This document discusses approaches to designing dosage regimens and individualizing dosage regimens for patients. It covers topics like dose size and frequency, drug accumulation during multiple dosing, loading and maintenance doses, sources of variability between patients, and dosing considerations for specific patient populations like neonates/children, elderly patients, and patients with renal or hepatic impairment. The key approaches discussed are empirical dosage regimens, individualized regimens based on pharmacokinetics, and regimens based on population averages using fixed or adaptive models.













![ Maintenance Dose :
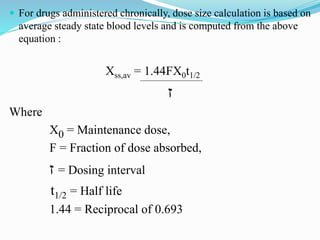
A maintenance dose is the maintenance rate [mg/h] of drug
administered equal to the rate of elimination at steady state. It is also
defined as the amount of drug required to keep a desired mean steady
state concentration in the tissues. It is administered after L.D.
Calculation of Maintenance Dose :
The required maintenance dose may be calculated as :
MD = CpCL
F
Where,
MD – Maintenance dose rate (mg/L)
Cp – desired peak Conc. Of drug (mg/l)
CL – Clearance of drug in body and F – Bioavailability.](https://image.slidesharecdn.com/dosageregimen-220825011407-2c12307a/85/dosage-regimen-pptx-15-320.jpg)



























