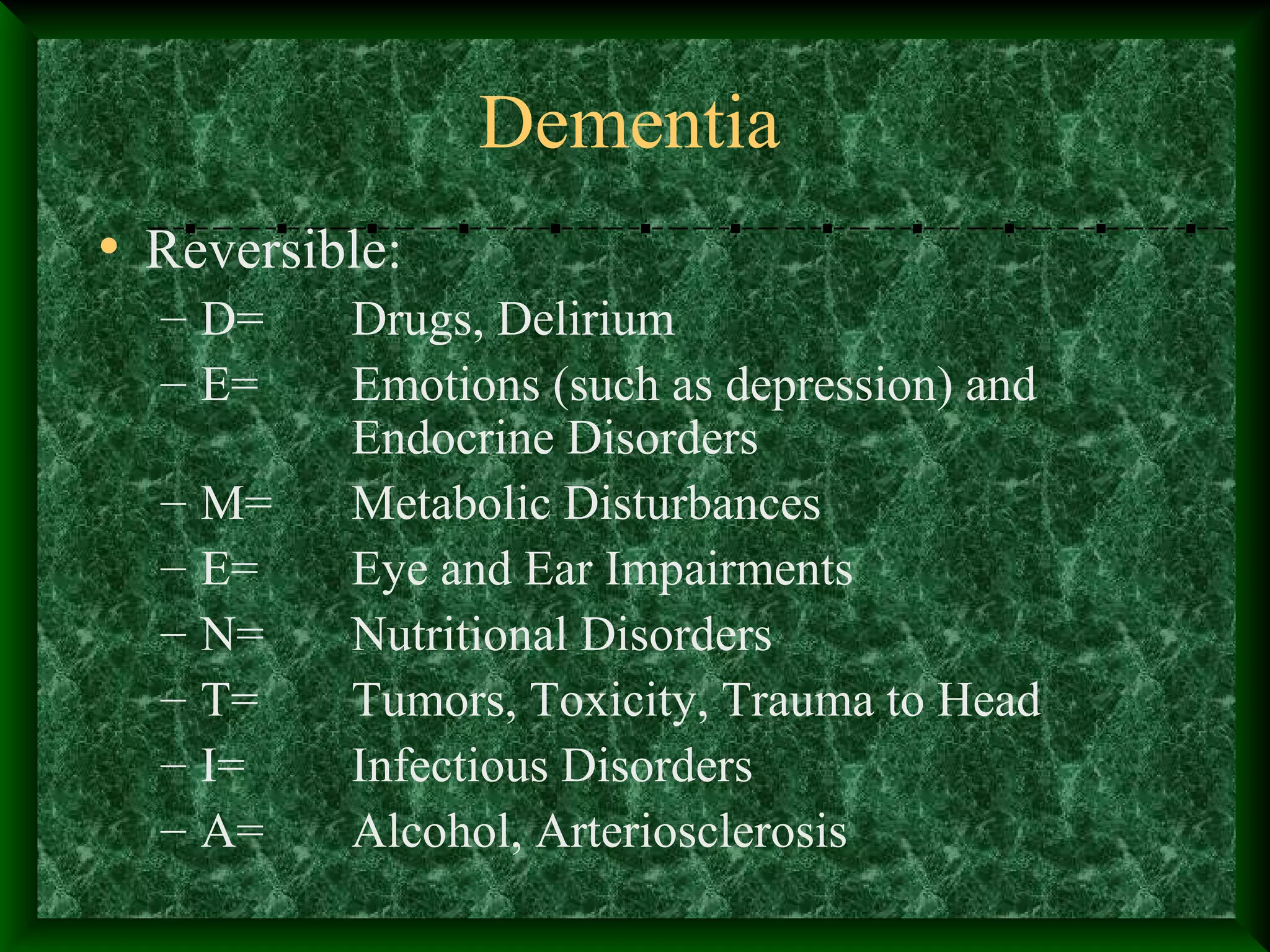
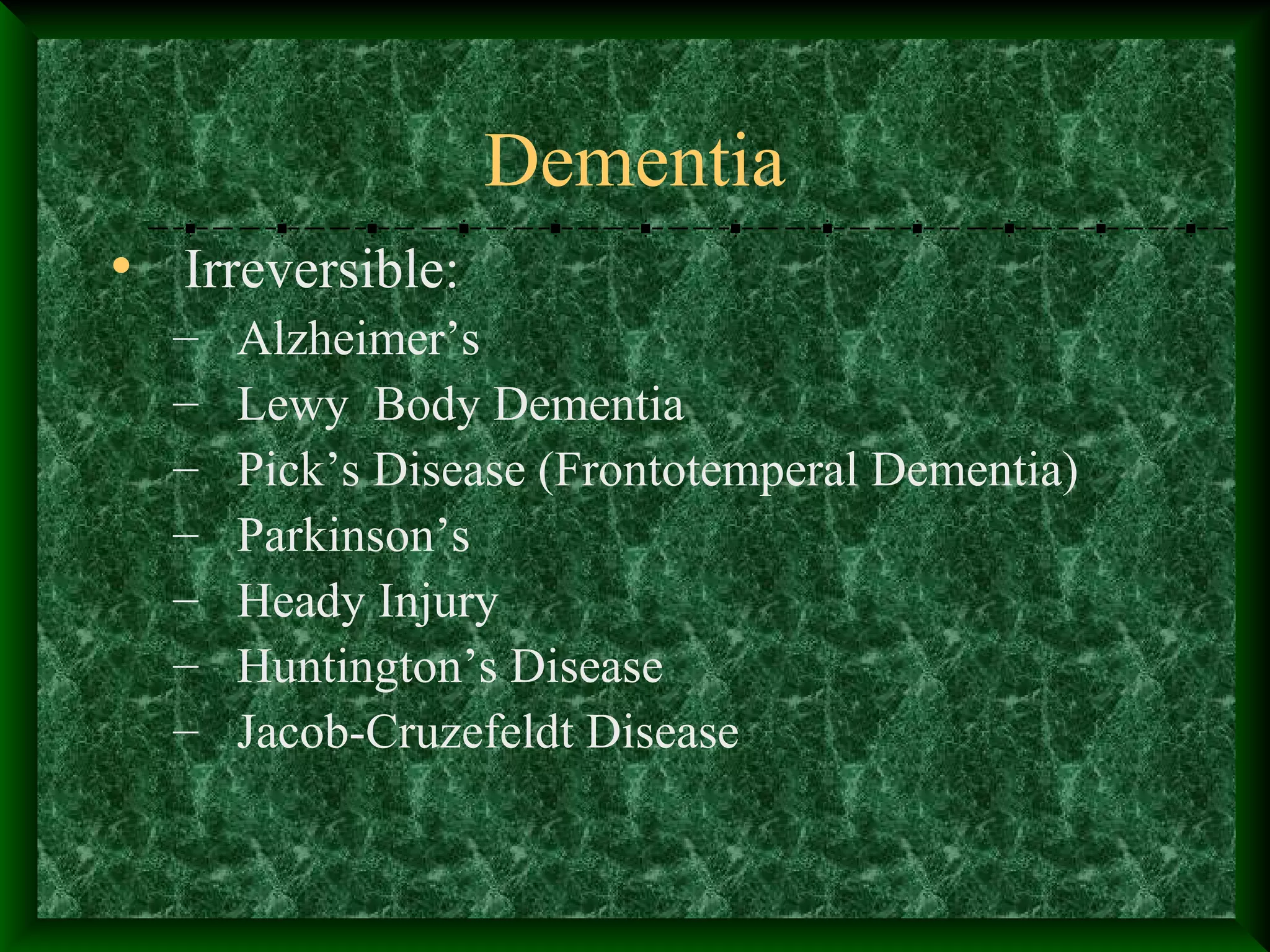
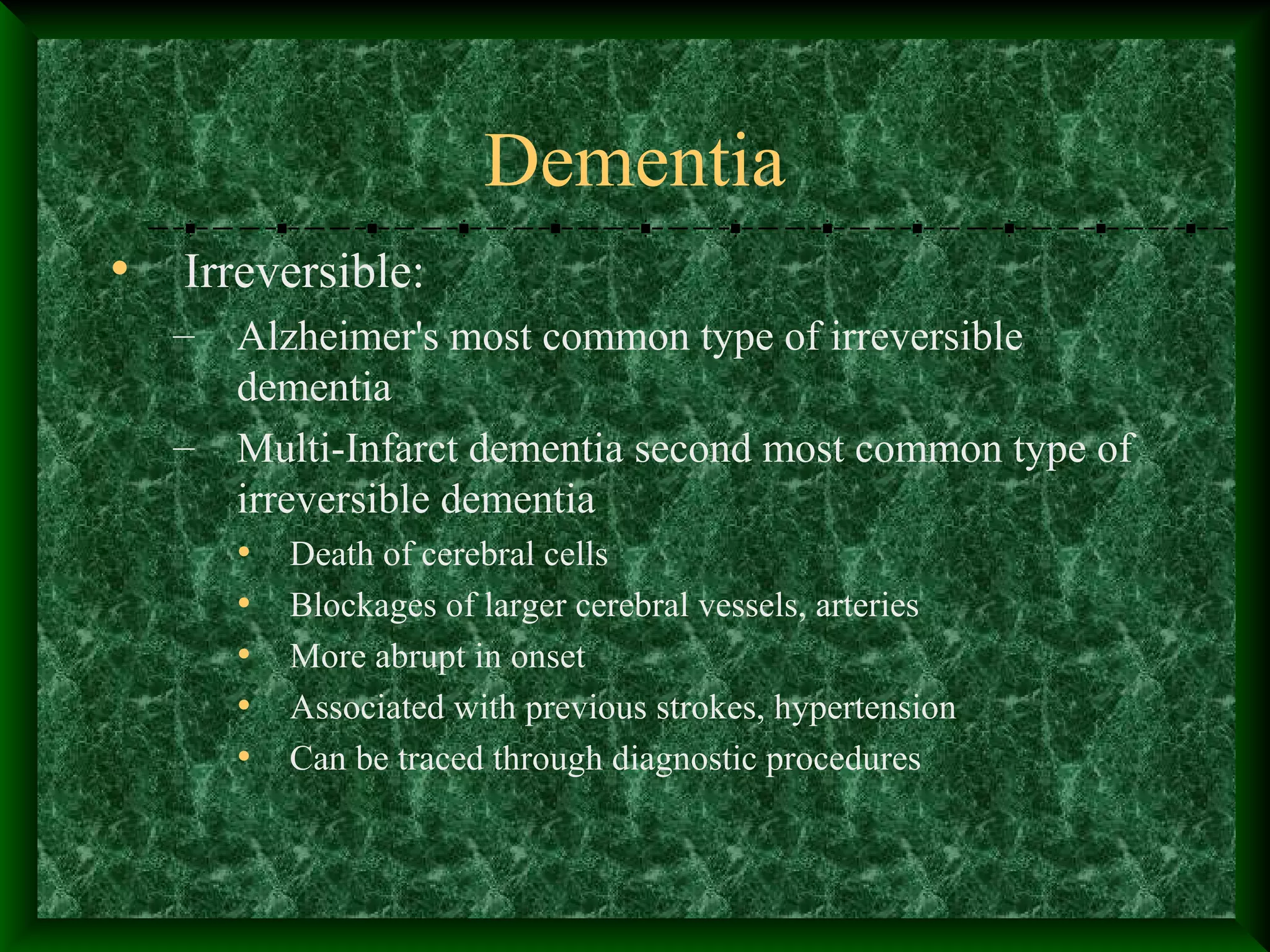
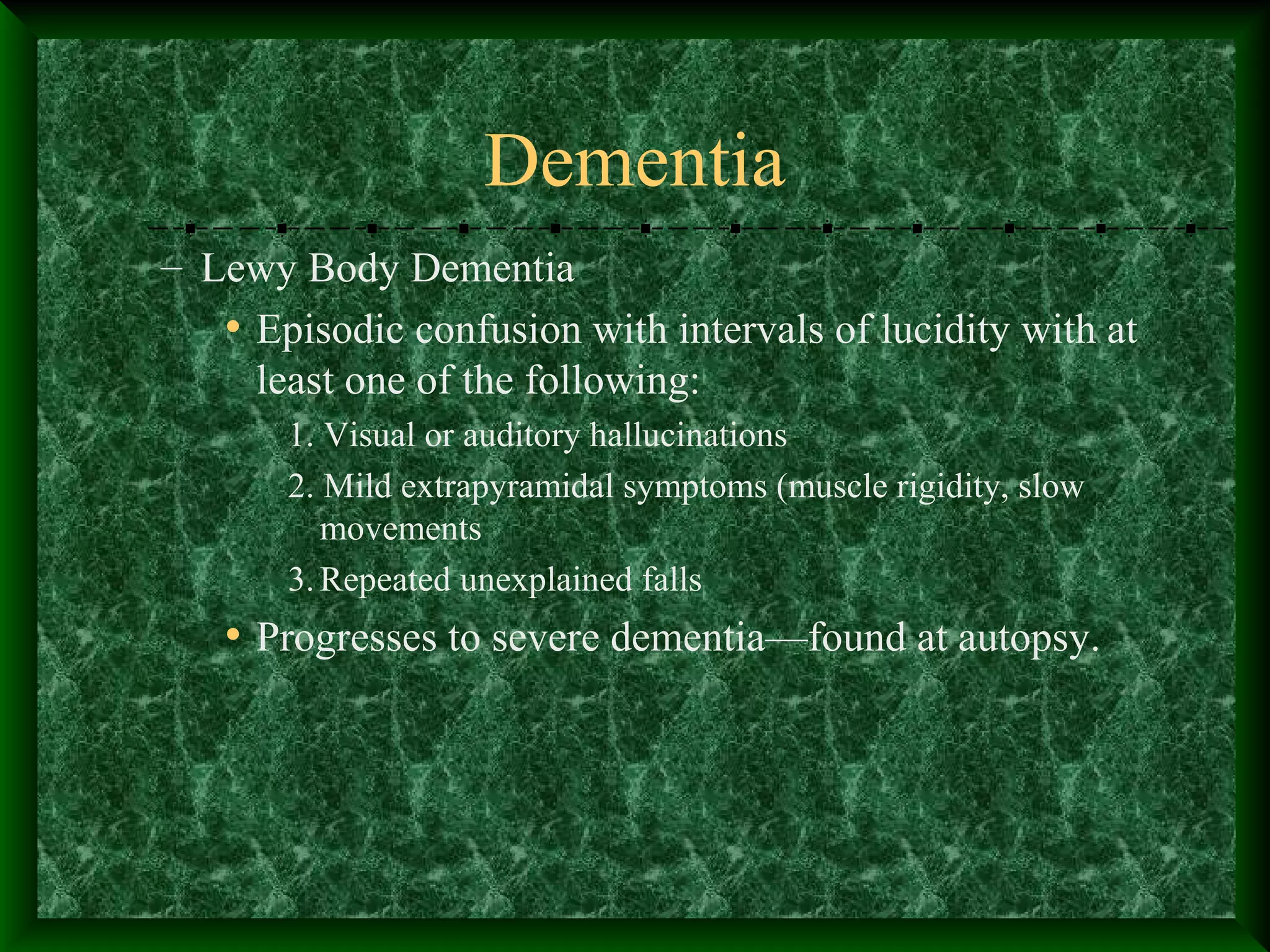
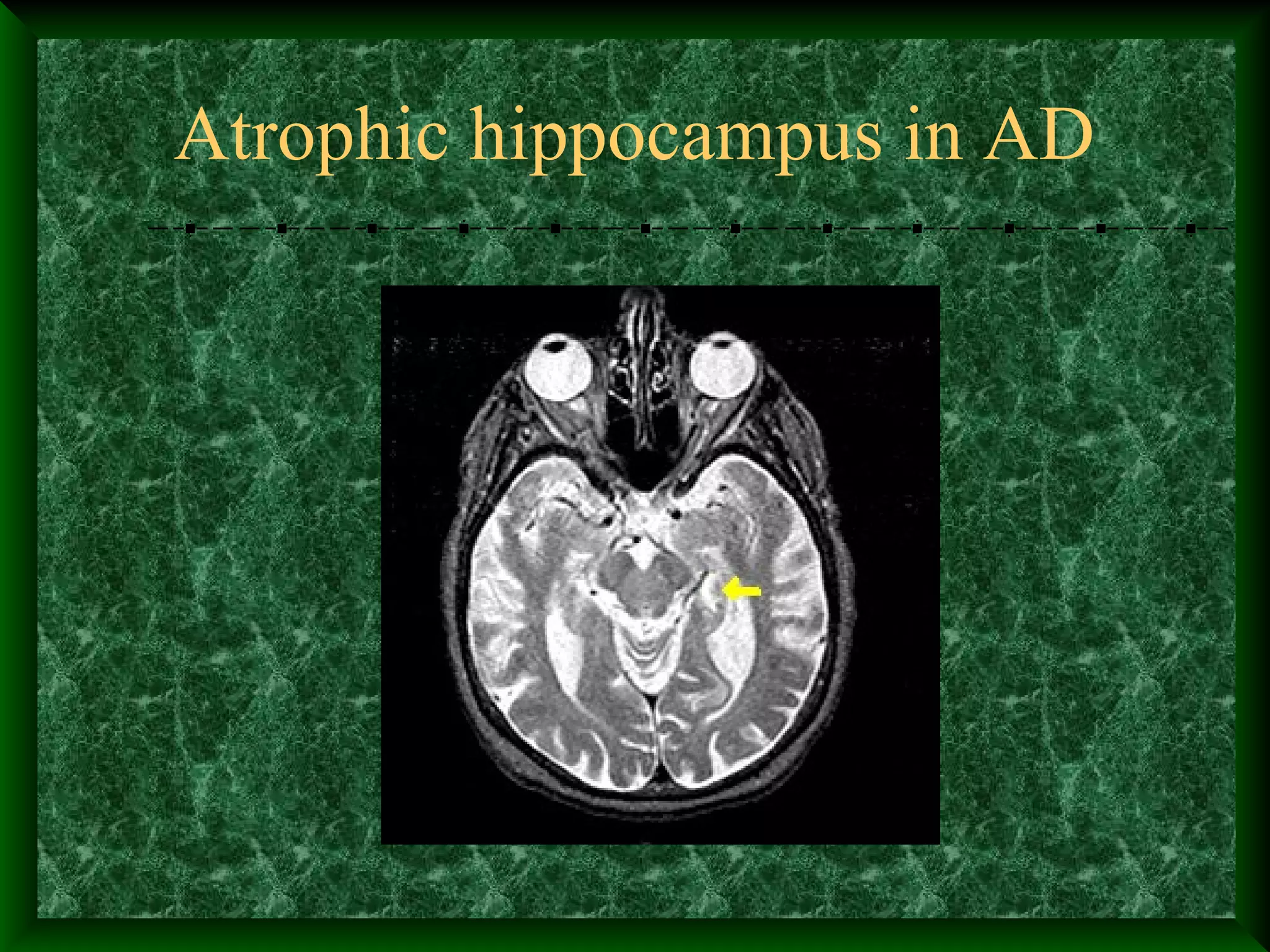
Dementia is a progressive decline in cognitive function that interferes with daily life. It has many potential causes but the most common is Alzheimer's disease. Dementia is characterized by declines in memory, spatial awareness, task performance, language, abstract thinking and mathematical skills. It can be reversible or irreversible. Delirium is a temporary disturbance in consciousness and cognition that develops over a short period of time, often due to an underlying medical condition. Complications of dementia include delusions, hallucinations, depression, aggression, dangerous behaviors and sundowning. Treatment focuses on managing symptoms, ensuring safety, and supporting patients and their caregivers.