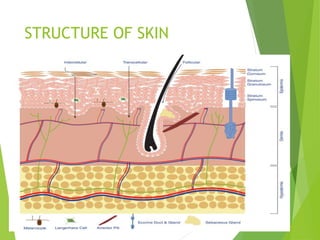
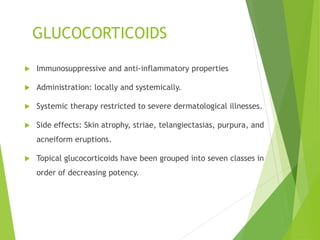
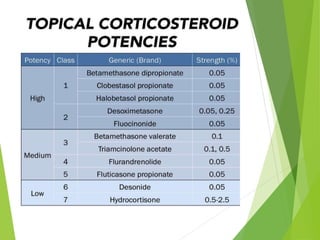
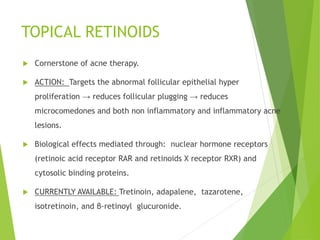
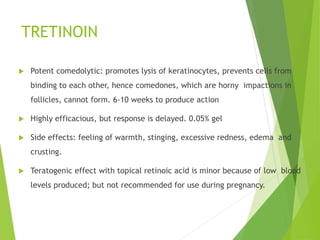
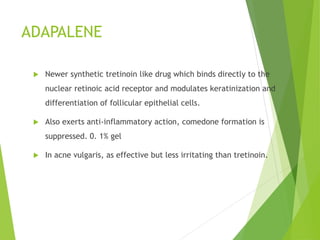
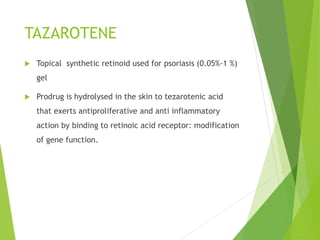
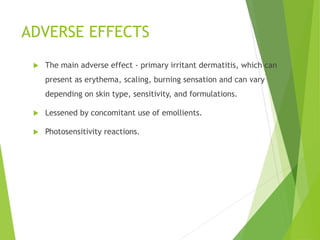
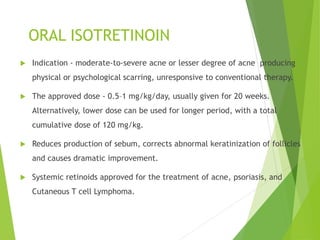
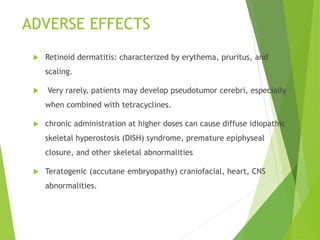
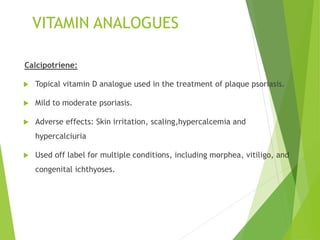
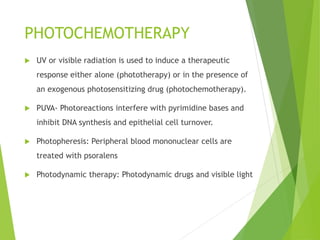
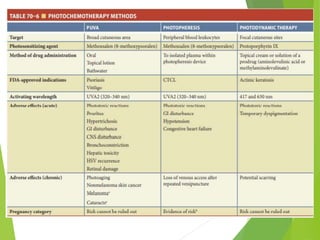
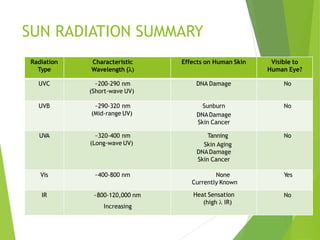
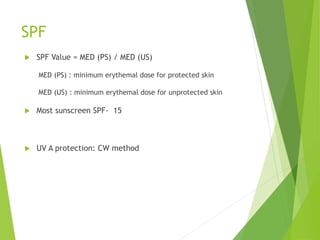
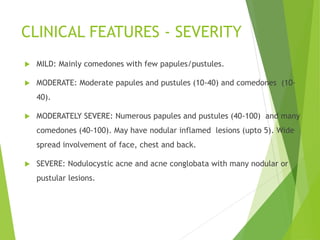
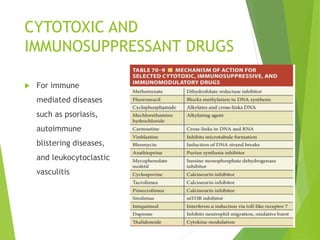
This document summarizes dermatological pharmacology. It discusses the structure of skin and topical vehicles like creams, lotions, gels and ointments used to deliver drugs to the skin. It also discusses various drug classes used in dermatology like glucocorticoids, retinoids, antibiotics, antifungals and immunomodulators. Specific drugs covered include tretinoin, adapalene, isotretinoin, calcipotriene and phototherapy agents. It also provides information on treatment of conditions like acne, hyperpigmentation and photoprotection with sunscreens.