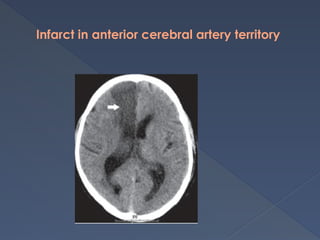
The document provides an extensive overview of cerebrovascular disorders and Parkinson's disease, covering assessment, classification, risk factors, and management strategies. It details clinical features of strokes, including ischemic and hemorrhagic types, and outlines diagnostic investigations like CT and MRI scans. Furthermore, it discusses Parkinson's disease, its symptoms, staging, and treatment options, including pharmacological and surgical approaches.