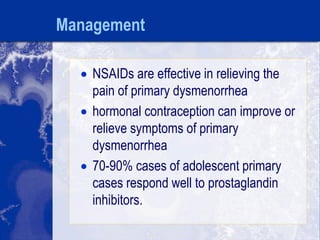
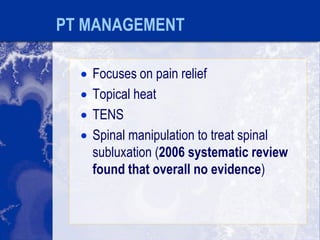
Dysmenorrhea is a medical condition that causes painful menstruation interfering with daily activities. It can feature sharp, throbbing, or dull pain in the lower abdomen that may precede or accompany menstruation. Dysmenorrhea is classified as primary, caused by excessive prostaglandins, or secondary, caused by underlying conditions like endometriosis. Common symptoms include abdominal pain, nausea, and fatigue. Treatment focuses on pain relief and includes NSAIDs, hormonal contraception, alternative therapies, and physical therapy.