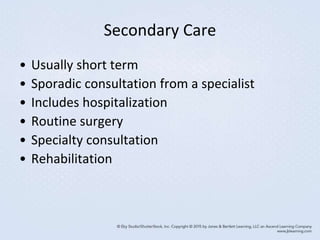
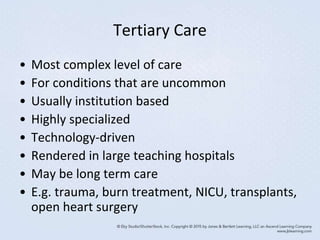
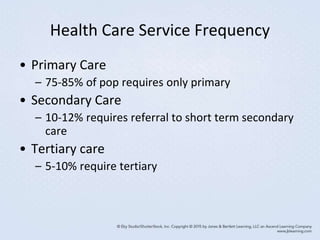
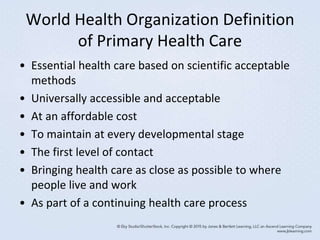
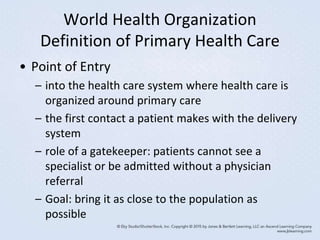
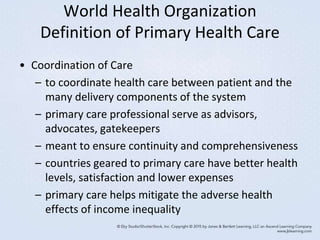
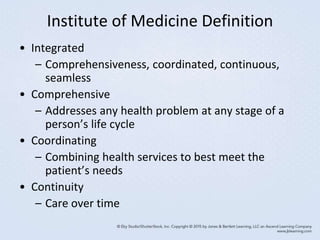
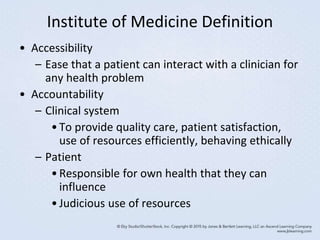
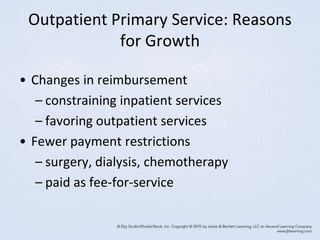
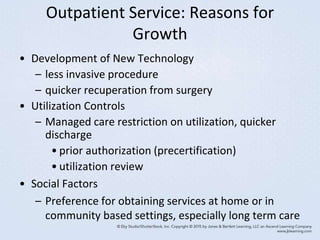
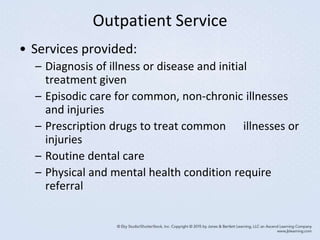
This document discusses outpatient and primary care services. It defines key terms like outpatient, ambulatory care, and primary care. It describes the growth of outpatient services due to changes in reimbursement and technology. Various outpatient settings are covered, including private practices, hospital-based clinics, free-standing facilities, home health, and hospice. The roles of primary, secondary, and tertiary care are also outlined.