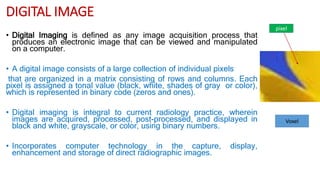
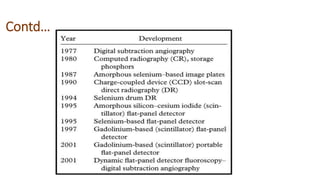
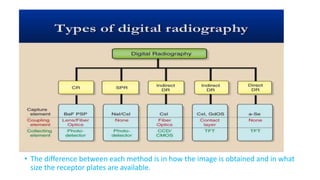
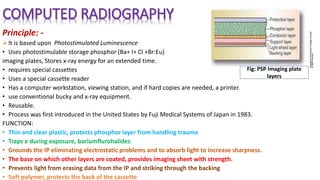
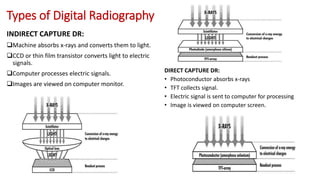
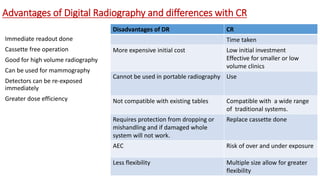
Digital imaging involves capturing radiographic images digitally using various methods like computed radiography (CR), direct radiography (DR), or scan projection radiography (SPR). CR uses photostimulable phosphor plates while DR uses flat panel detectors, eliminating processing. Digital imaging provides advantages like improved image manipulation, reduced radiation exposure, and improved storage and sharing of images. Key types of digital radiography discussed are CR, DR, SPR, digital fluoroscopy, and digital subtraction angiography (DSA).