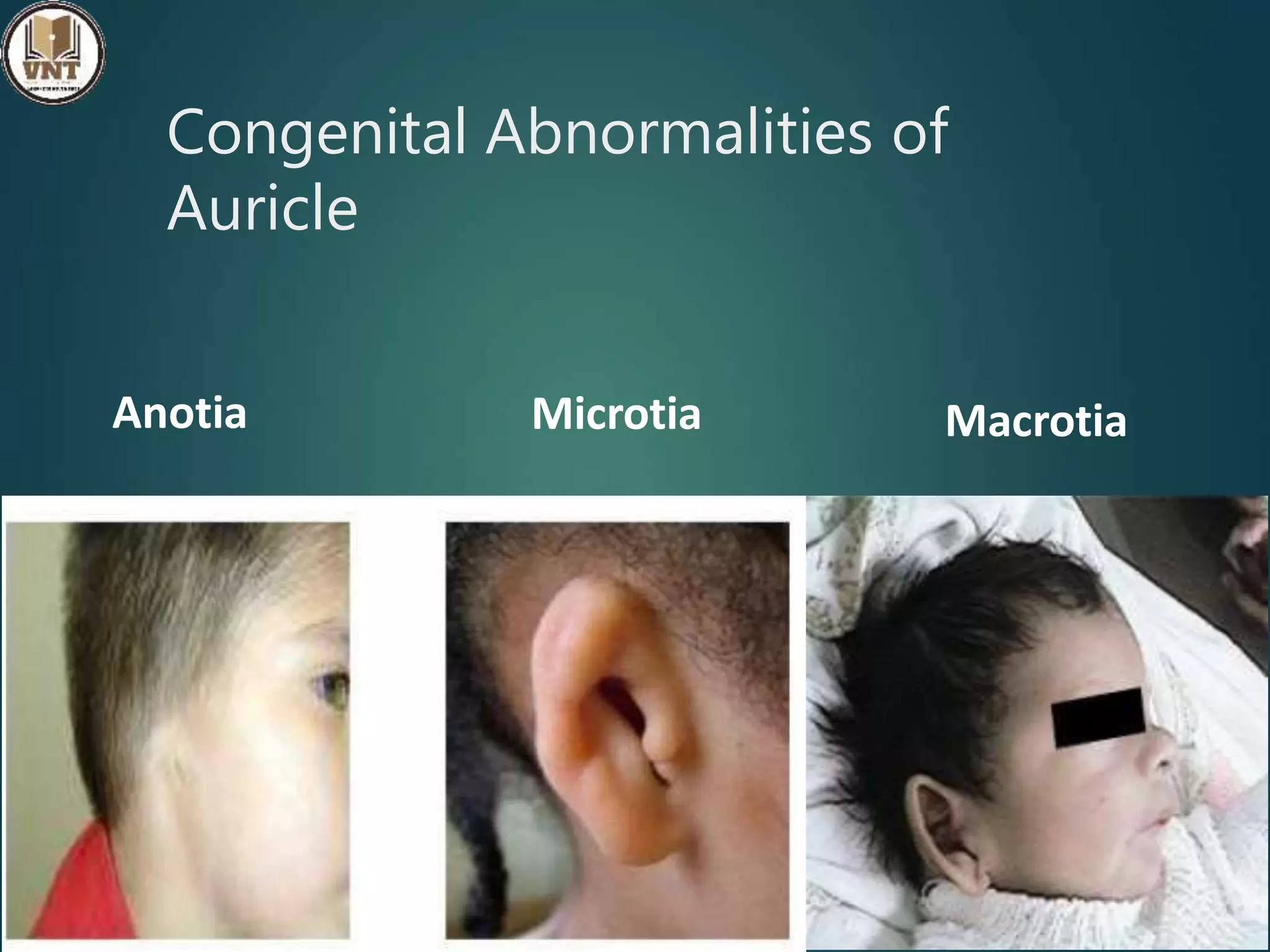
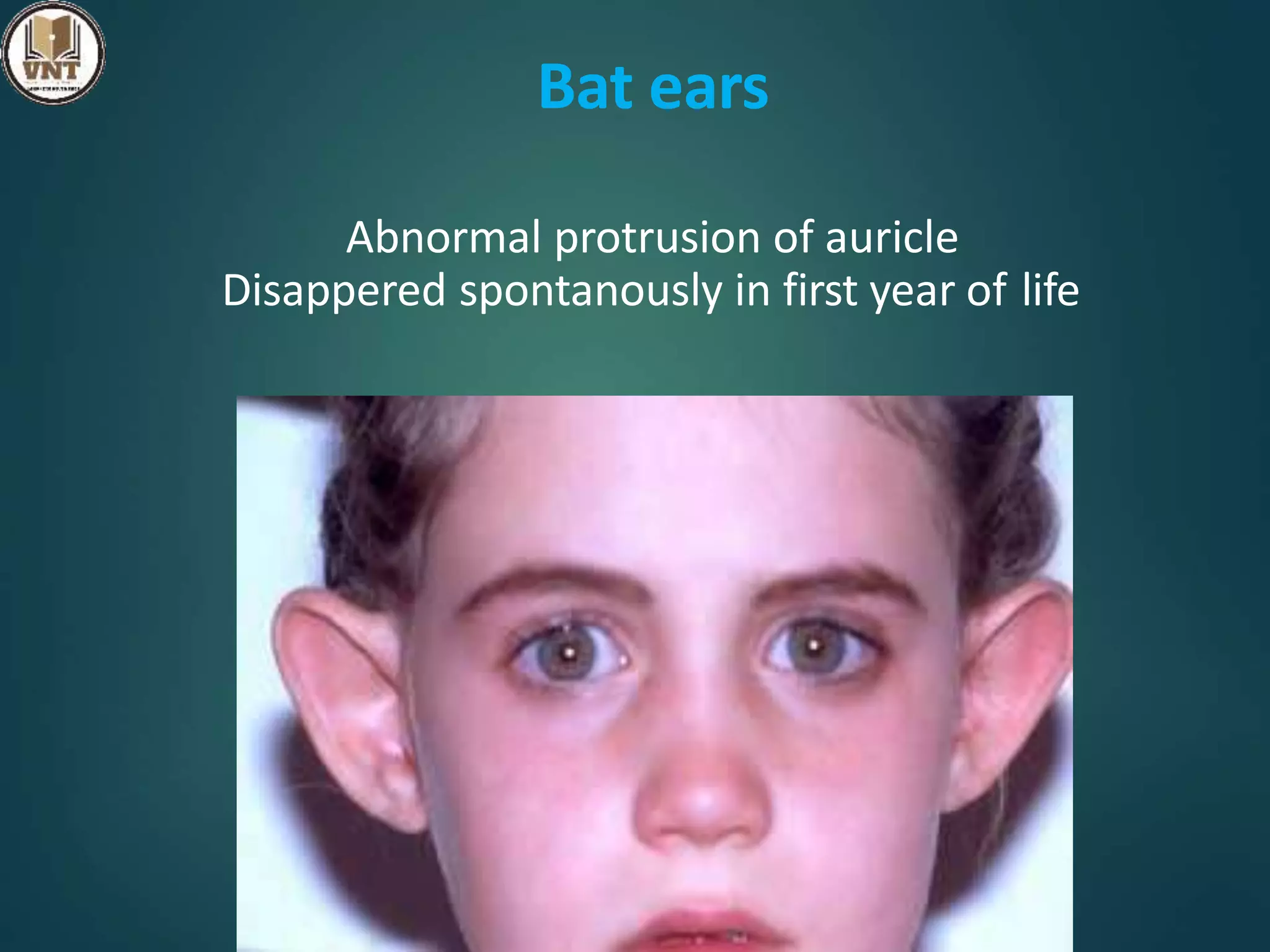
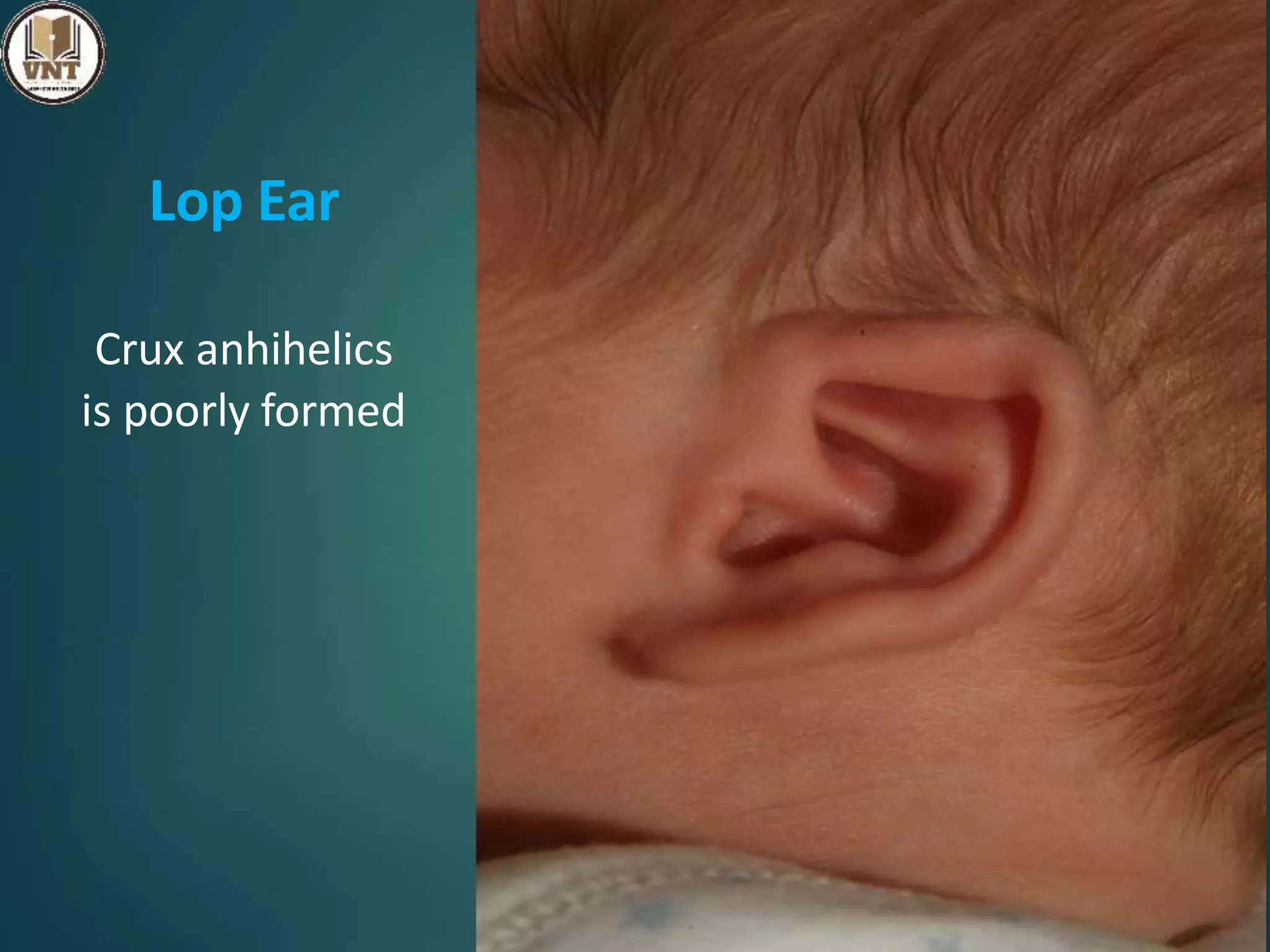
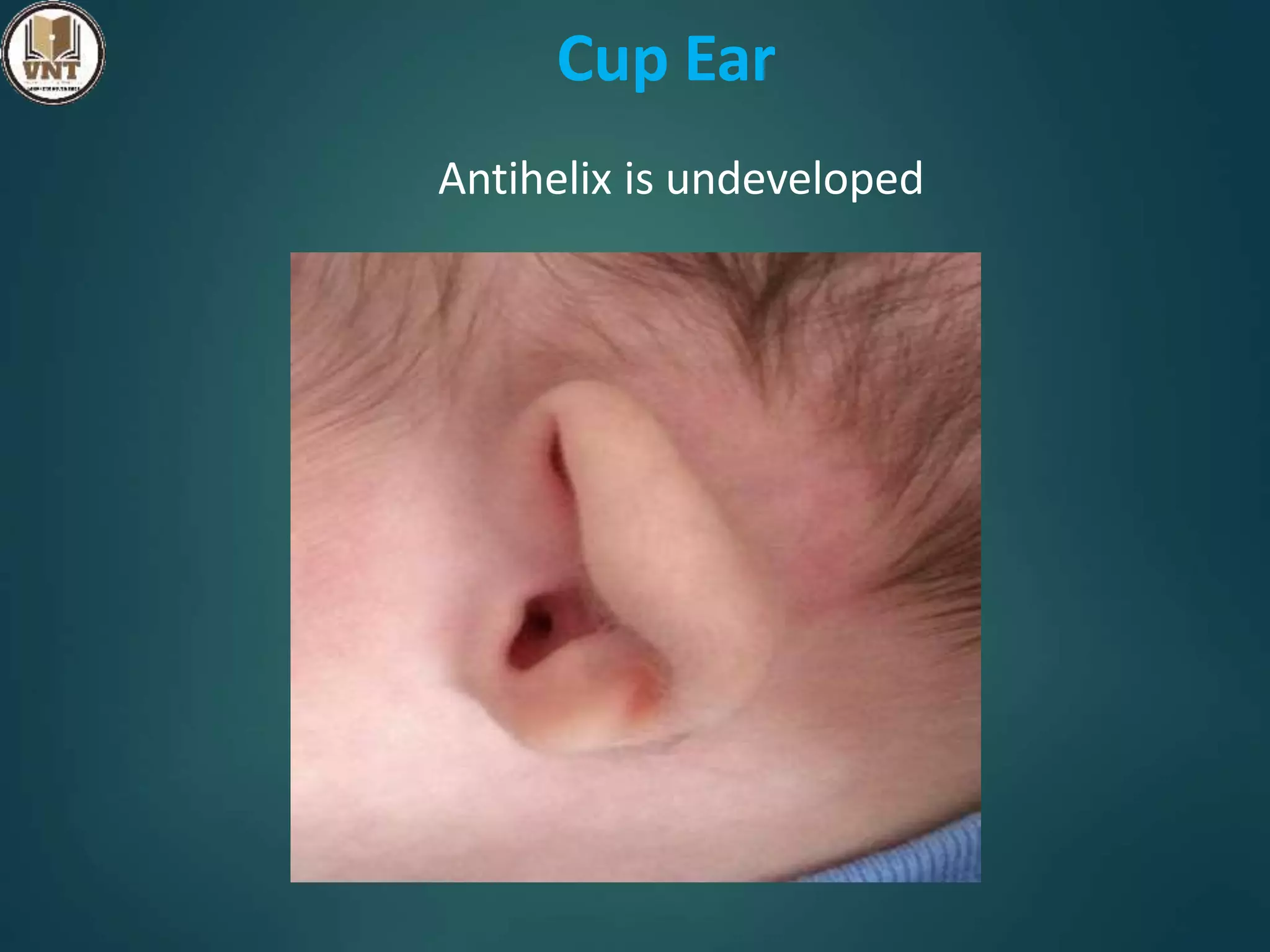
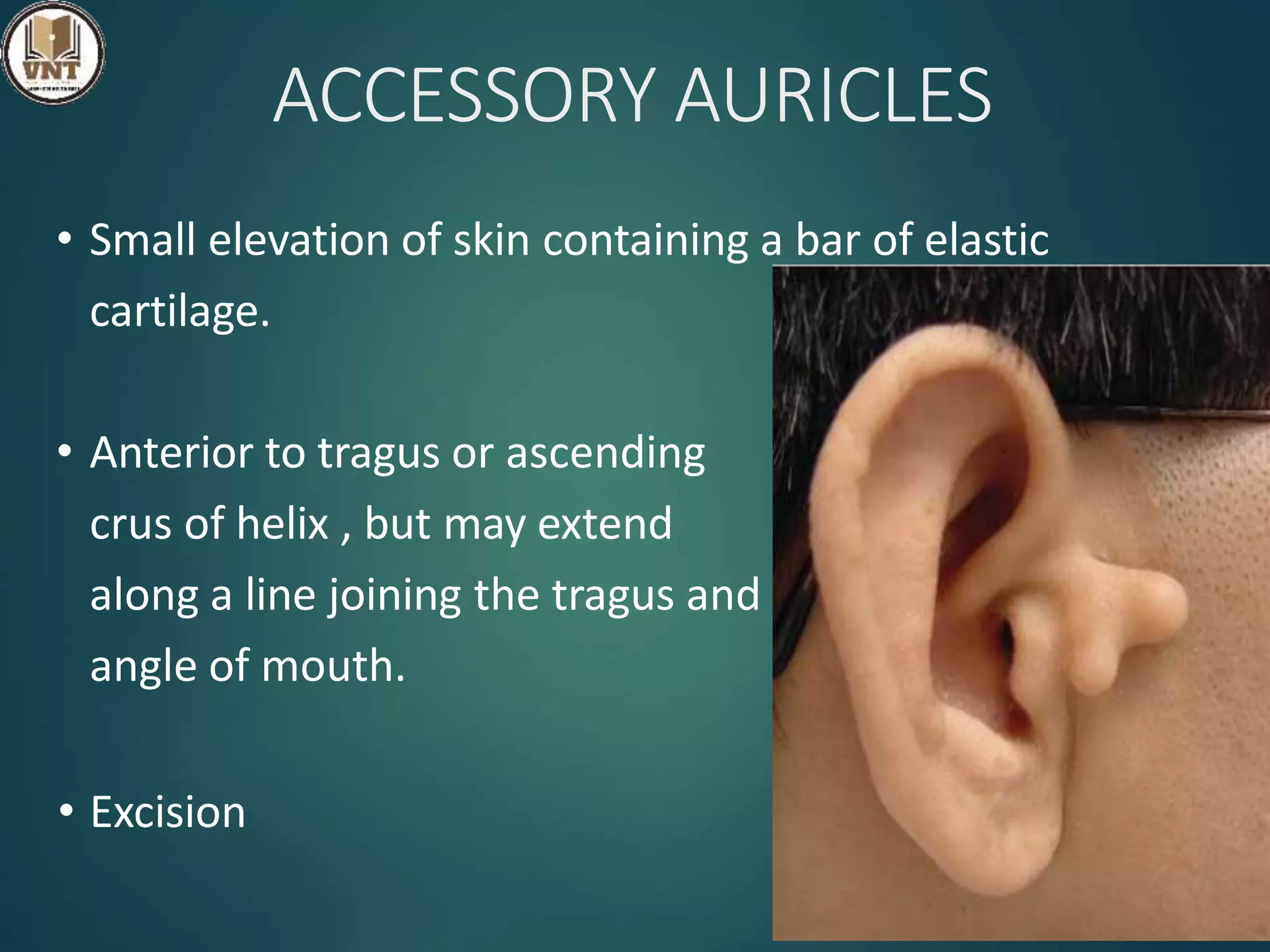
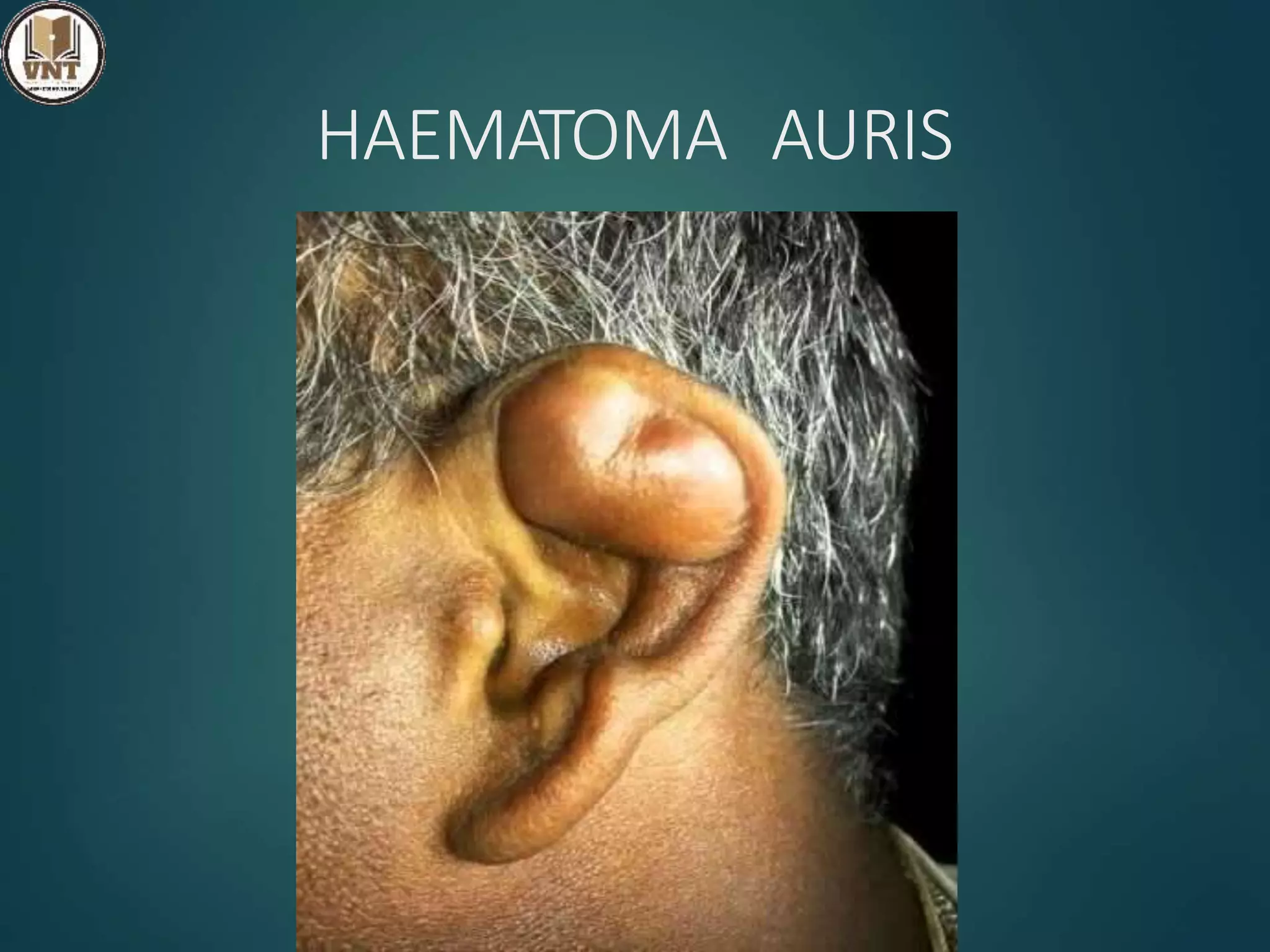
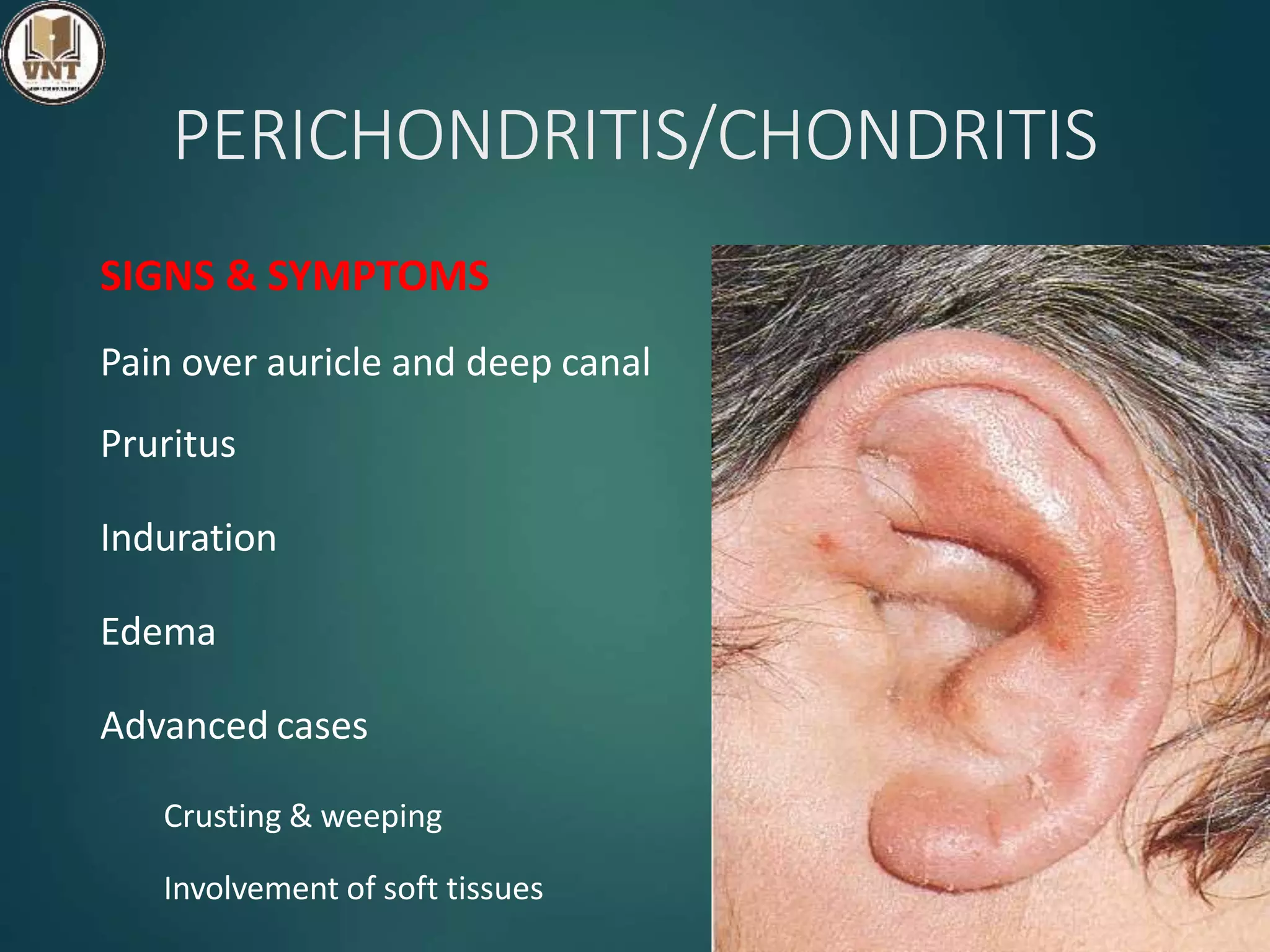
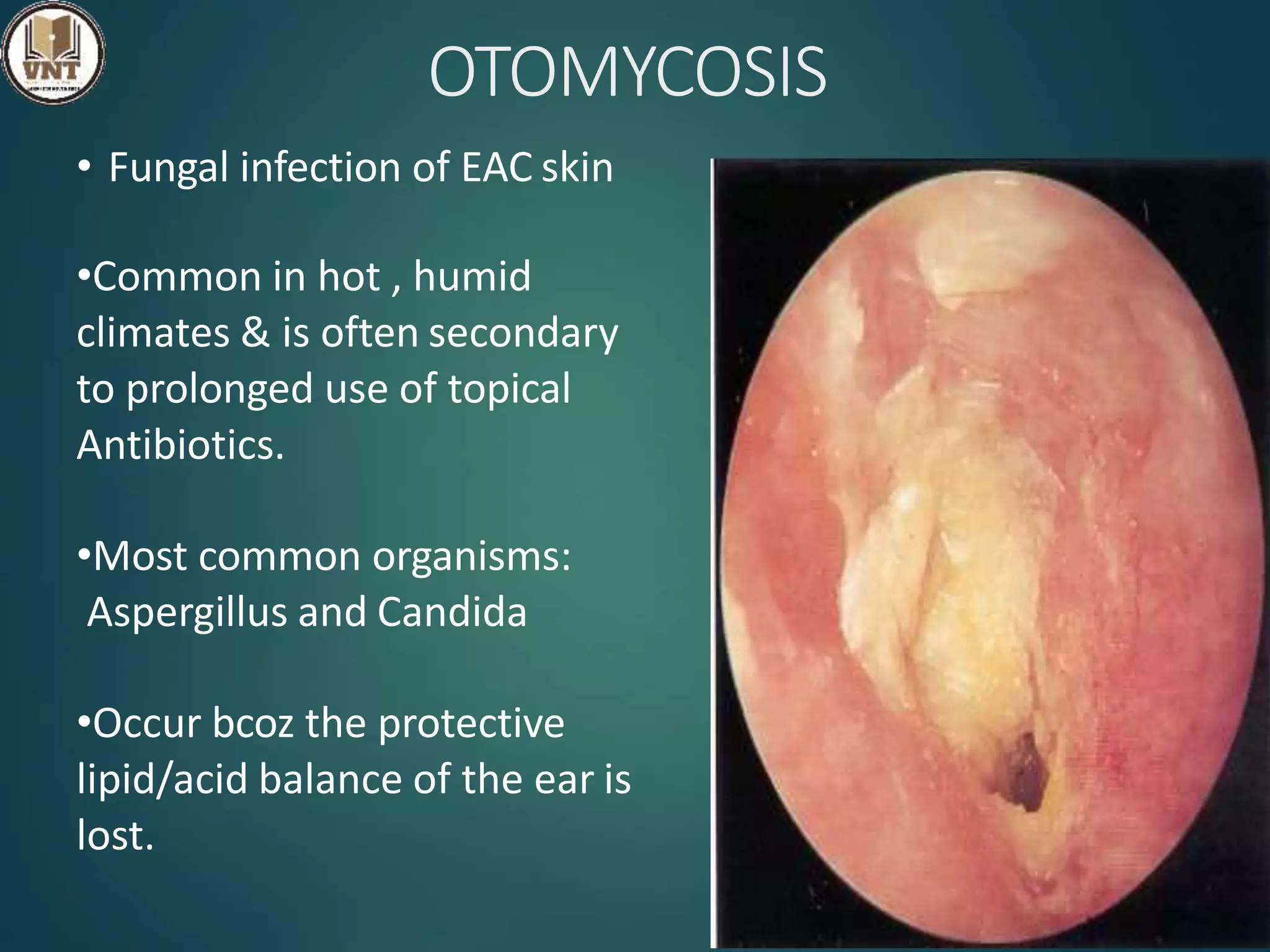
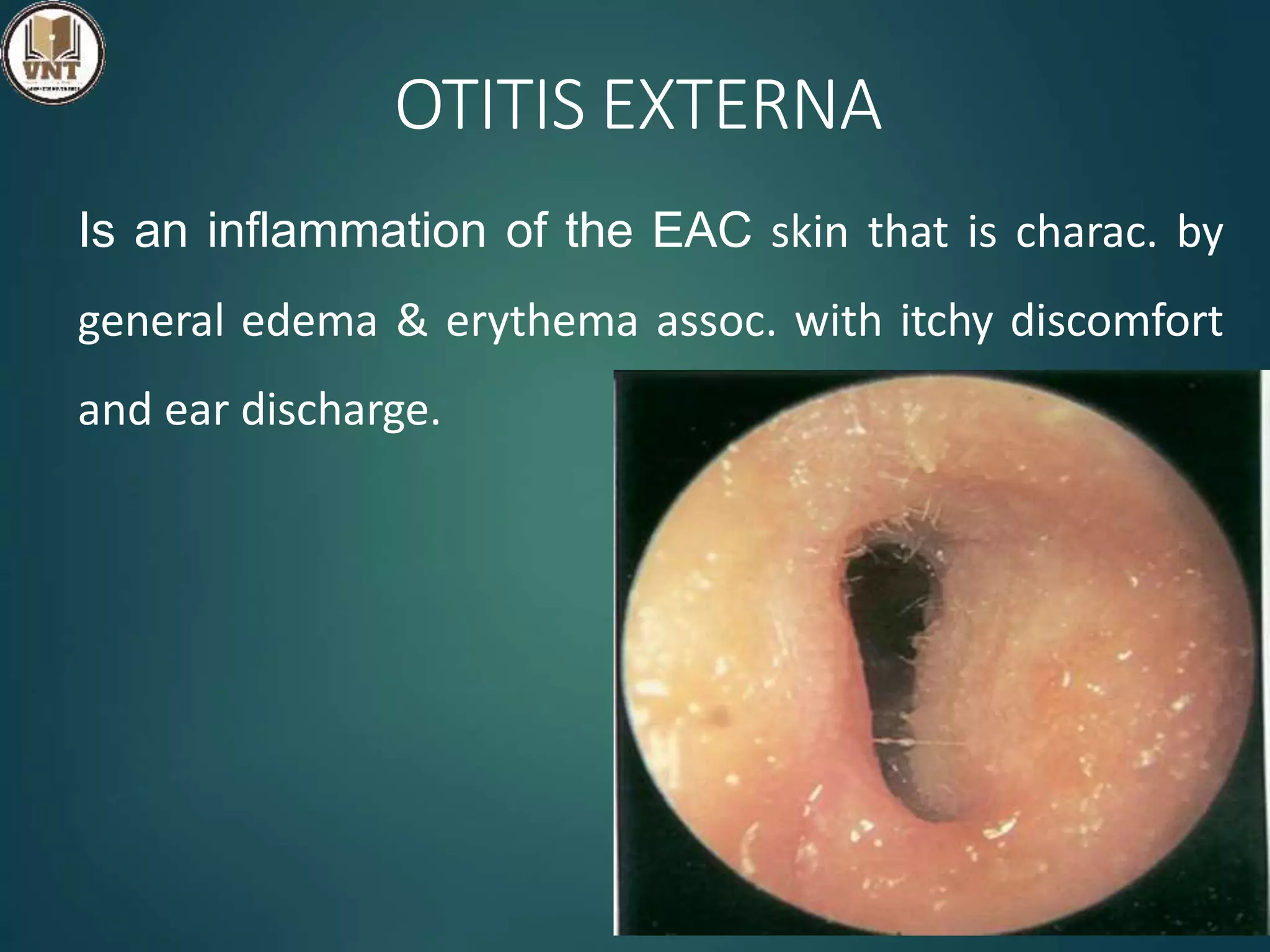
This document discusses deformities and conditions of the external ear, including congenital abnormalities and inflammation. It describes several congenital conditions involving abnormal development of the pinna, such as Darwin's tubercle, Wildermuth's ear, and Mozart's ear. External ear inflammation, including perichondritis, furunculosis, otitis externa, and other conditions are also covered. Signs, symptoms, causes, and treatments are provided for each condition. The aim is to comprehensively review deformities and inflammatory conditions that can affect the external ear.