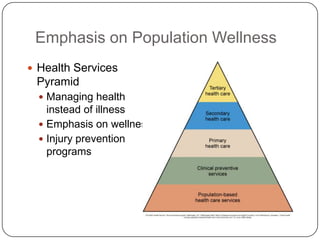
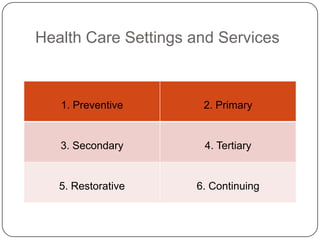
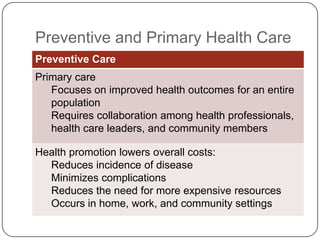
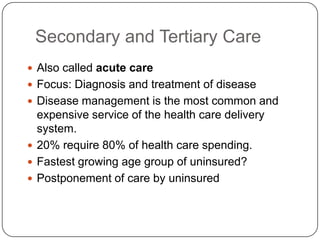
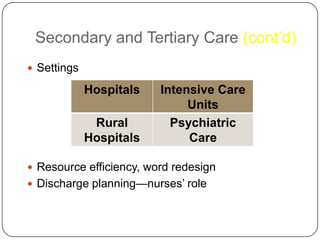
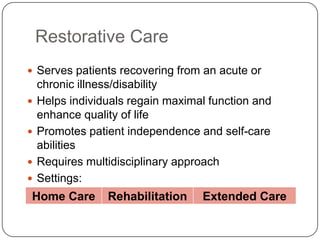
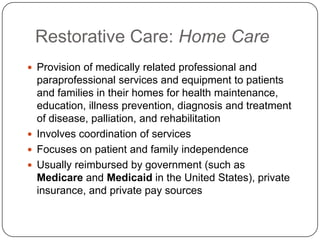
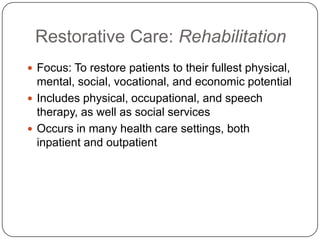
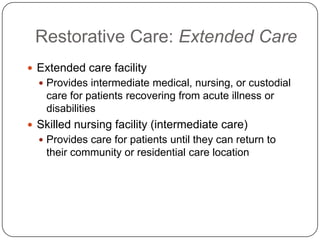
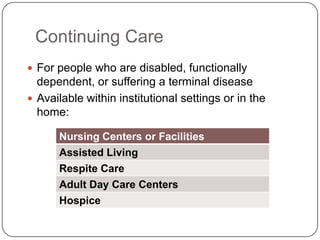
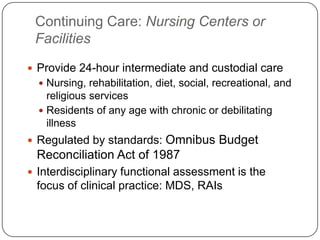
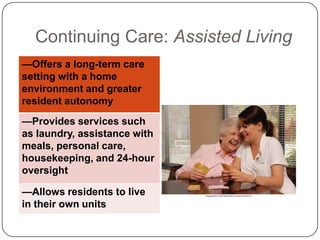
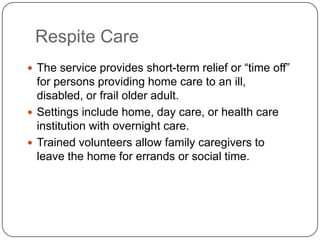
This document provides an overview of the US health care delivery system. It discusses challenges like reducing costs while maintaining quality, improving access, and encouraging healthy behaviors. It also covers different levels of care like preventative, primary, secondary, tertiary, restorative, continuing care and settings within each level. Issues discussed include the nursing shortage, evidence-based practice, quality/safety, and the future of health care needing to address the uninsured while improving quality through nurse participation.