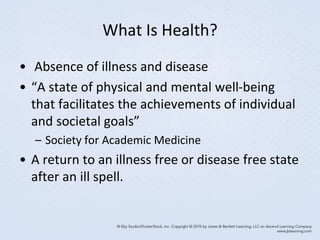
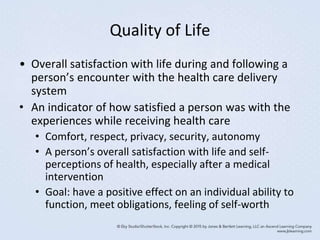
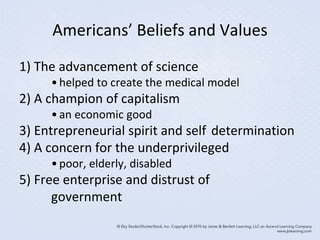
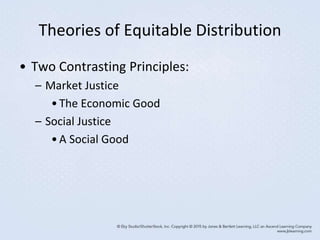
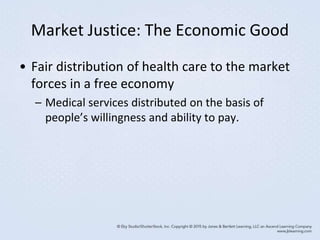
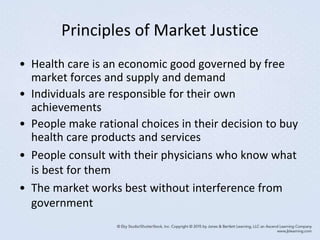
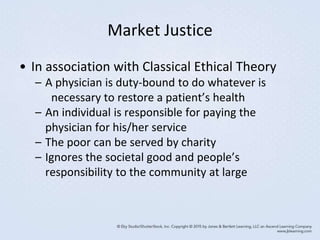
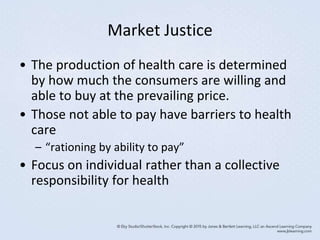
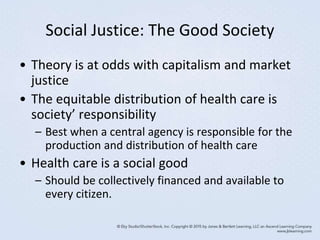
1) The document discusses American beliefs and values related to health, including viewing health care as an economic good subject to market forces rather than a publicly financed system.
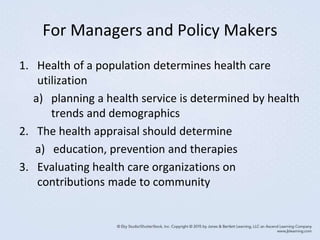
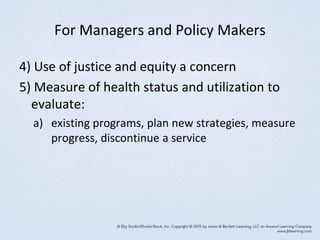
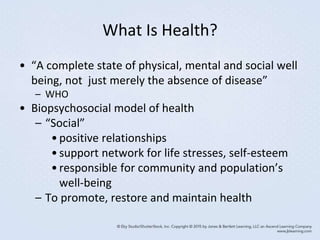
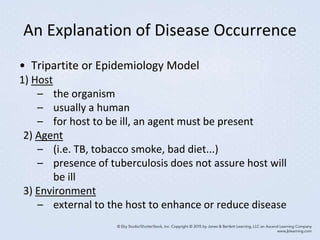
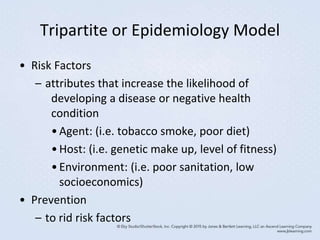
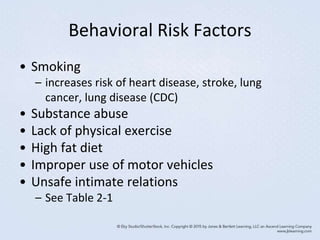
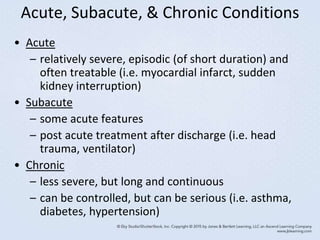
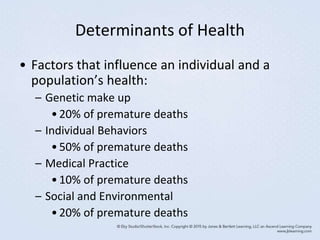
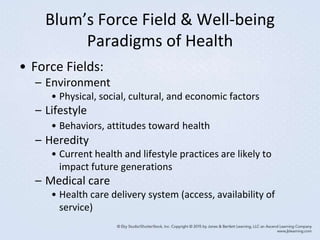
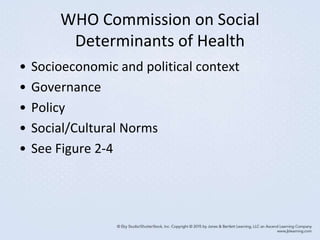
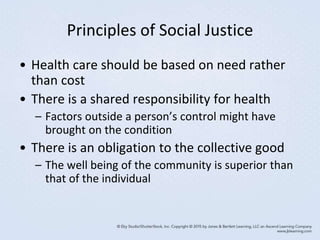
2) Key determinants of health are discussed, including behaviors, environment, medical care, and social factors. Health is influenced by multiple levels from genetic to societal.
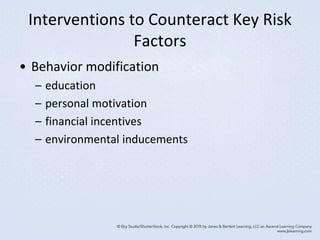
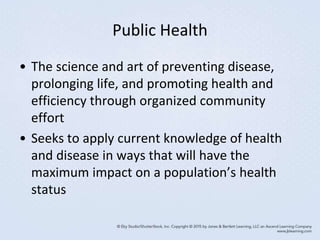
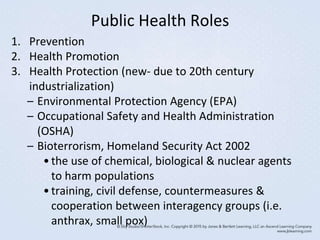
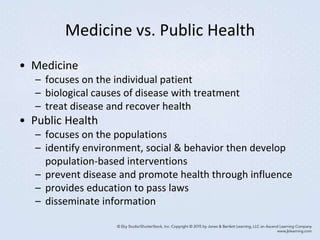
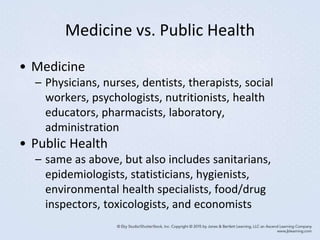
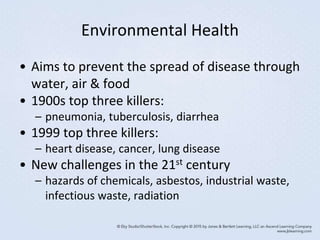
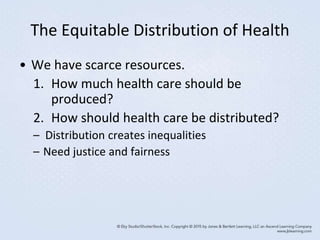
3) Public health aims to promote community health through disease prevention, health education, and policies addressing environmental and societal risks to health. It complements medicine's focus on treatment of individuals.