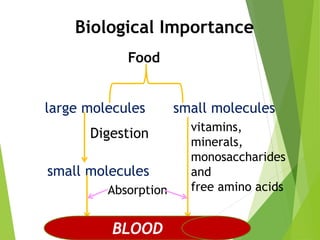
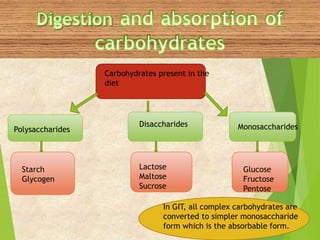
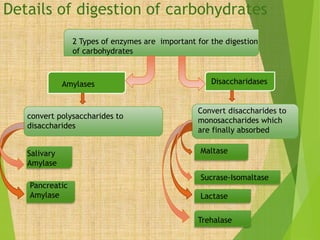
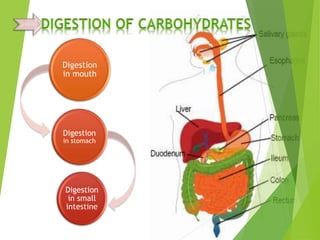
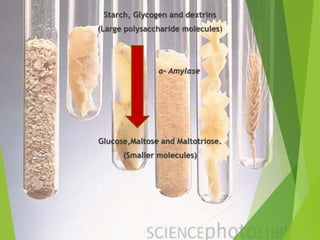
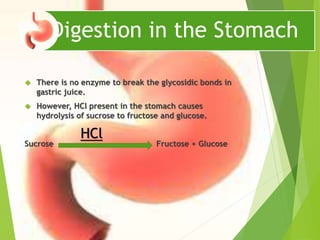
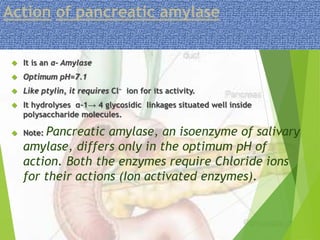
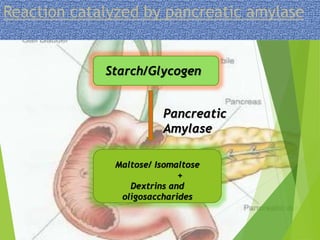
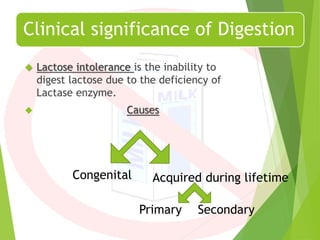
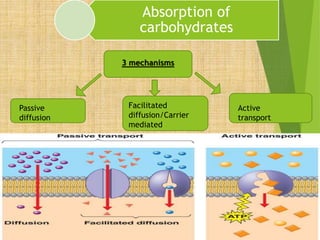
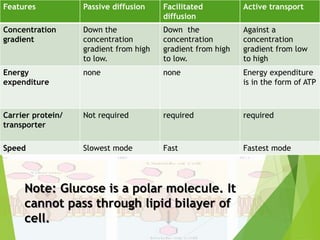
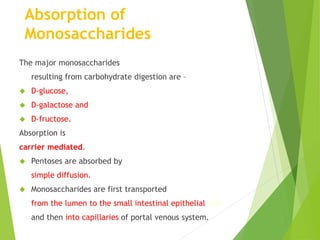
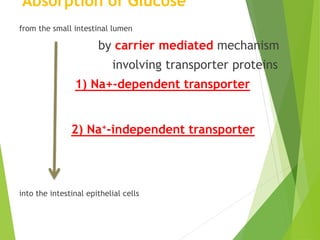
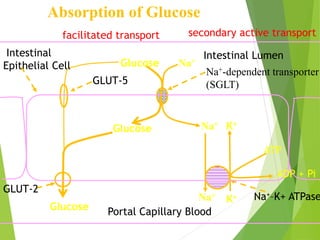
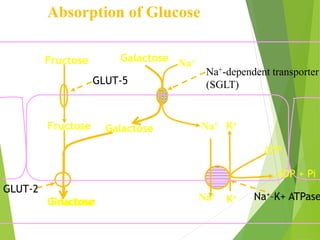
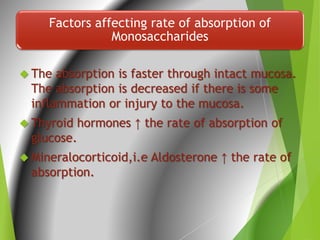
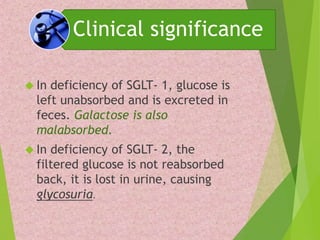
This document summarizes the digestion and absorption of carbohydrates. It begins by outlining the types of carbohydrates present in the diet and how they are broken down by enzymes into simpler monosaccharides. It then details the specific enzymes involved in digesting carbohydrates at each step, from salivary amylase in the mouth to pancreatic amylase and disaccharidases in the small intestine. Absorption of monosaccharides like glucose, galactose and fructose occurs via active transport in the intestinal epithelium. Clinical examples like lactose intolerance are also discussed.