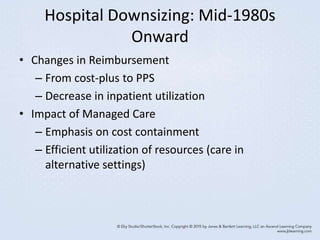
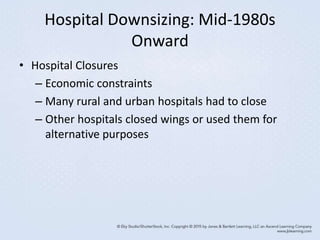
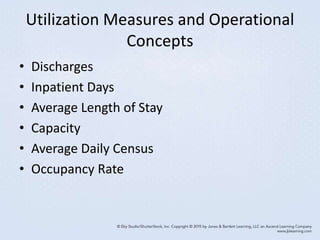
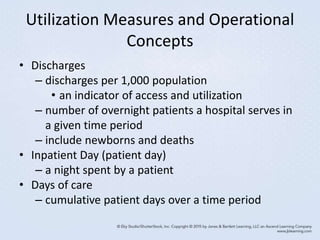
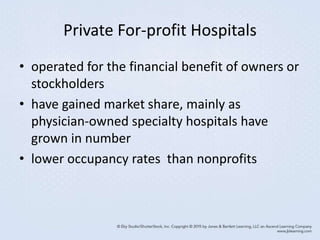
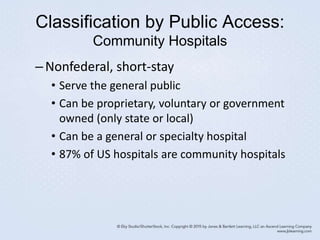
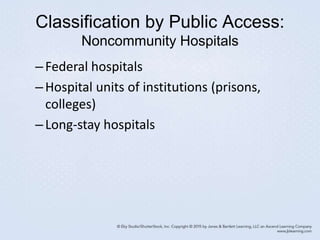
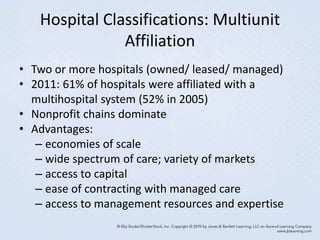
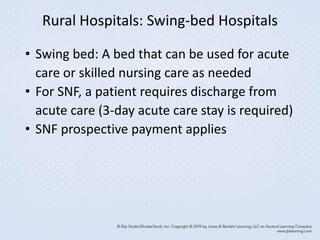
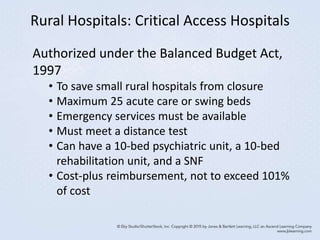
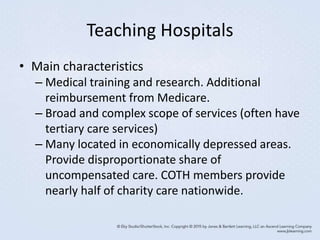
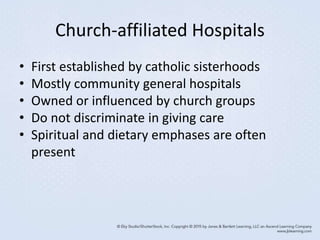
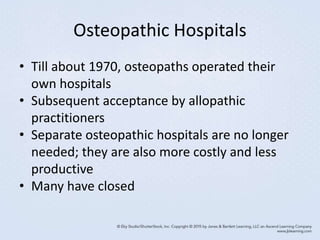
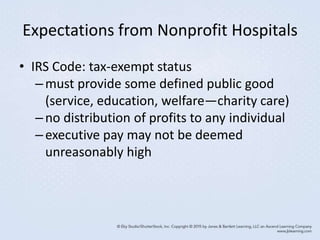
This document discusses inpatient facilities and services, including the evolution and transformation of hospitals in the United States. It covers the factors that contributed to the growth of hospitals prior to the 1980s, as well as the subsequent decline in hospitals and utilization. It also differentiates between various types of hospitals, including classifications by ownership, public access, services provided, and multi-unit affiliation. Key concepts around hospital utilization measures, costs, governance and regulations are also introduced.