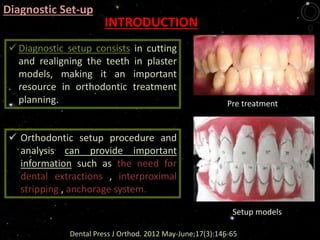
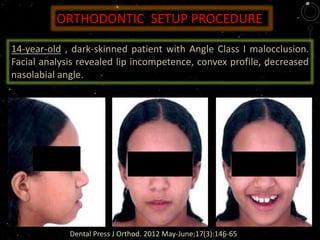
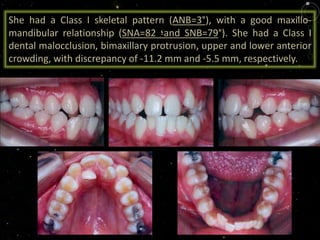
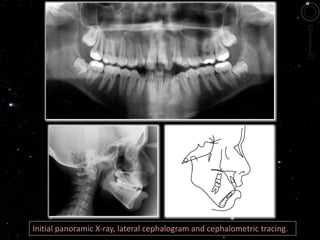
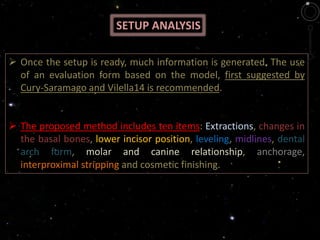
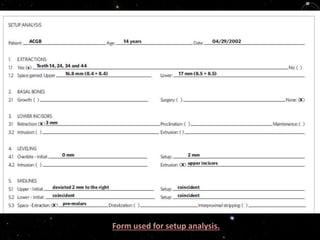
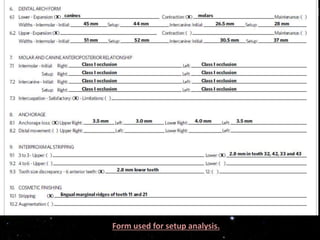
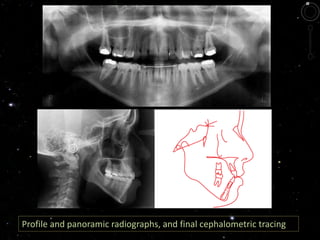
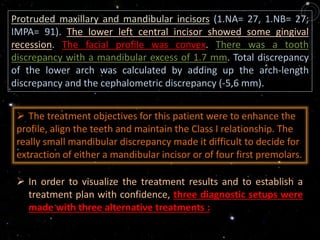
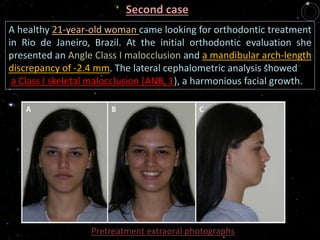
This document describes the steps for performing an orthodontic diagnostic setup using plaster study models. It involves:
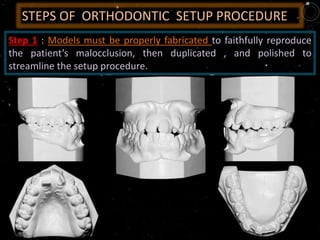
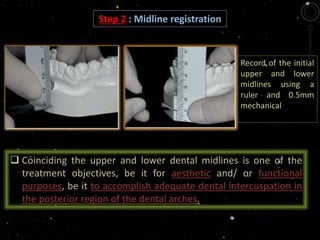
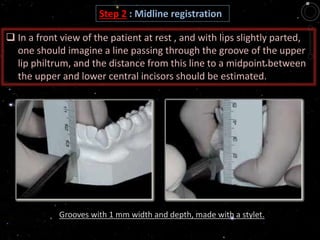
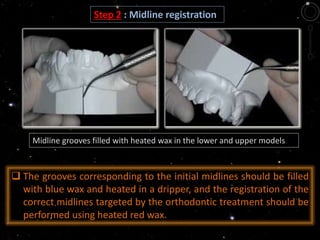
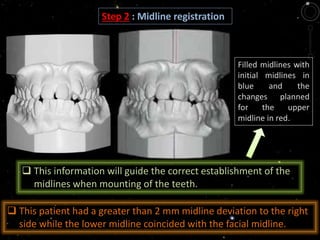
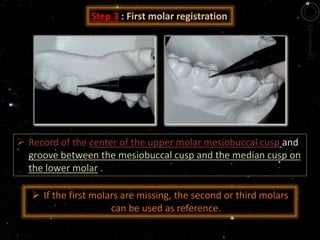
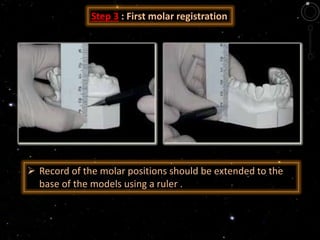
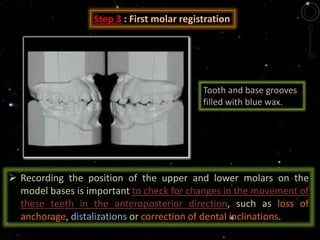
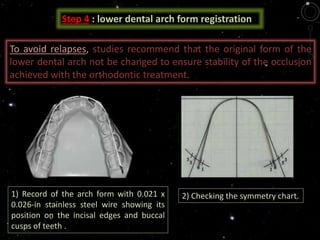
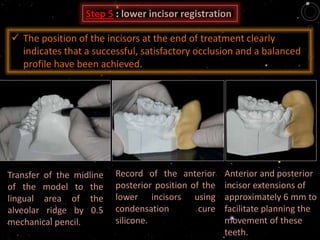
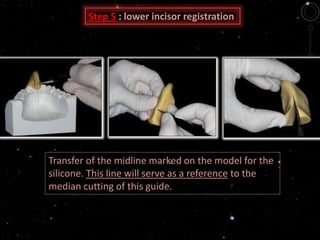
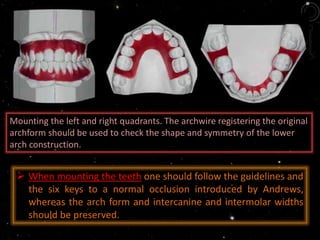
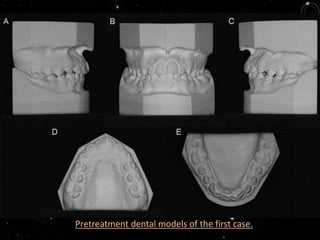
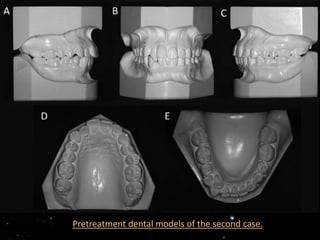
1) Registering the midline, first molar positions, and lower arch form on the initial study models.
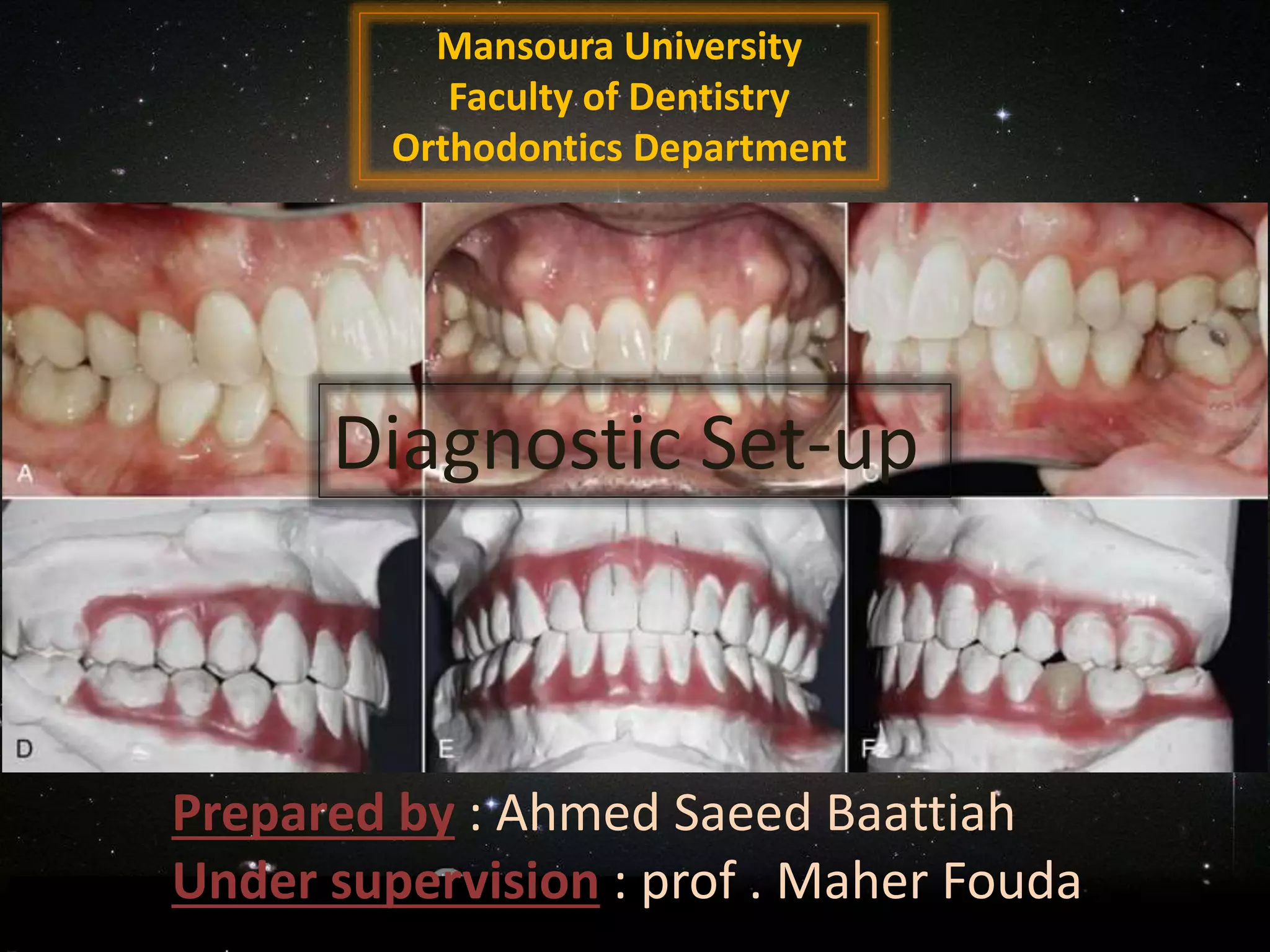
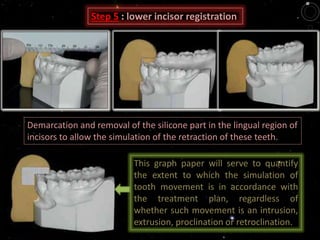
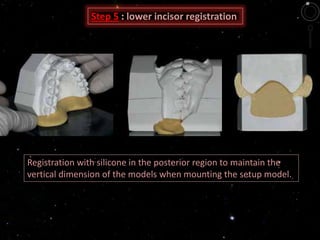
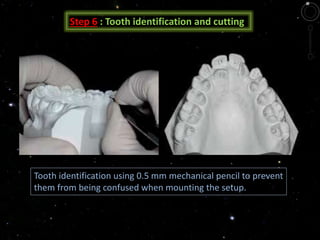
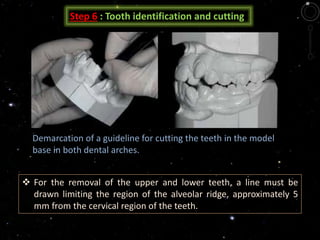
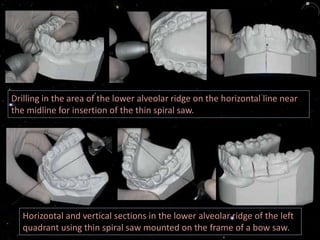
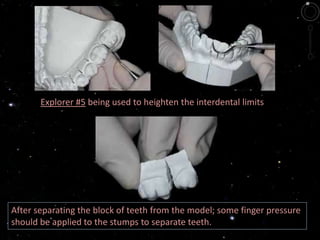
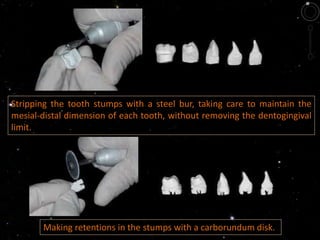
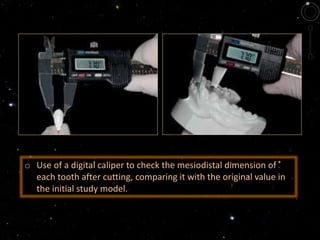
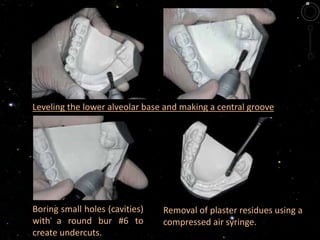
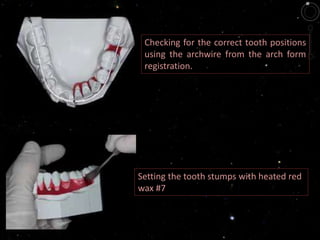
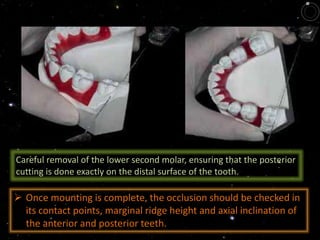
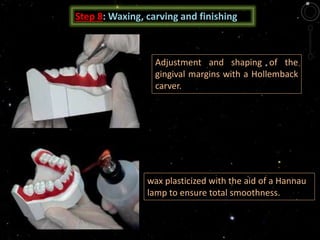
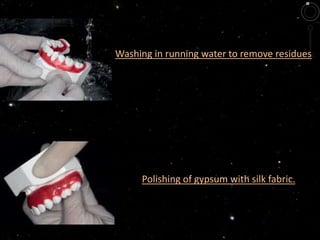
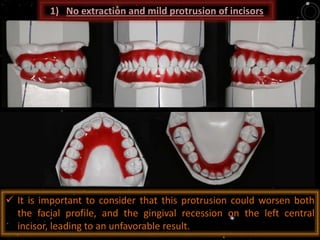
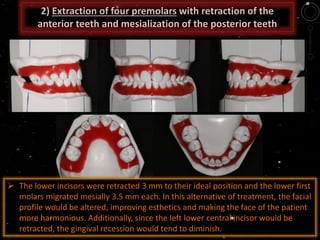
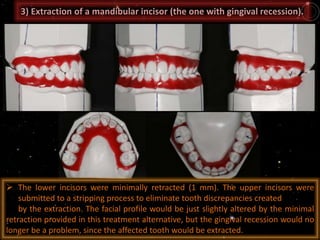
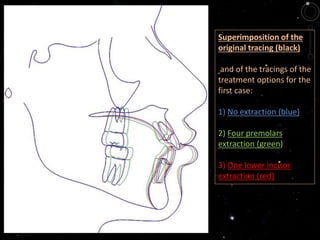
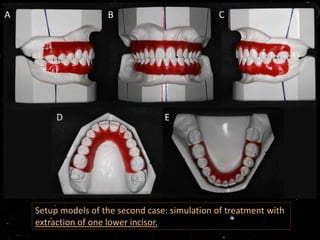
2) Cutting and repositioning the teeth on the setup models to simulate the proposed orthodontic treatment plan.
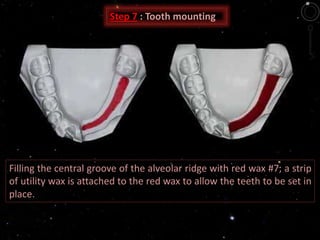
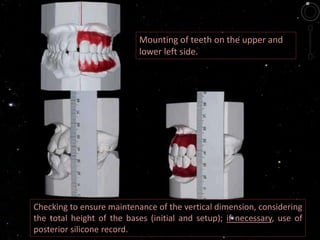
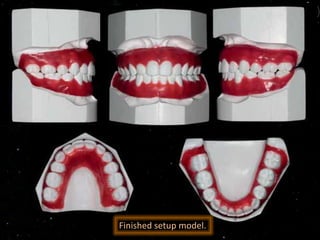
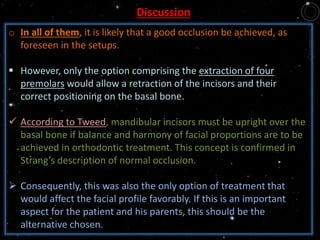
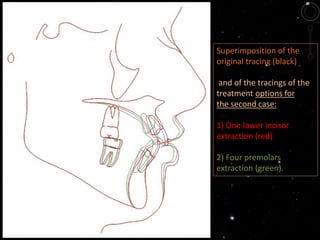
3) Mounting the teeth in the new positions and analyzing the occlusion and treatment objectives that can be achieved.
Diagnostic setups provide important information to assess treatment options and plan anchorage needs before starting orthodontic treatment. They allow simulation and verification of the proposed treatment results.