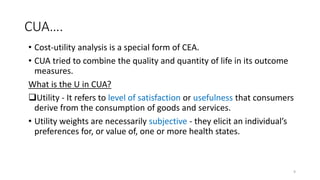
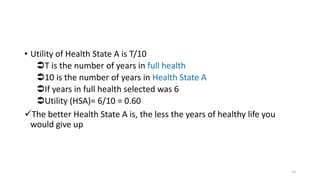
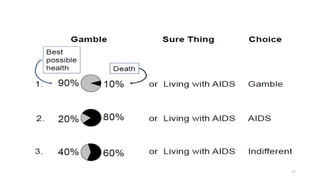
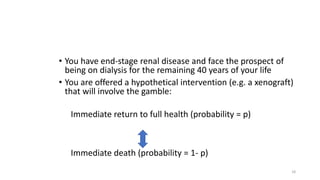
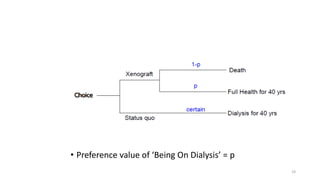
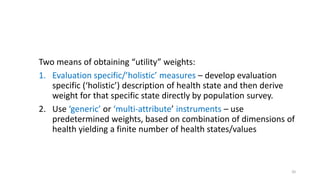
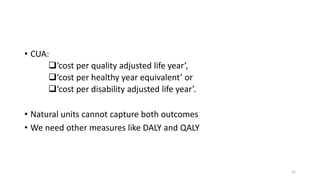
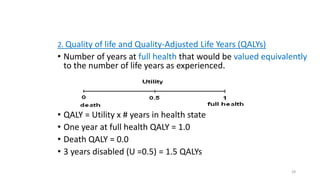
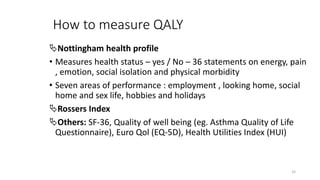
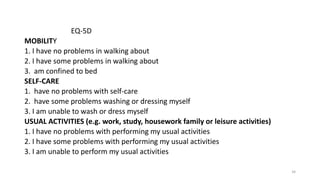
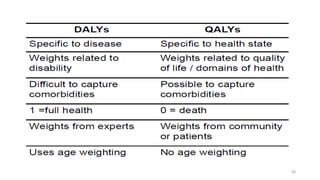
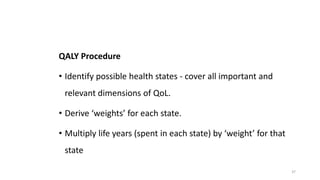
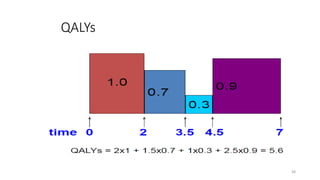
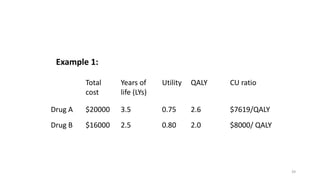
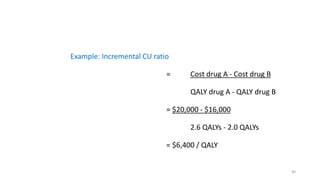
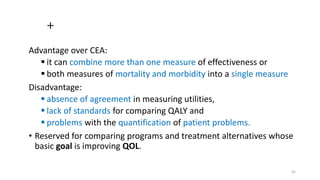
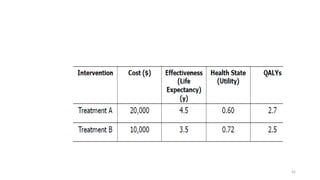
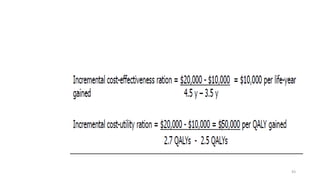
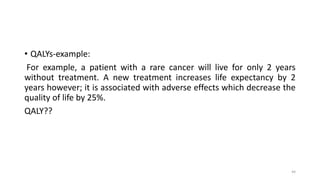
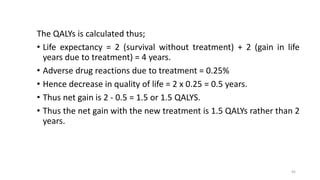
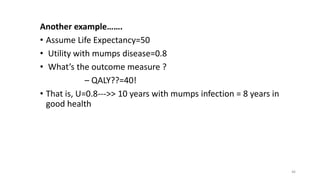
Cost-utility analysis (CUA) is a type of economic analysis that compares treatment alternatives by integrating measures of patient preferences and health-related quality of life. CUA uses quality-adjusted life years (QALYs) as the measure of health outcome, which combines both quantity and quality of life into a single metric. The preferred treatment is the one with the lowest cost per QALY gained. QALYs are calculated by multiplying the expected survival time in a health state by a weight representing the quality of life in that health state on a scale of 0 to 1, with 0 being death and 1 being perfect health. CUA allows for comparison of interventions that impact both mortality and morbidity.