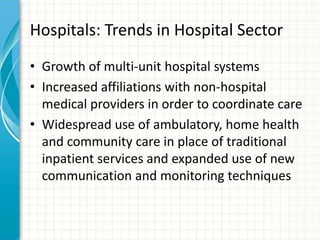
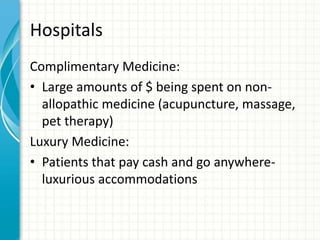
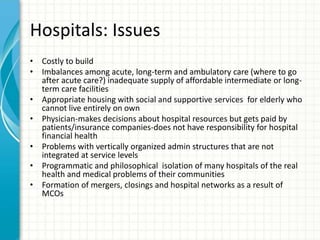
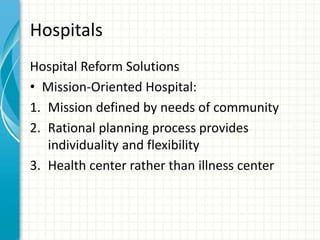
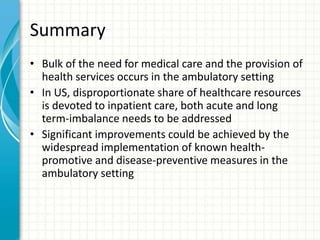
This document provides an overview of hospitals and the healthcare delivery system. It discusses the evolution of hospitals from places where people went to die to modern multiservice institutions. Hospitals are classified by type, ownership, size and services provided. Trends include consolidation, outpatient care replacing inpatient care, and increased partnerships between hospitals and other providers. Challenges include rising costs, physician decision making, and ensuring access to care.