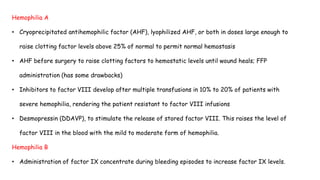
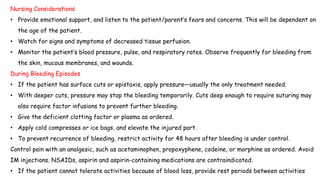
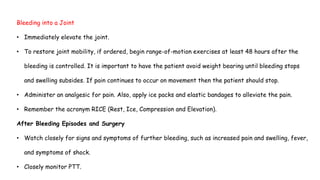
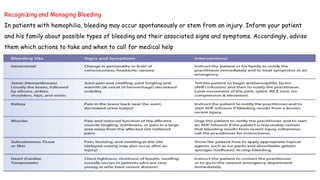
Hemophilia is a hereditary bleeding disorder caused by deficiencies in clotting factors VIII or IX. Hemophilia A accounts for 80% of cases and results from a lack of factor VIII, while Hemophilia B makes up 15% of cases and stems from a deficiency in factor IX. Symptoms include bleeding after injury or surgery, bleeding into joints or muscles, and internal bleeding. Treatment focuses on replacing the deficient clotting factor through infusions to control bleeding and allow for proper healing. Nursing care involves monitoring for signs of bleeding, providing pain management and joint care, educating on injury prevention, and ensuring proper treatment is administered.