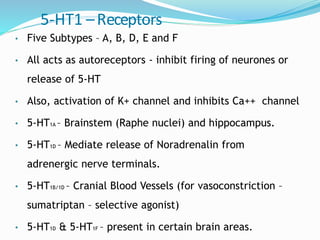
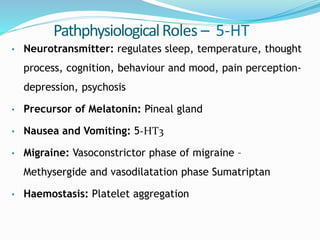
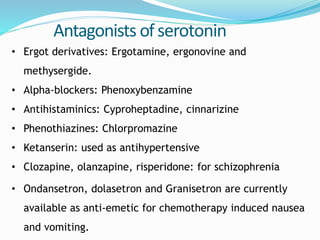
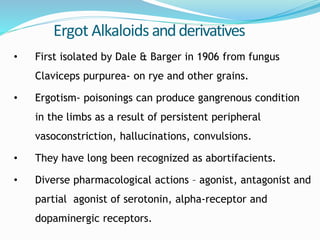
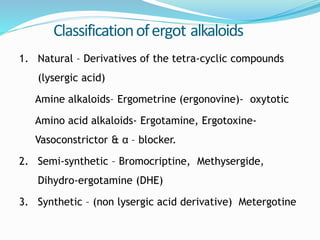
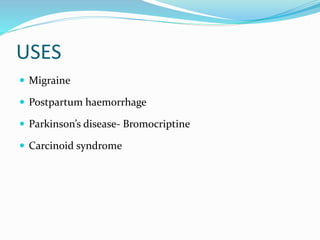
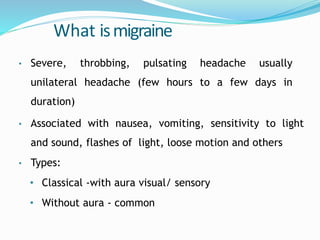
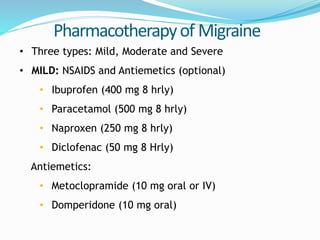
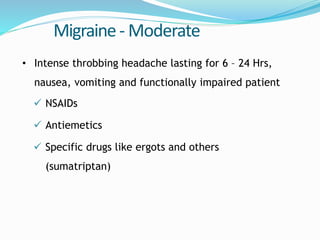
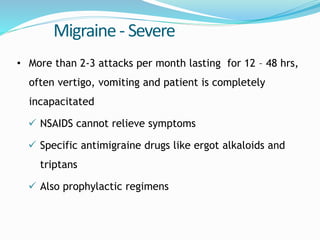
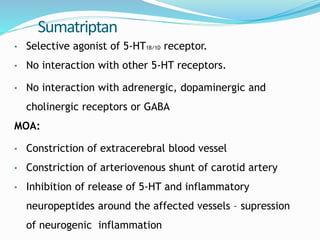
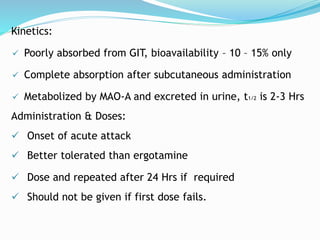
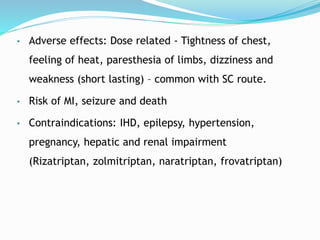
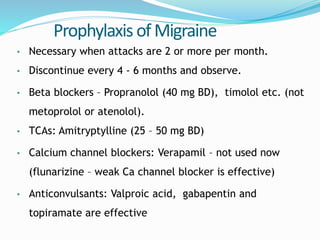
The patient is presenting with symptoms consistent with migraine including severe unilateral headache, nausea, and flashing lights. The probable diagnosis is migraine. For acute treatment, medications like NSAIDs, triptans like sumatriptan, and ergot alkaloids like ergotamine may be used. Prophylactic treatments include beta blockers, TCAs, calcium channel blockers, and anticonvulsants.