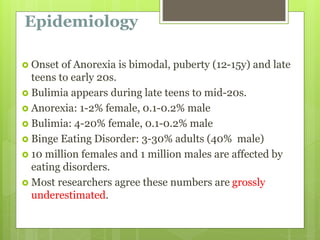
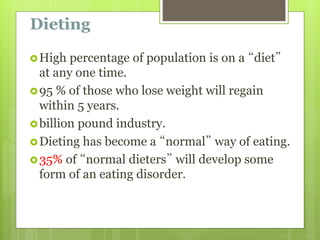
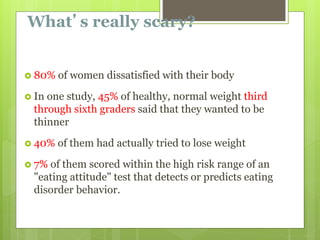
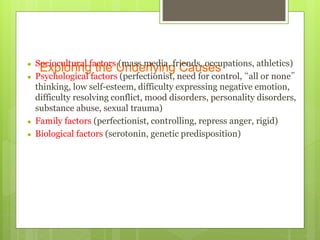
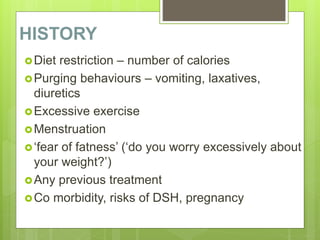
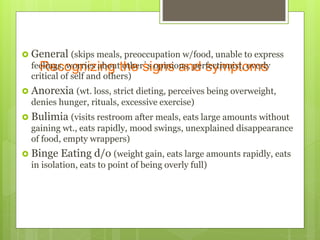
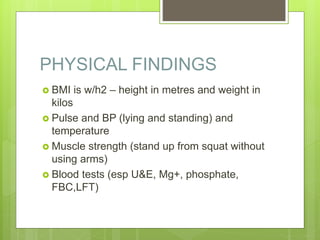
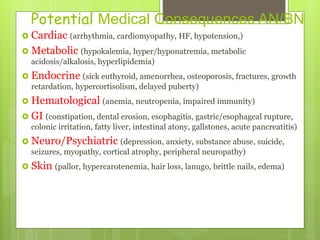
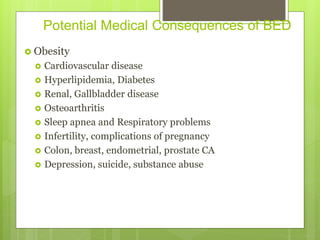
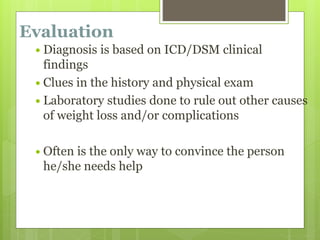
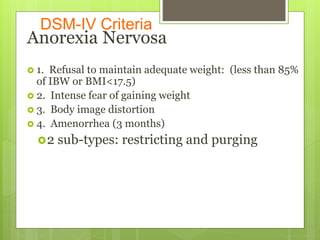
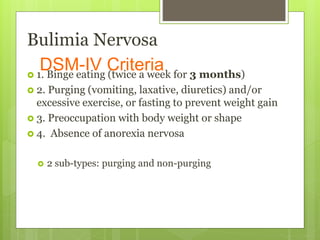
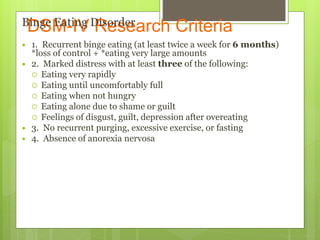
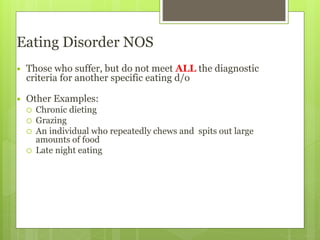
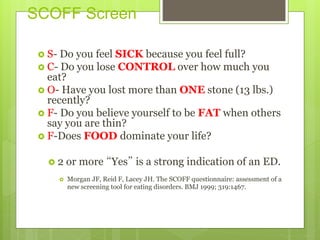
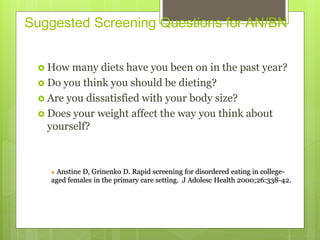
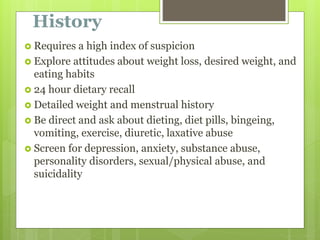
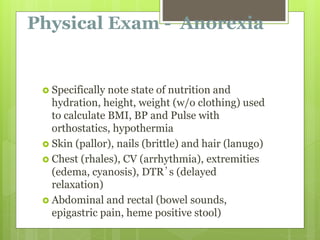
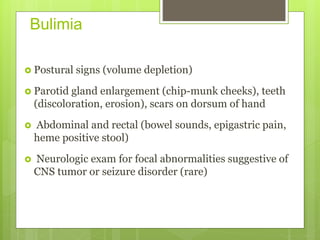
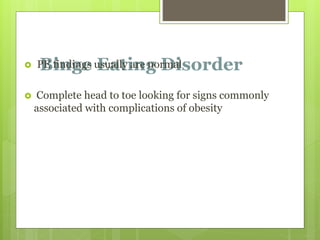
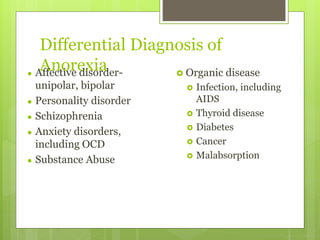
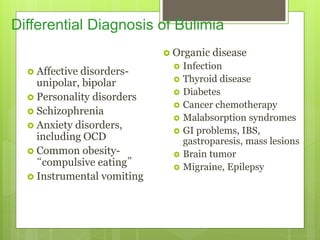
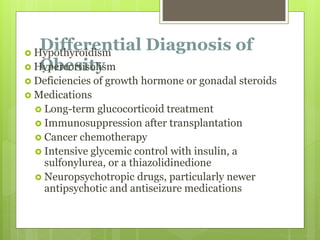
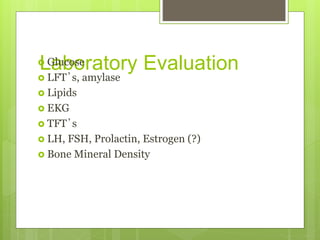
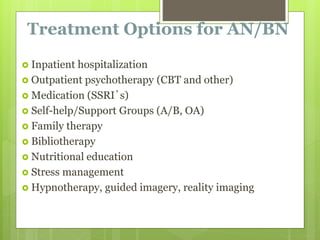
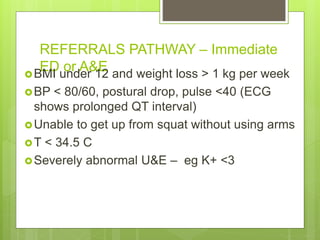
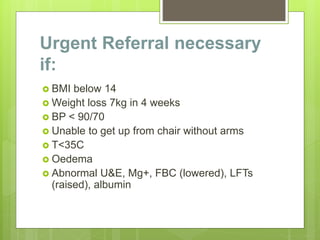
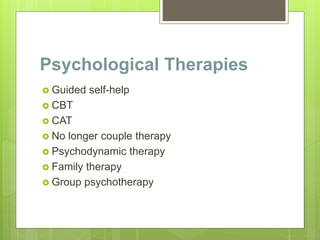
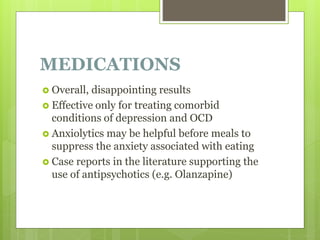
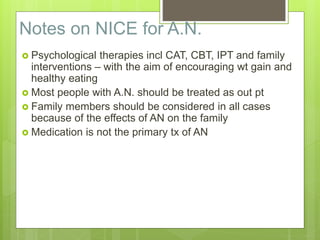
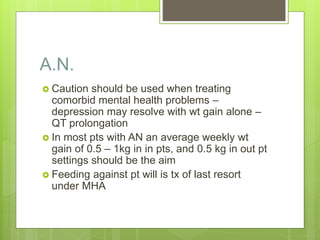
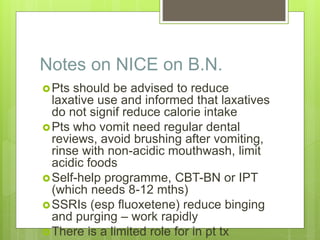
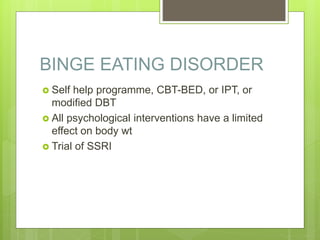
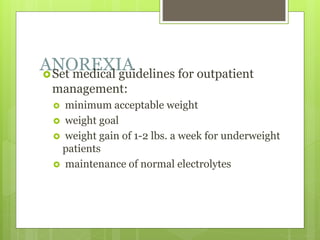
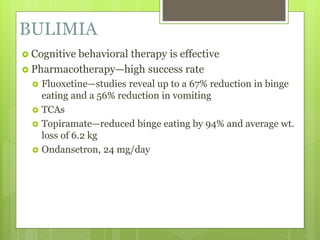
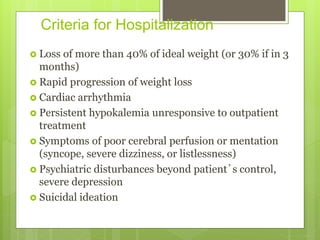
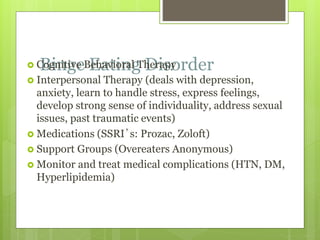
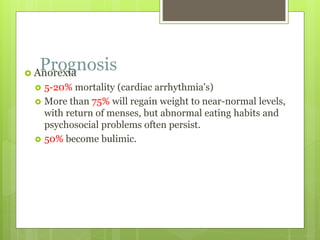
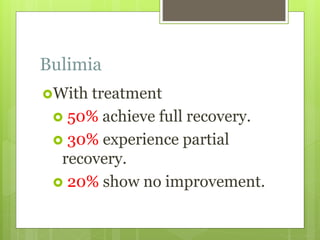
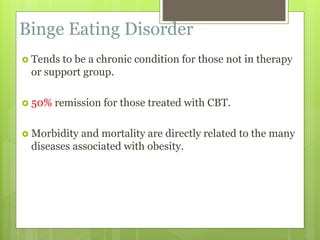
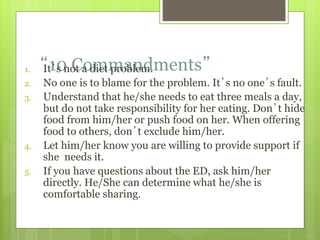
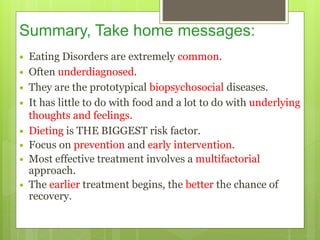
This document discusses eating disorders such as anorexia nervosa, bulimia nervosa, and binge eating disorder. It provides information on the epidemiology, underlying causes, signs and symptoms, medical complications, diagnostic criteria, screening tools, treatment options, and the role of primary care providers in managing these conditions. Eating disorders typically have an onset during adolescence or young adulthood and disproportionately affect females. Treatment involves a multidisciplinary team approach including medical monitoring, nutritional counseling, and psychological therapies like CBT.