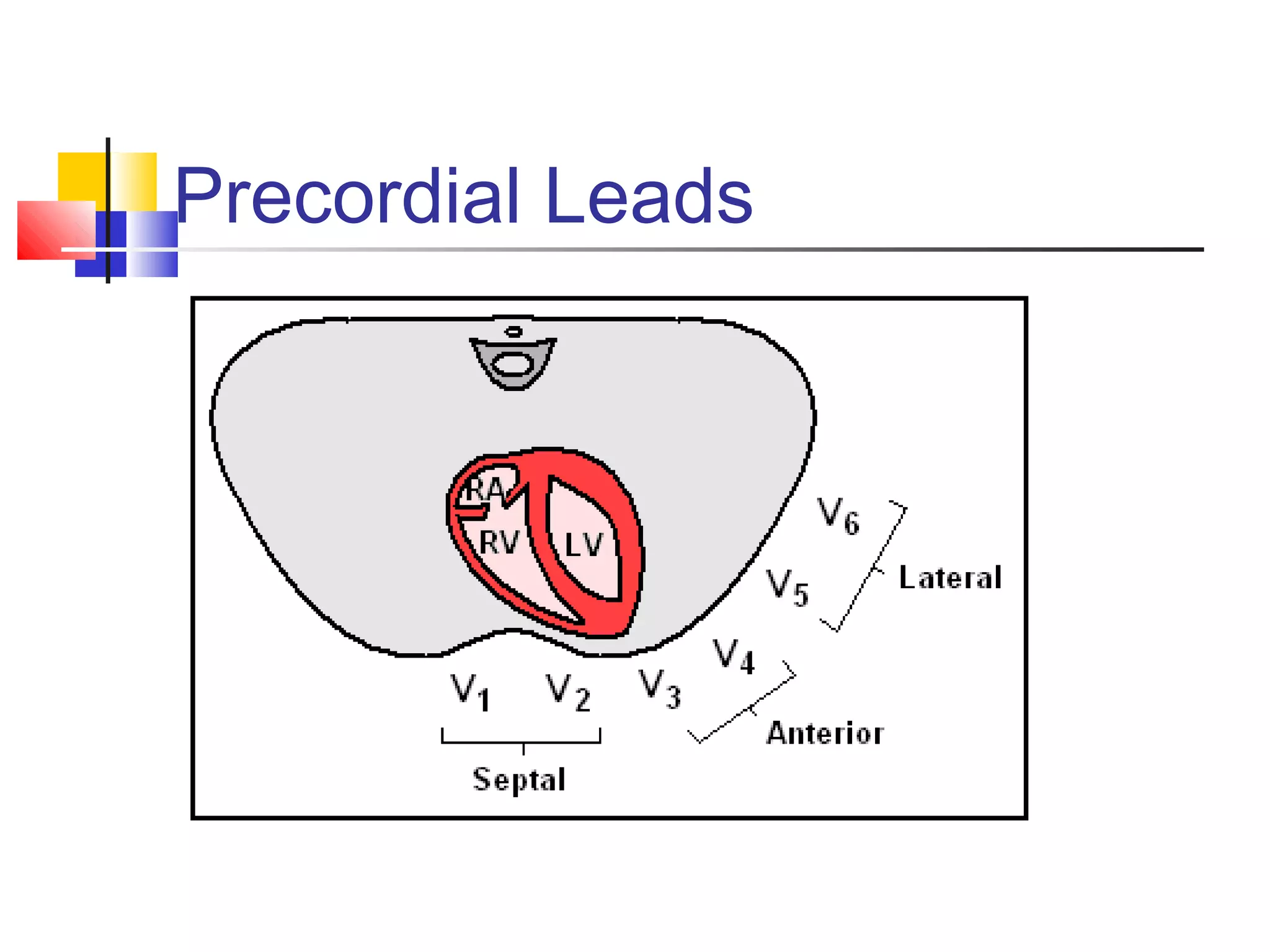
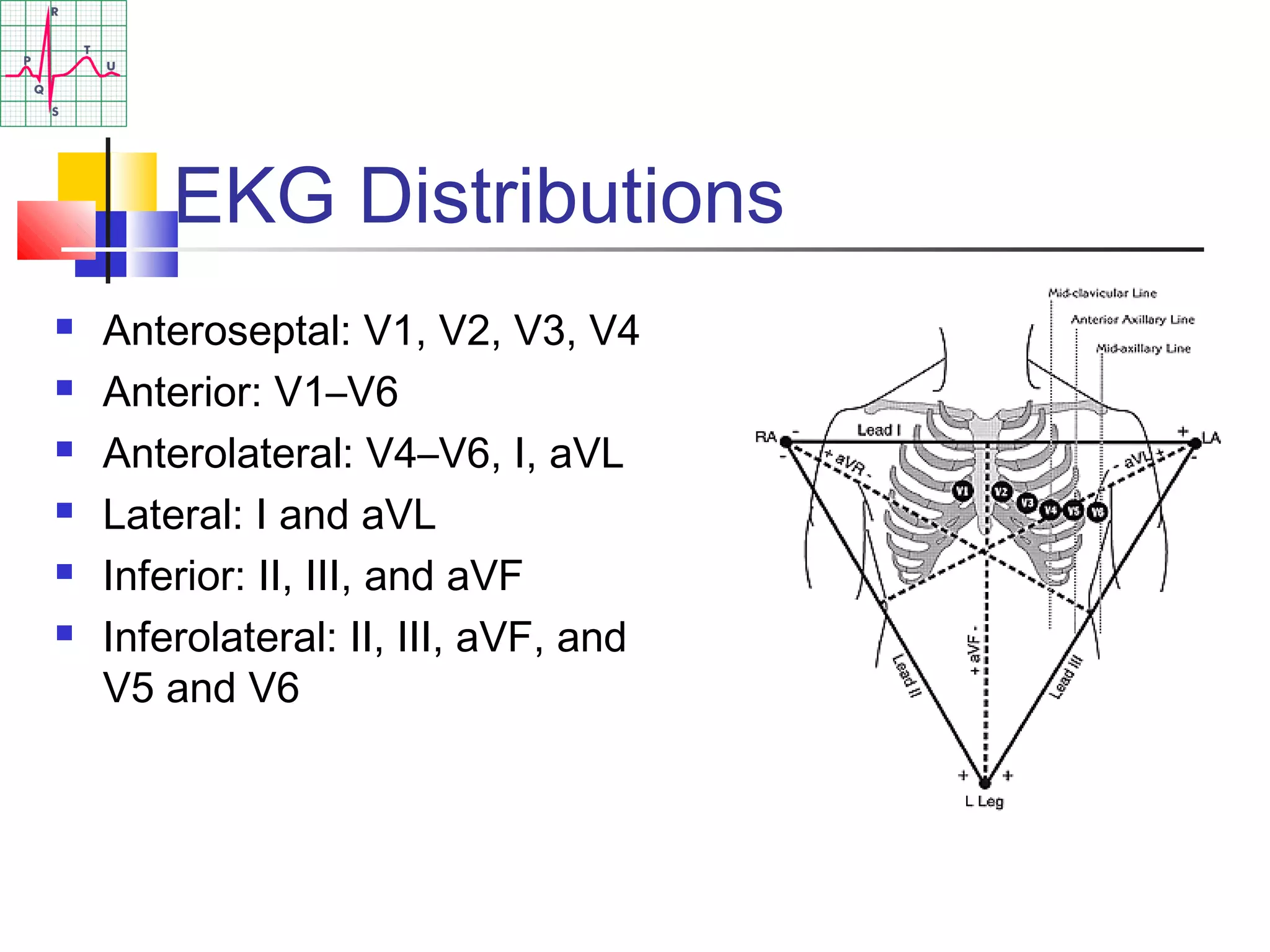
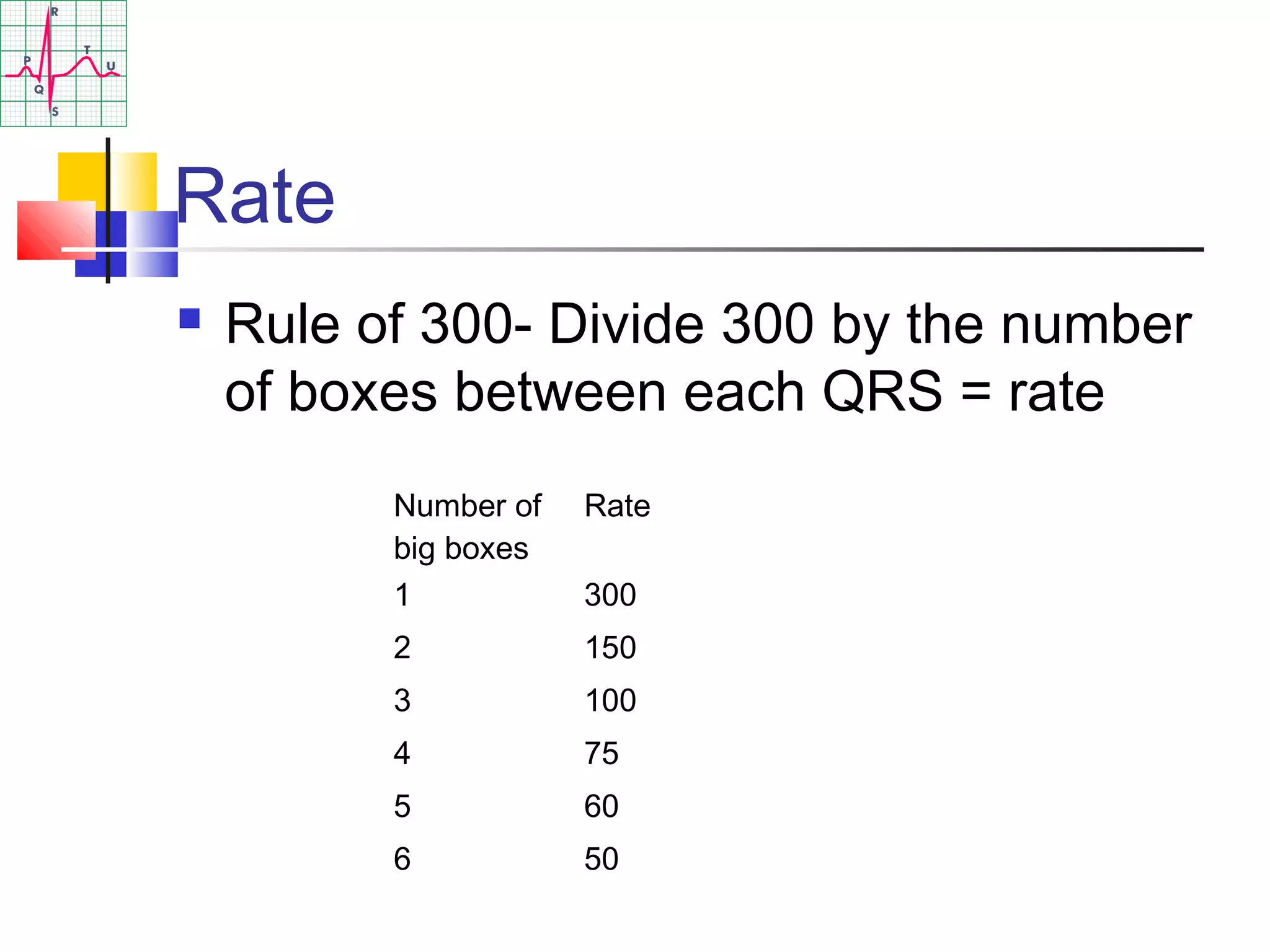
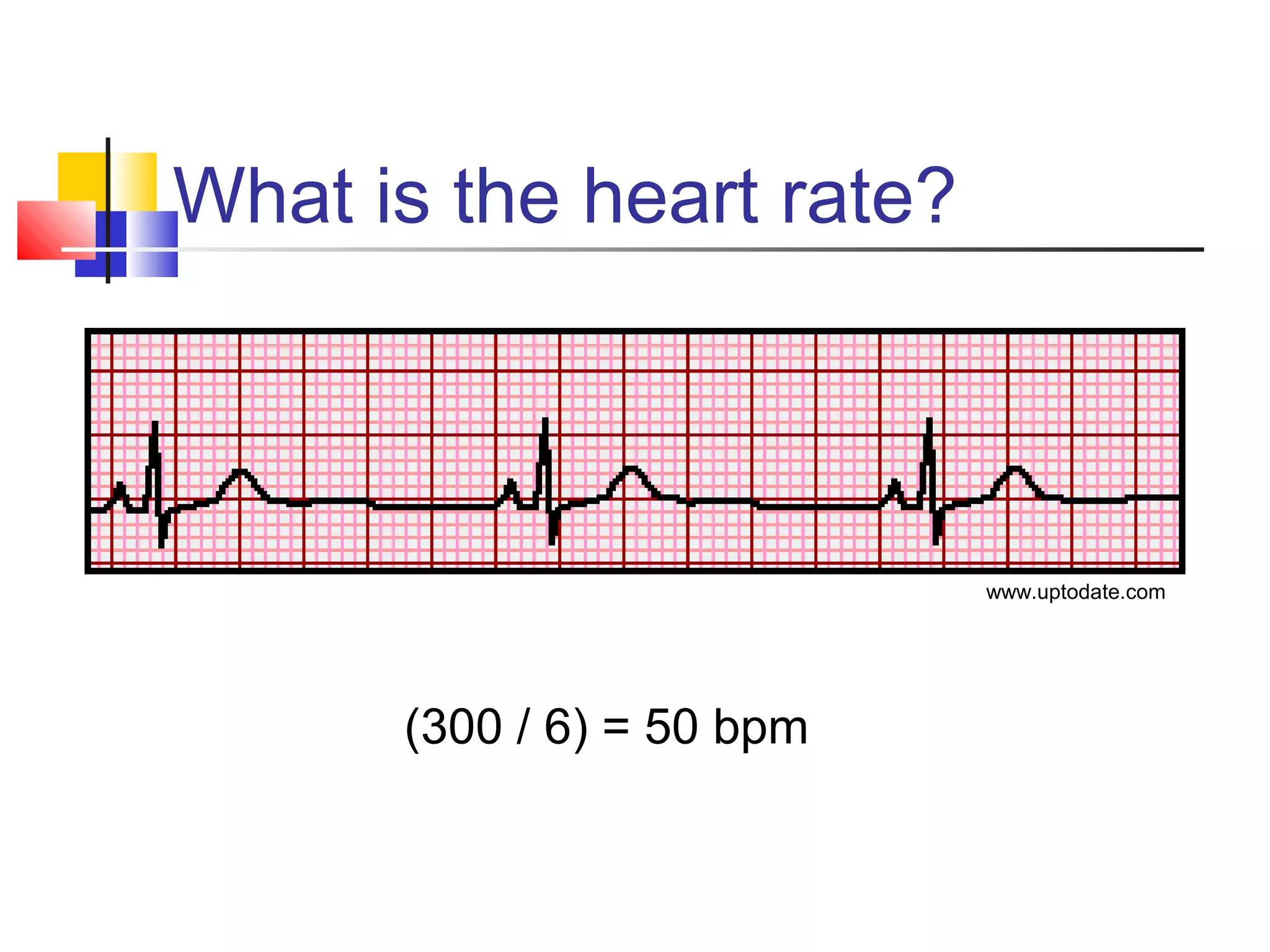
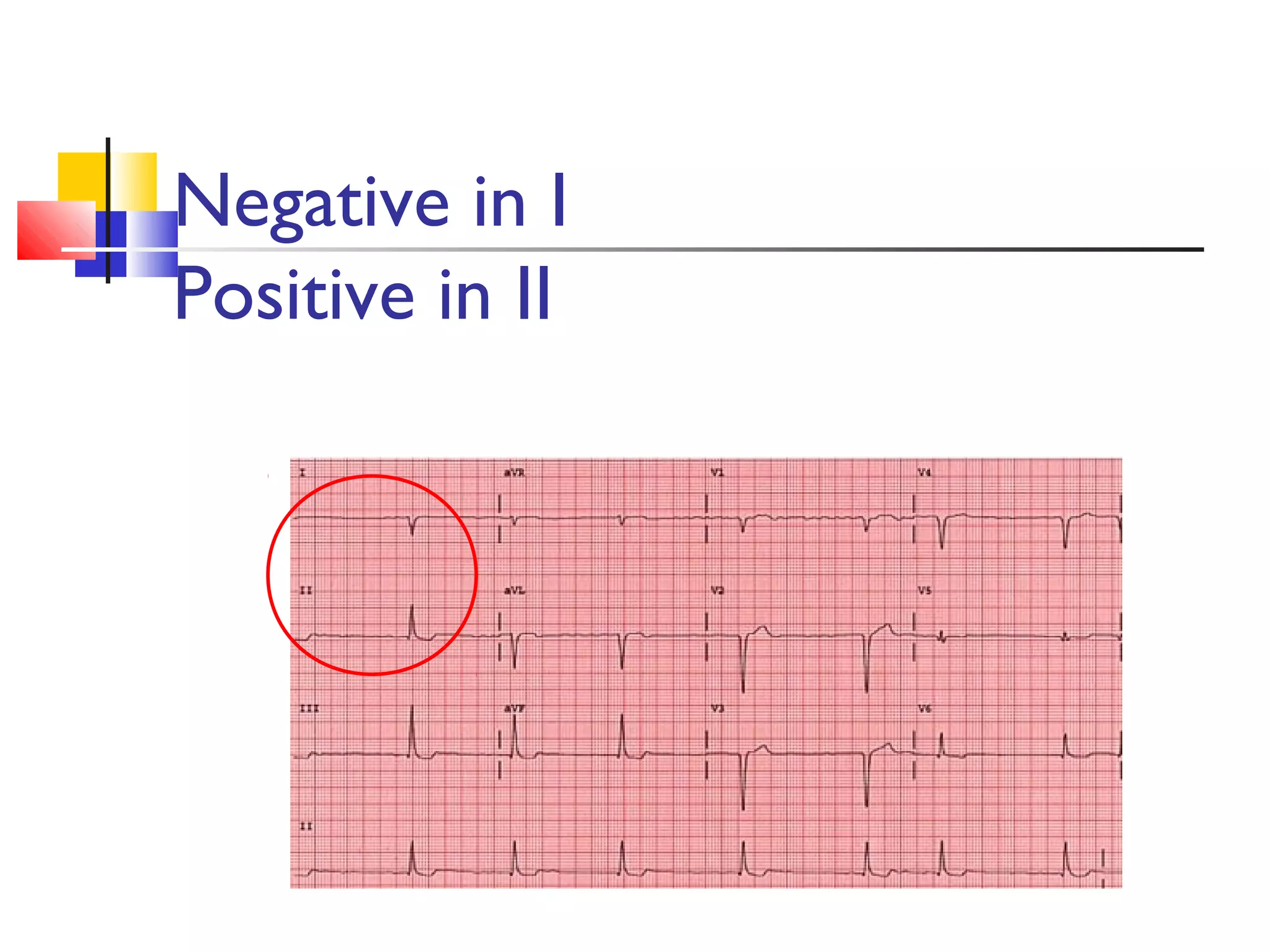
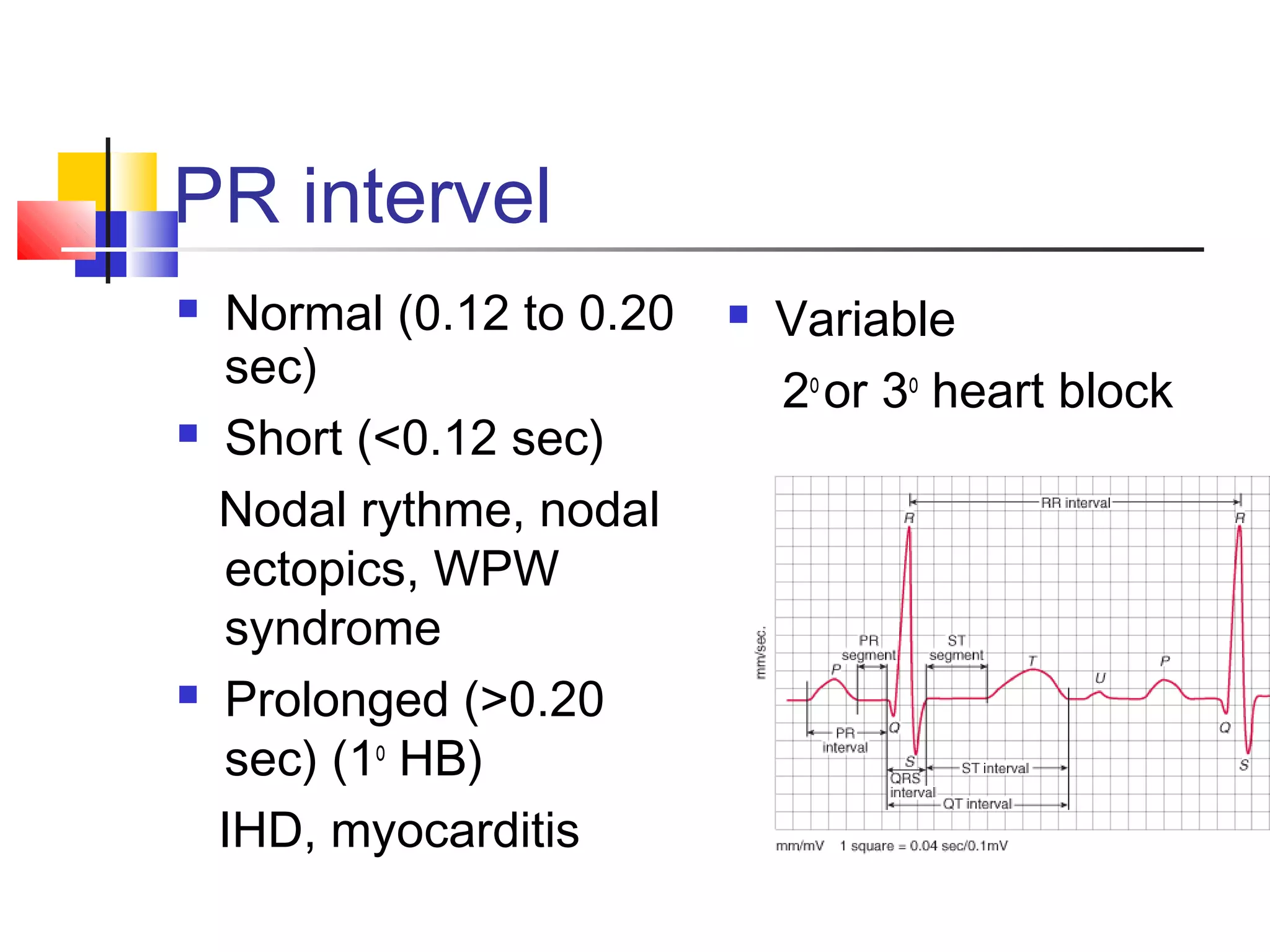
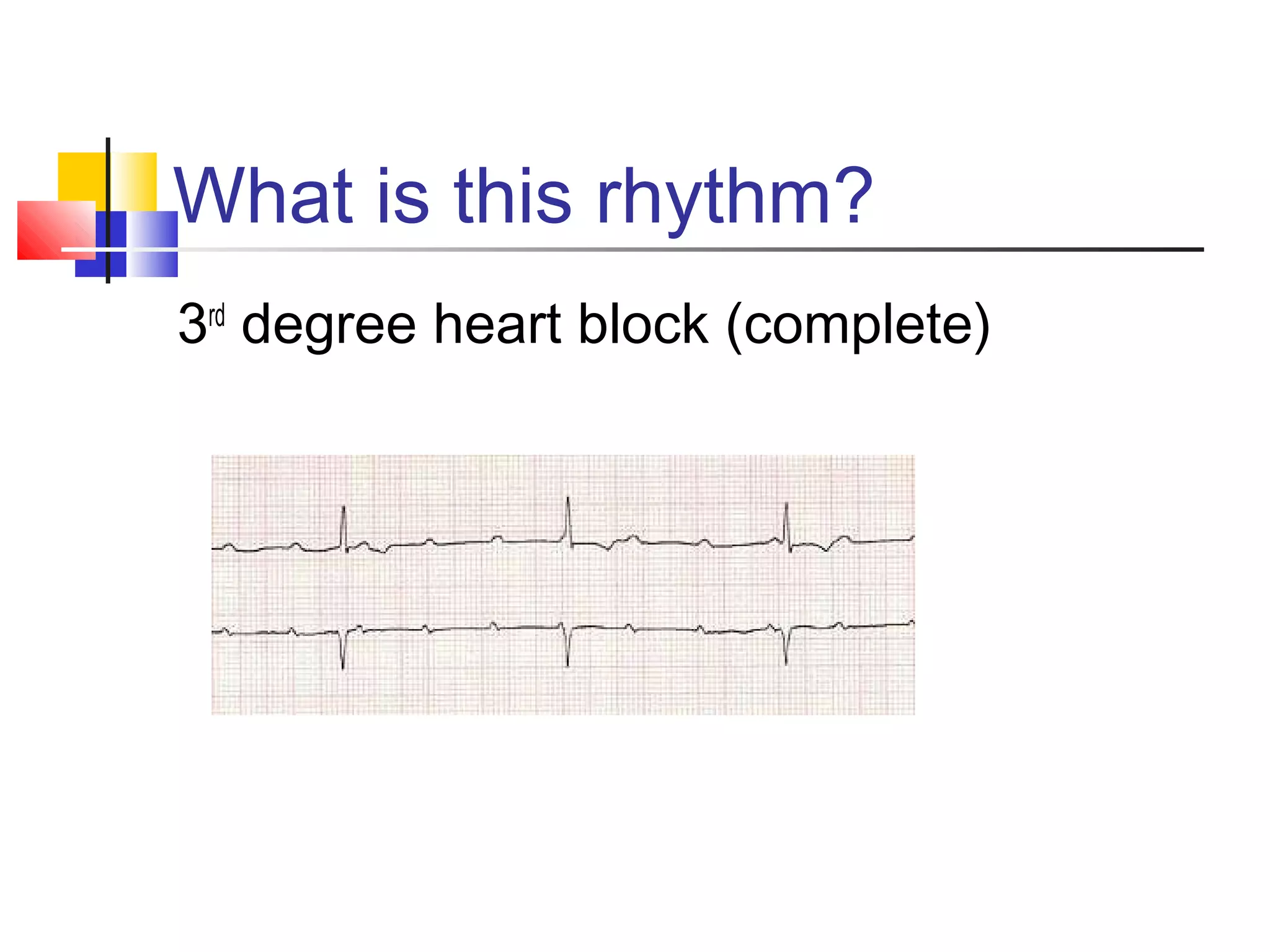
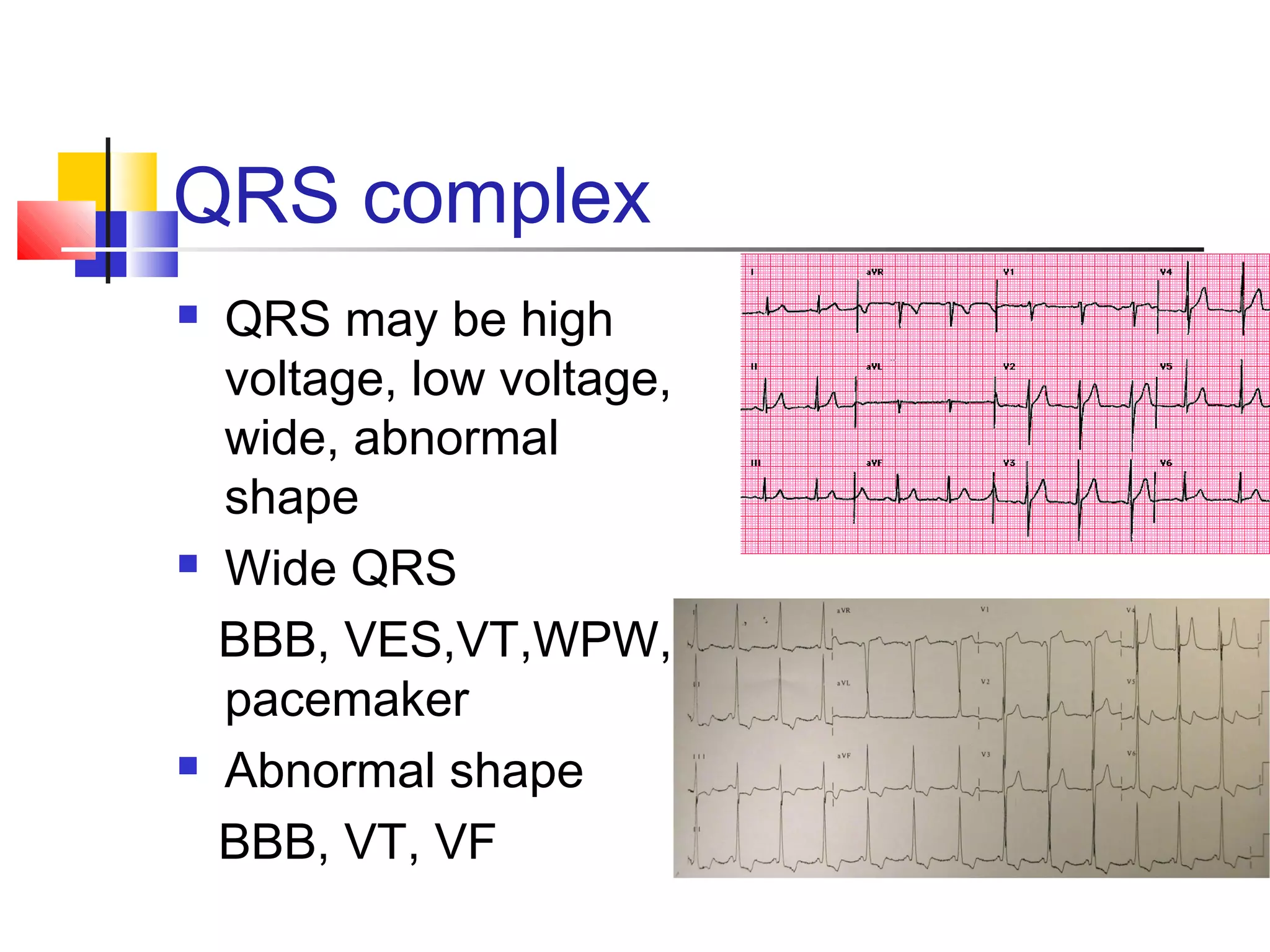
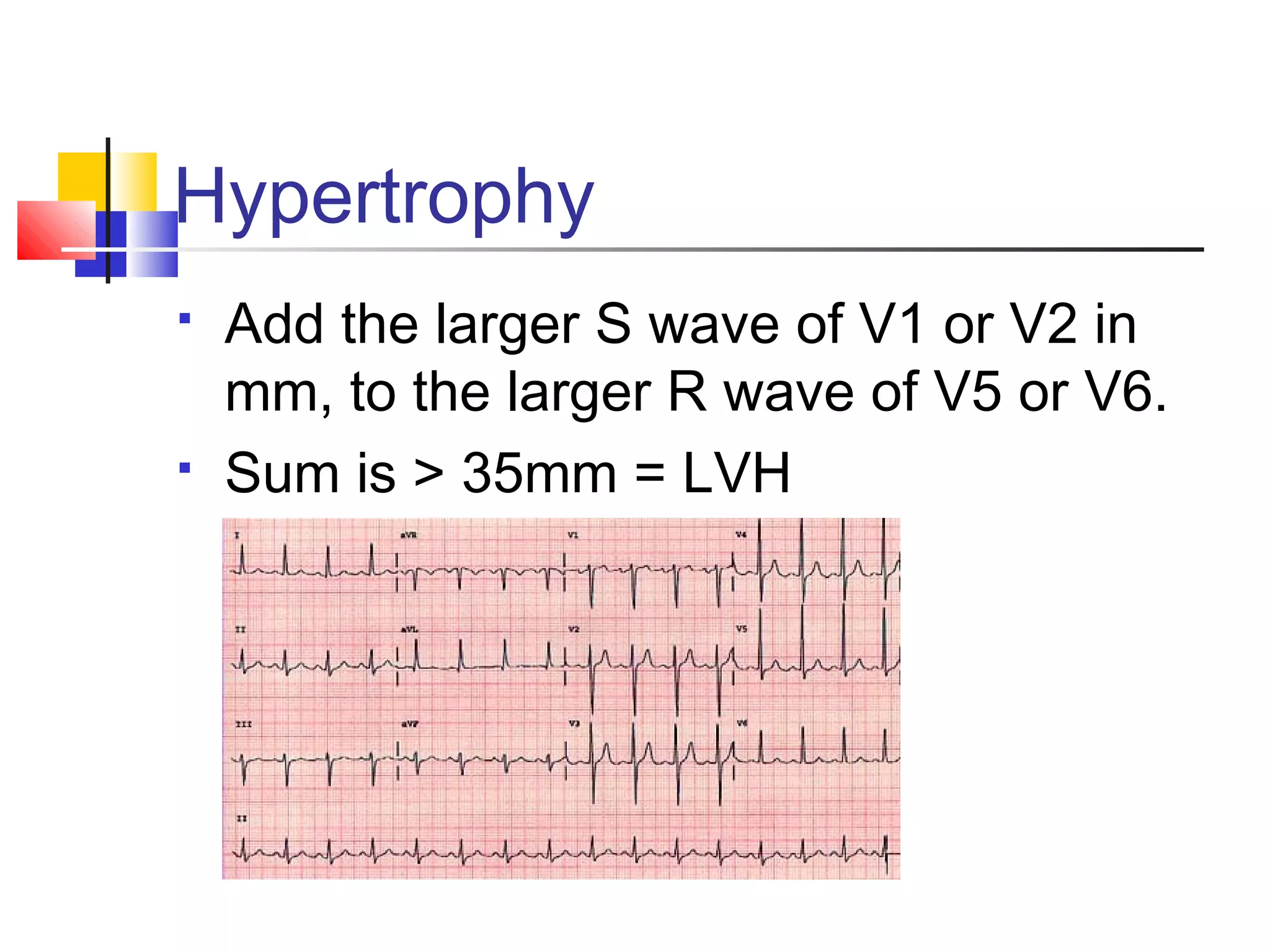
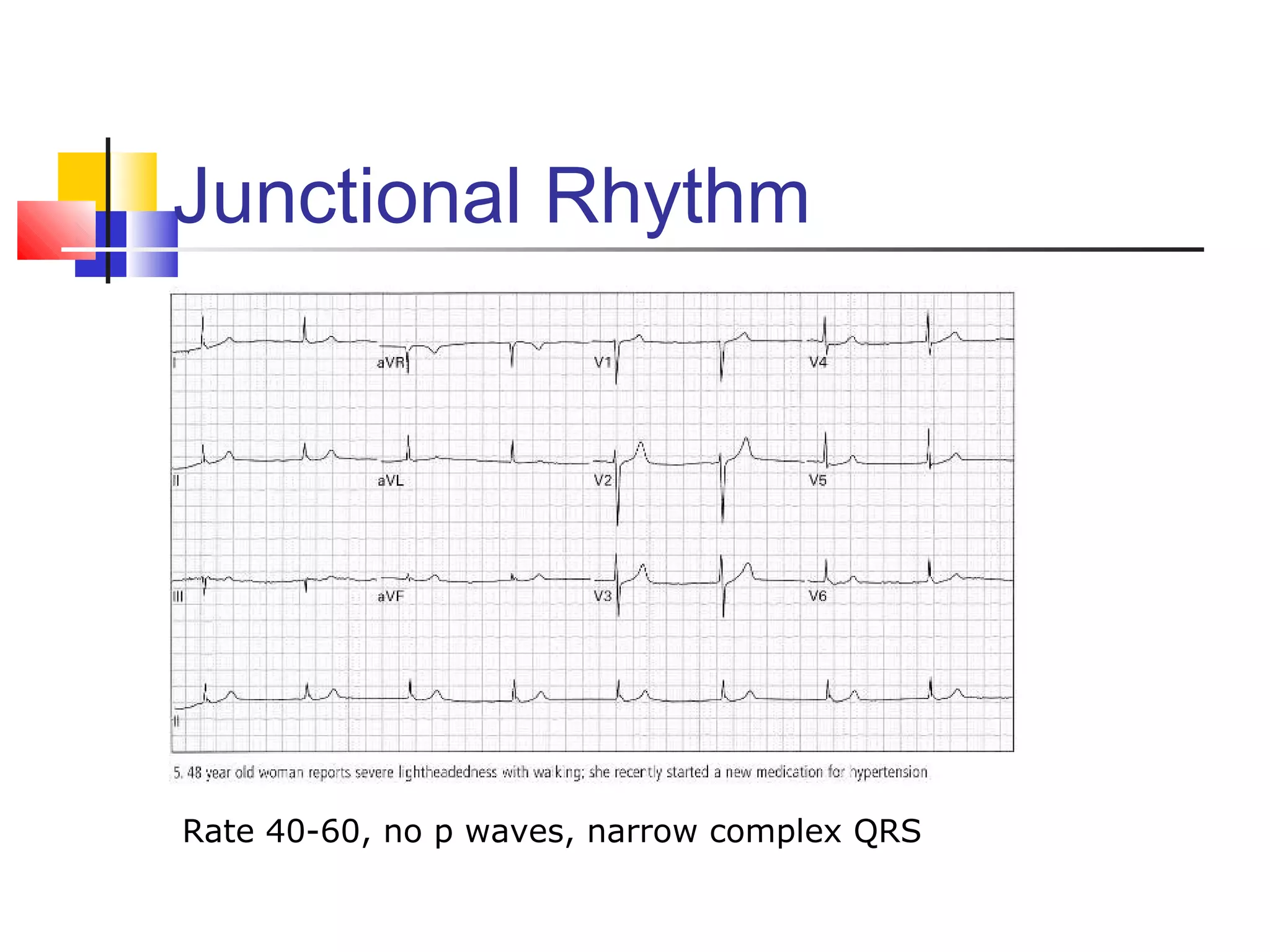
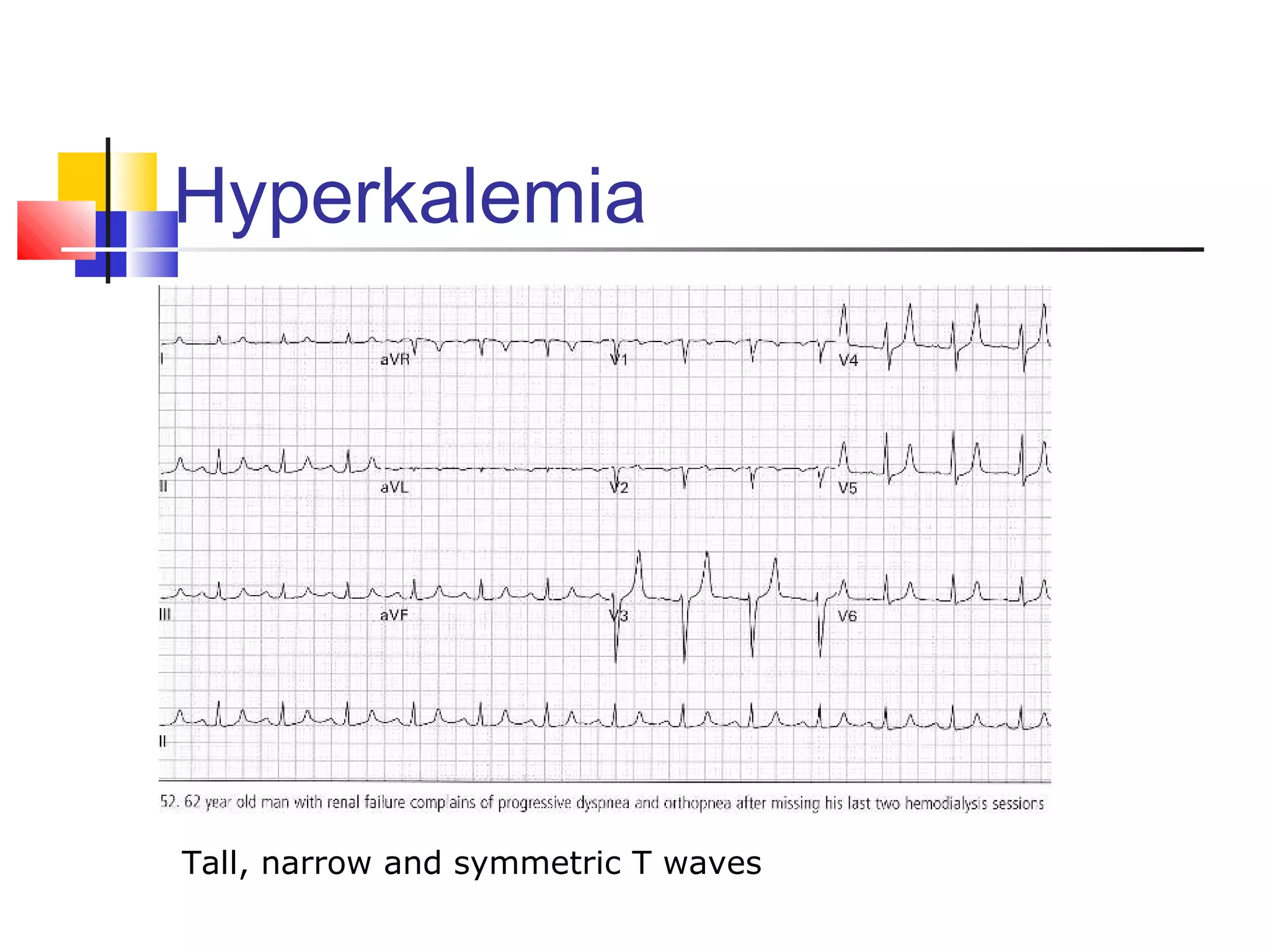
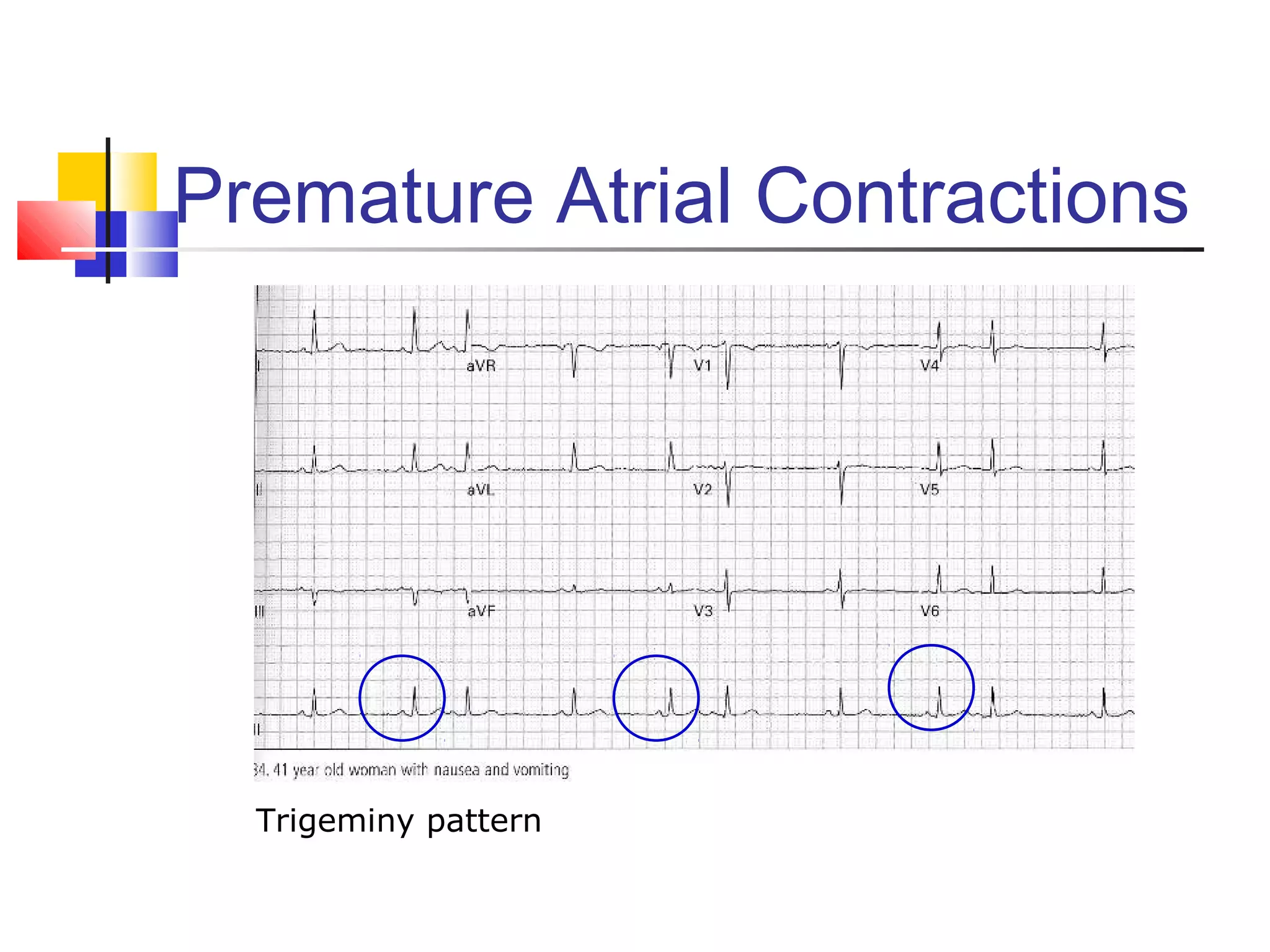
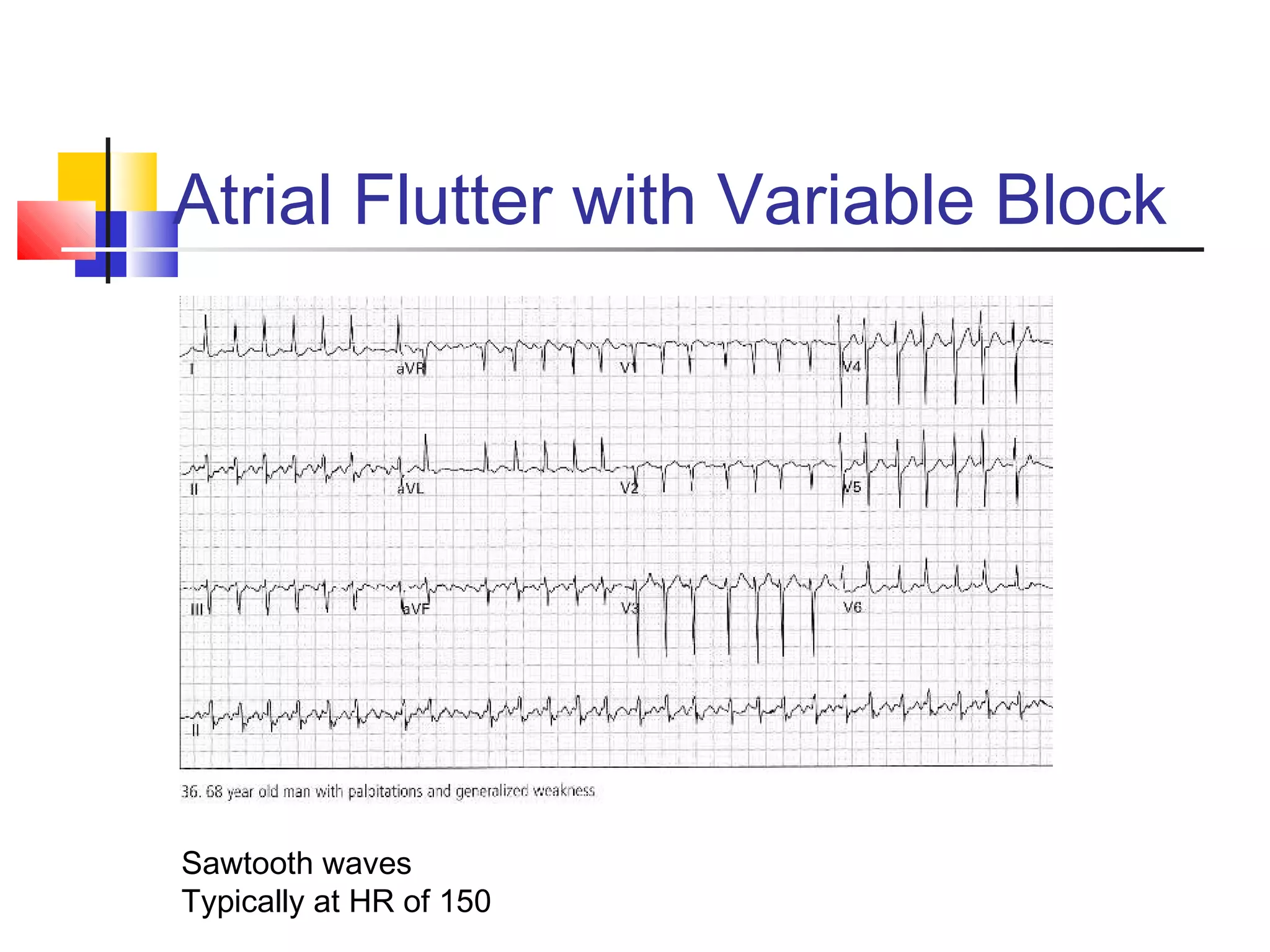
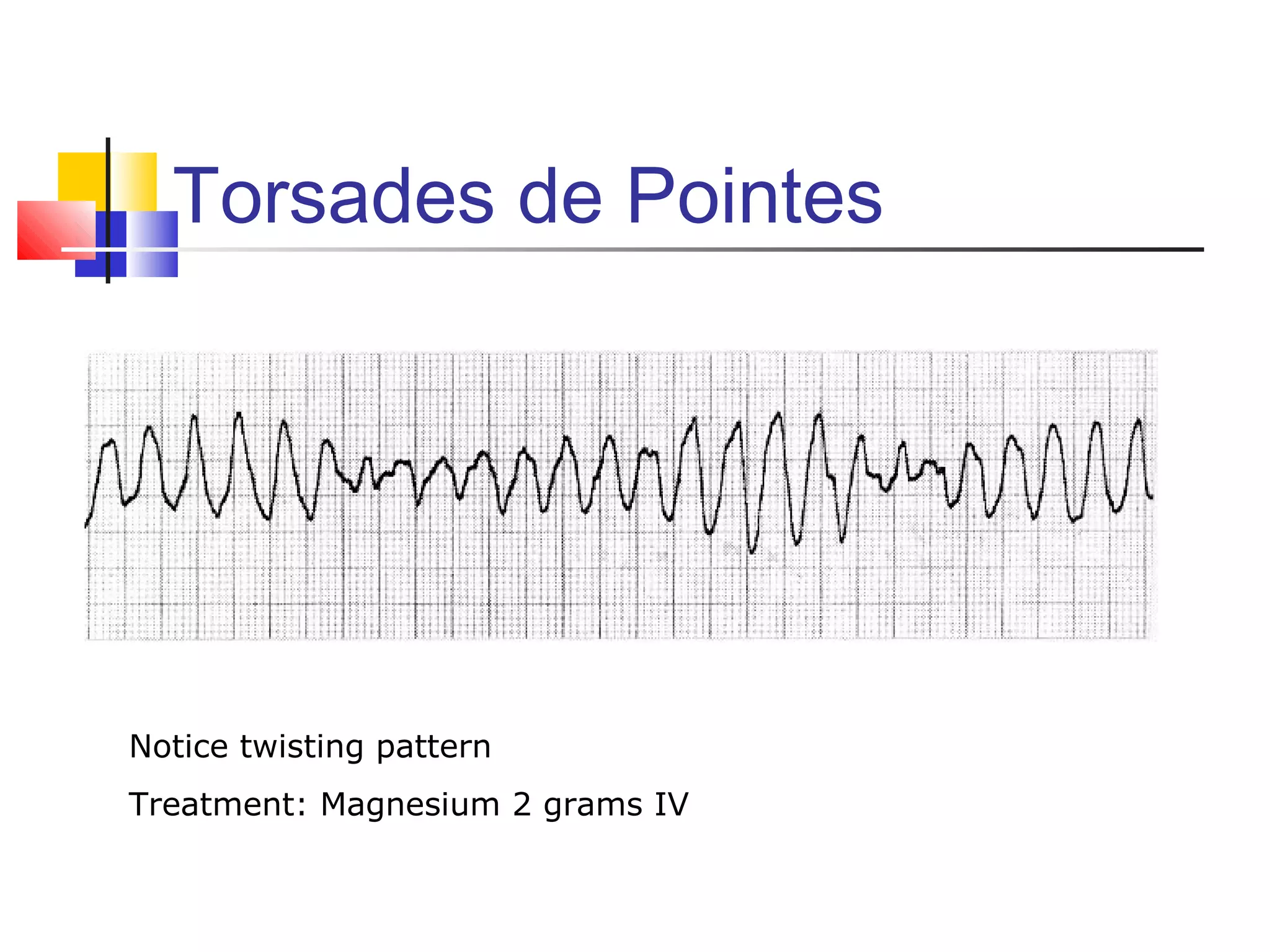
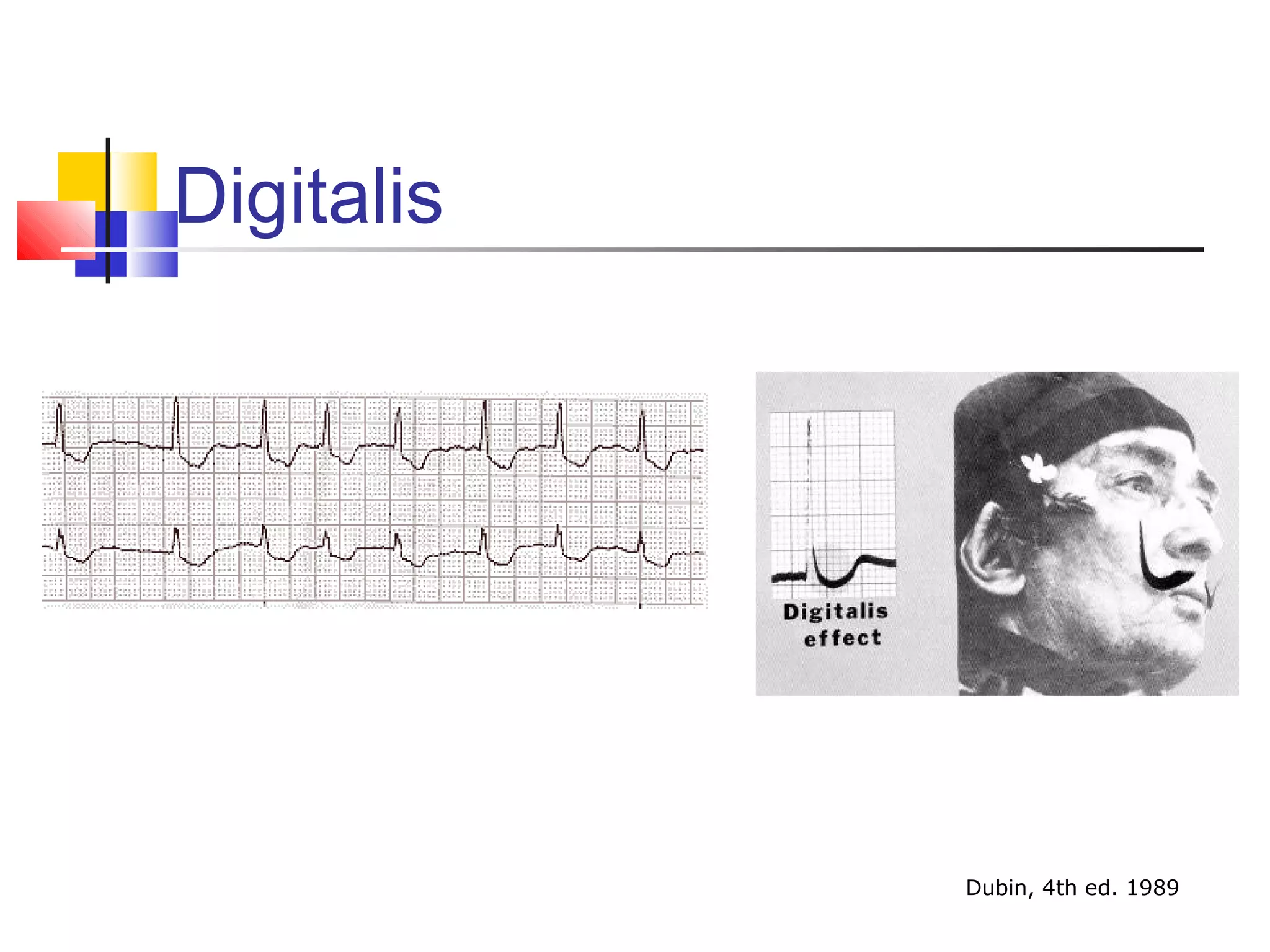
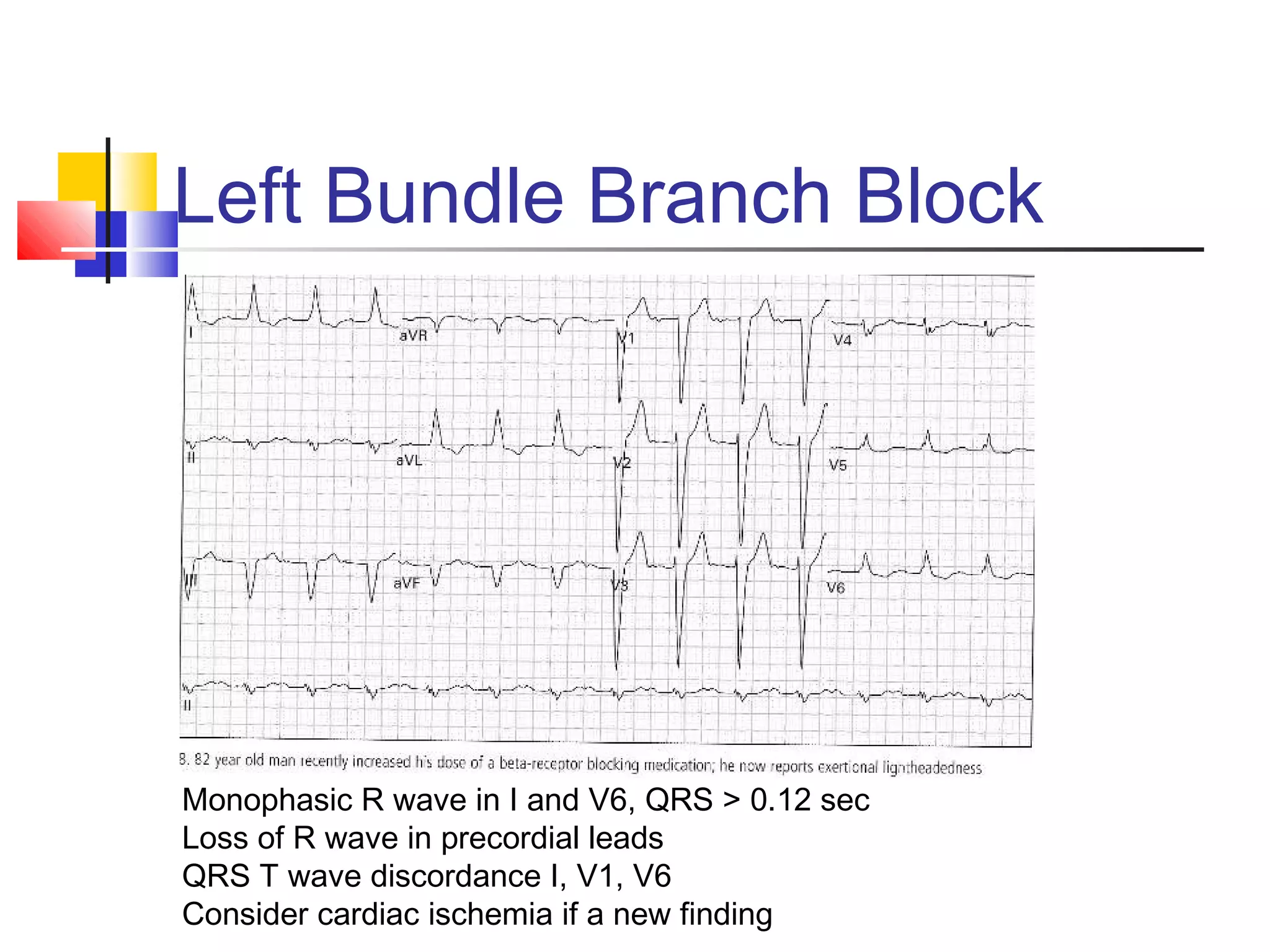
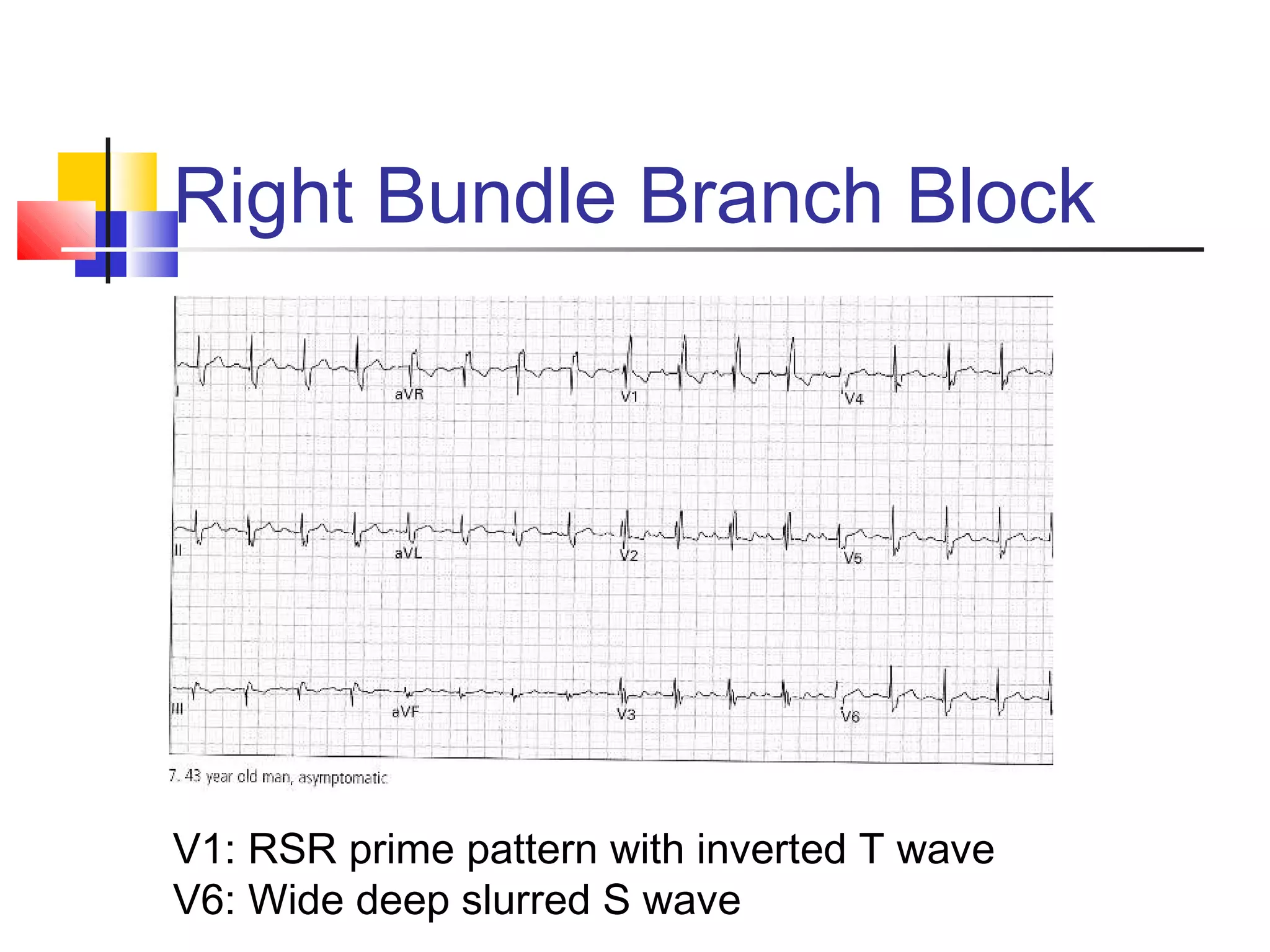
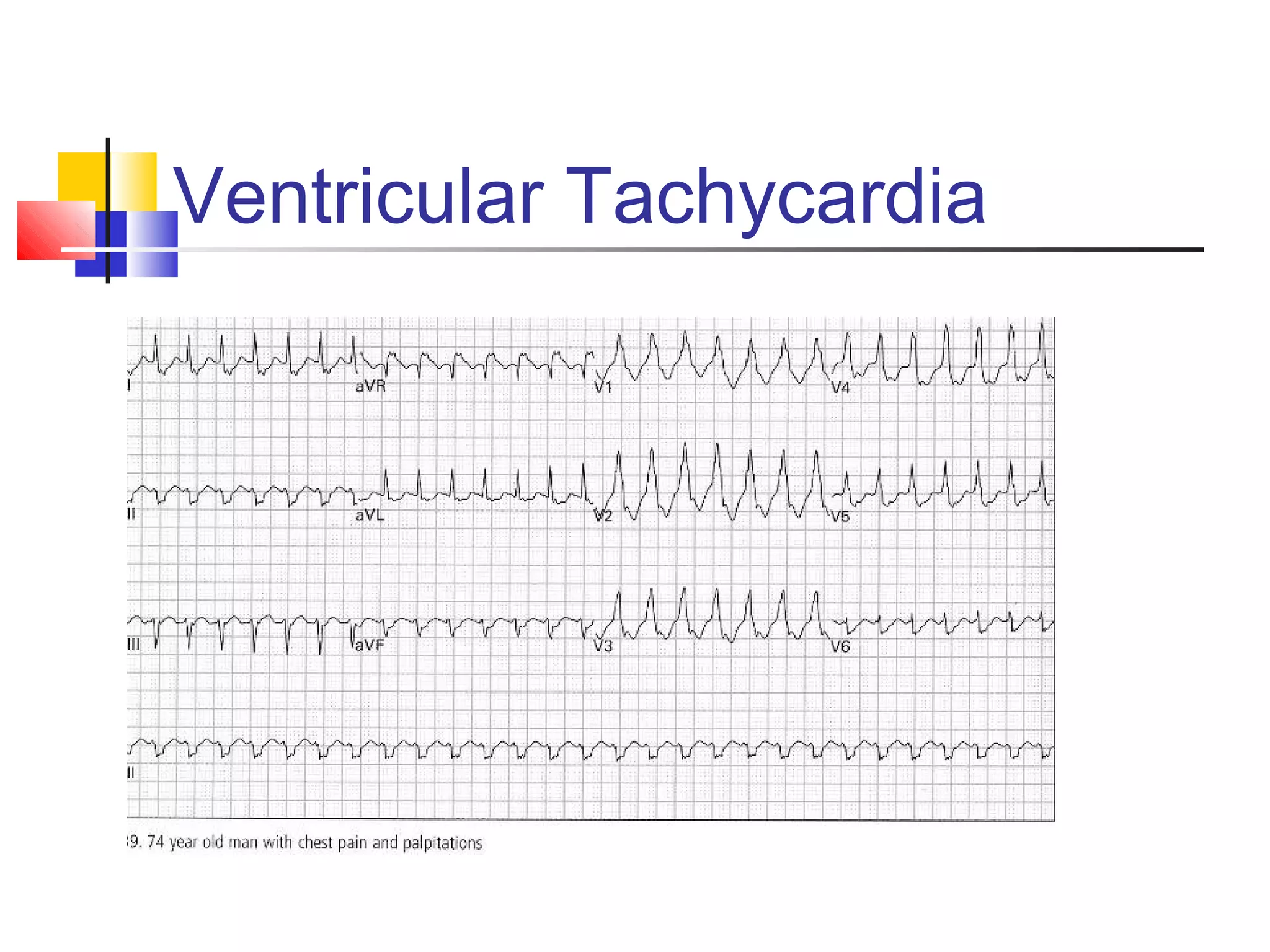
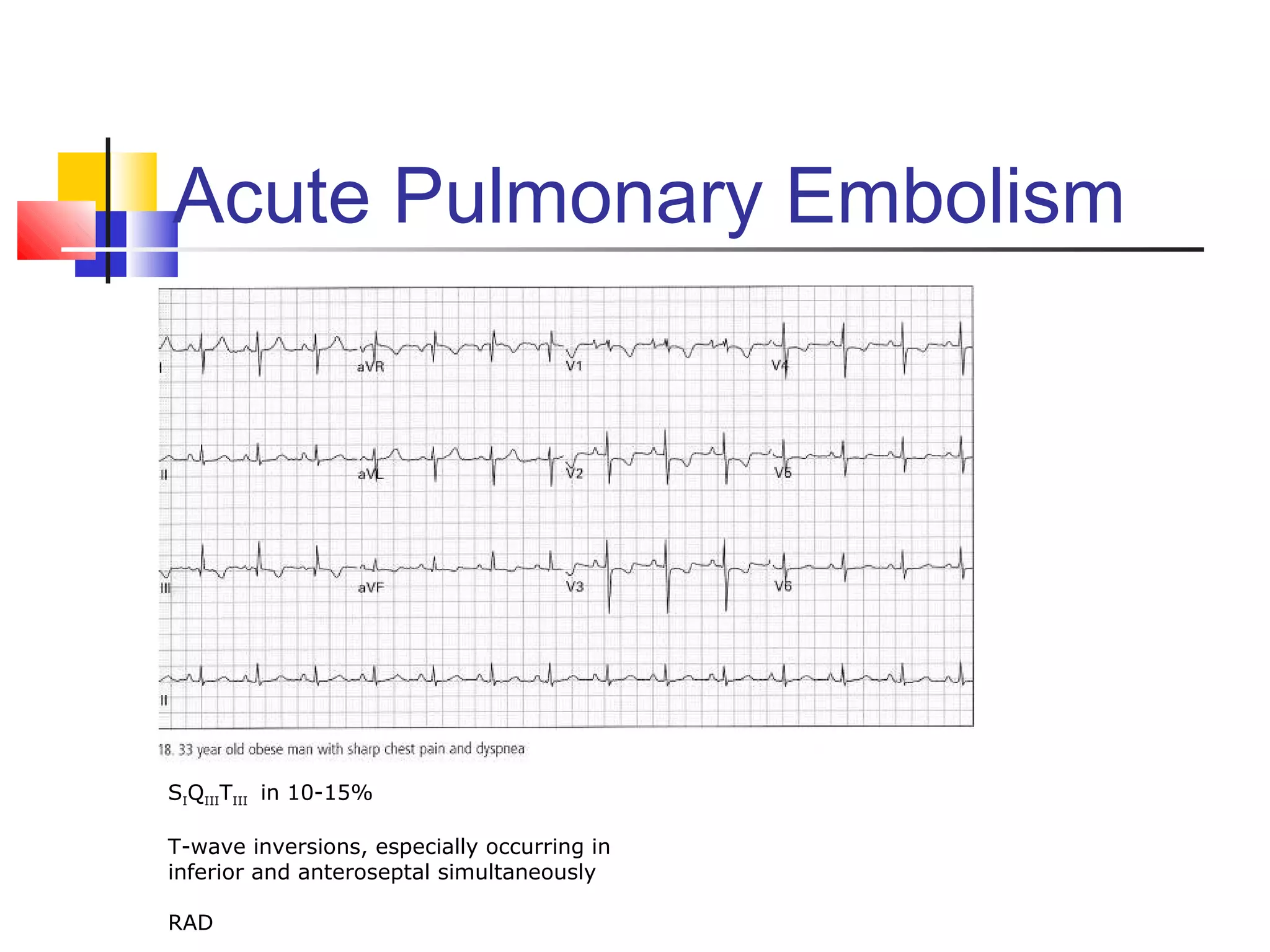
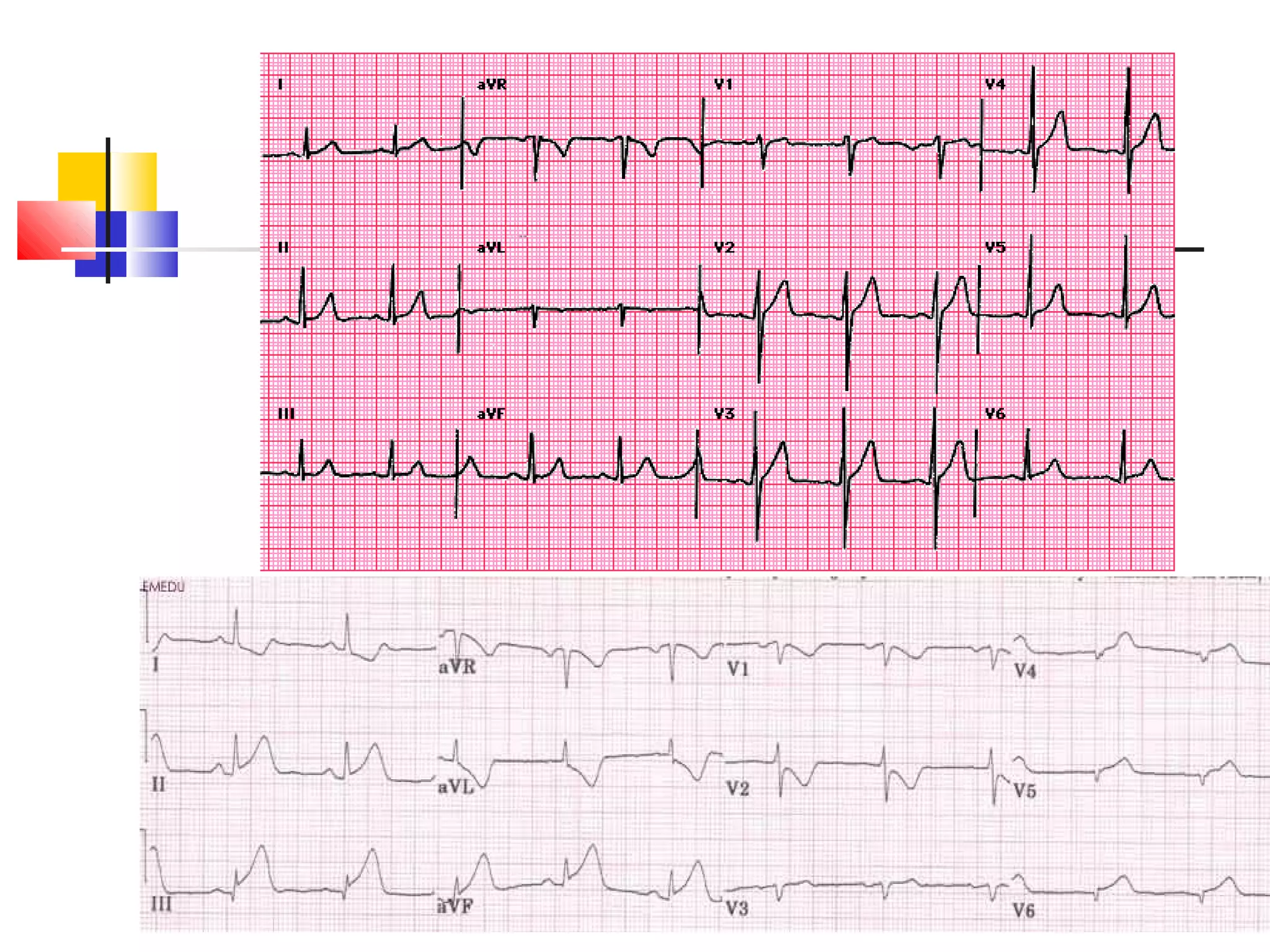
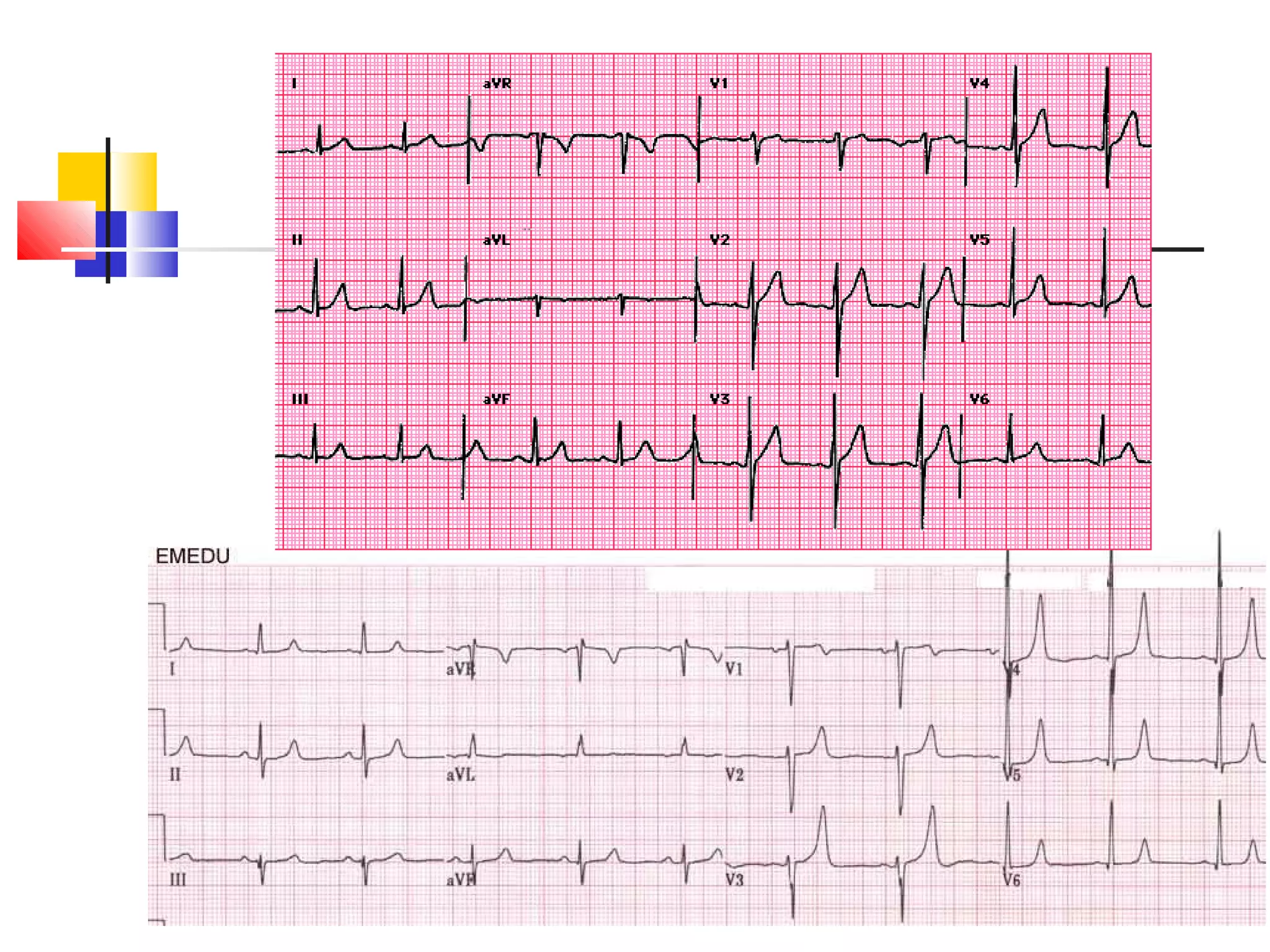
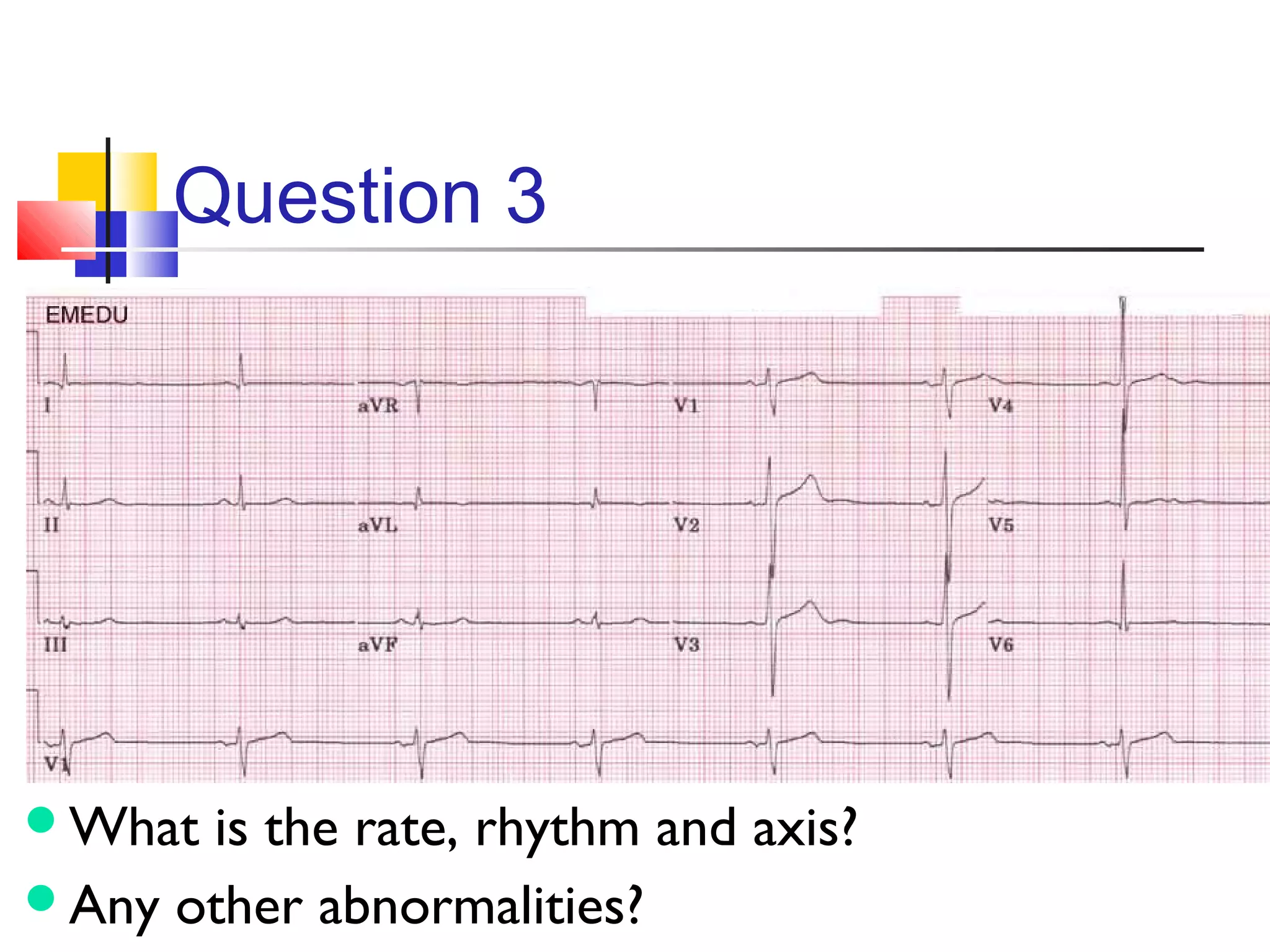
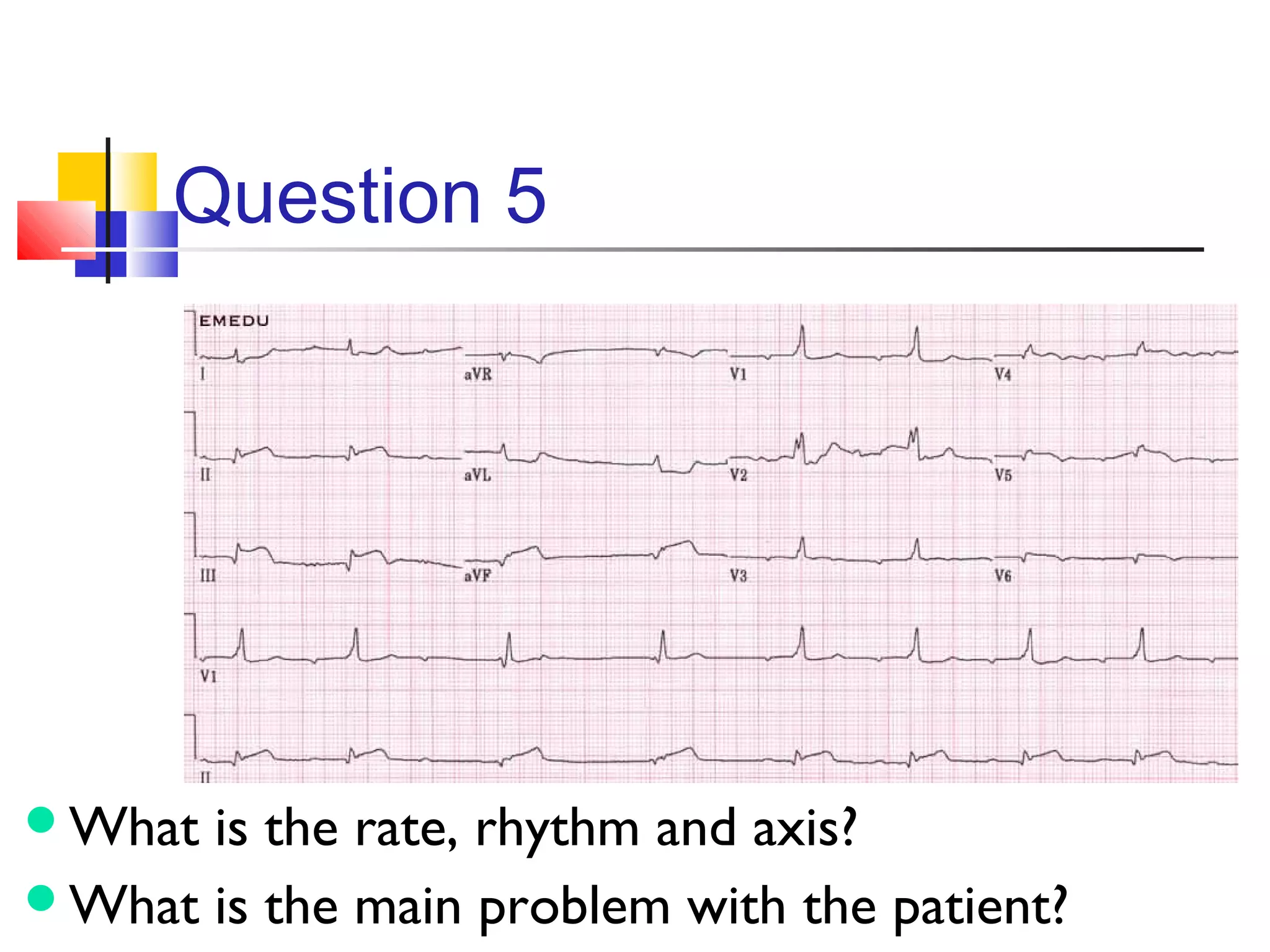
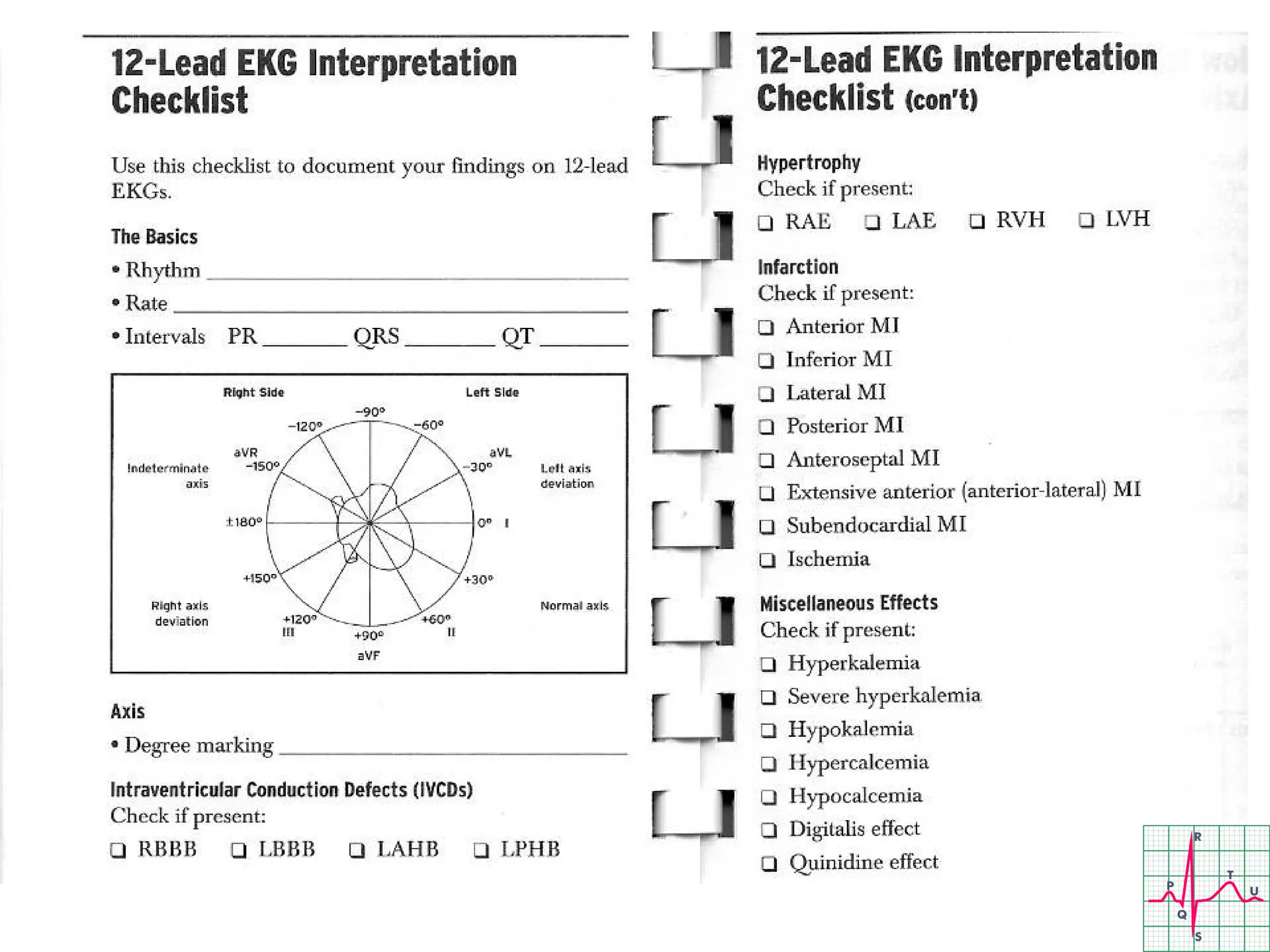
The document provides a comprehensive overview of ECG interpretation, including key concepts such as rate, rhythm, axis, and chamber size assessment. It covers various conditions, waveforms, and physiological principles essential for accurate ECG analysis, as well as guidelines for recognizing abnormalities. Additionally, it highlights important ECG conventions, lead placements, and diagnostic criteria for common cardiovascular issues.