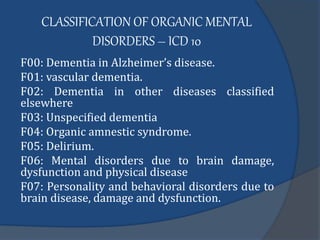
1. Organic mental disorders are caused by physical damage or disease in the brain that results in impaired mental functioning. Common causes include head injuries, strokes, substance abuse, and neurological conditions.
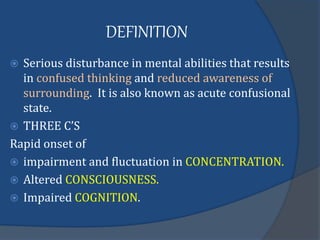
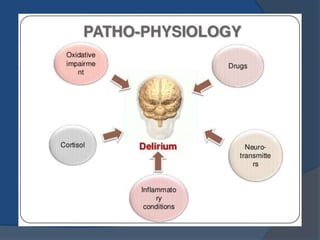
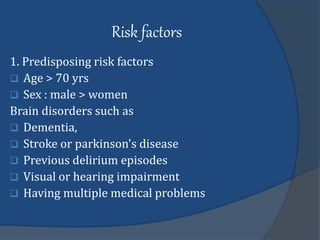
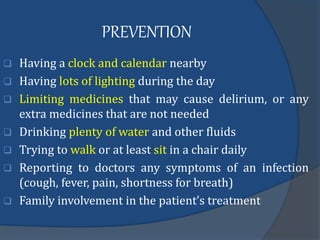
2. Delirium is a type of acute organic mental disorder characterized by a rapid decline in attention, awareness, and cognition. It is often precipitated by medical illnesses, infections, medication side effects, or physical restraints in vulnerable populations like the elderly.
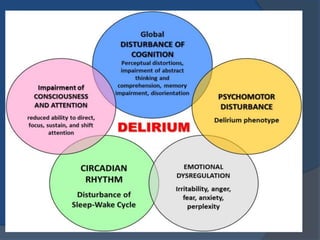
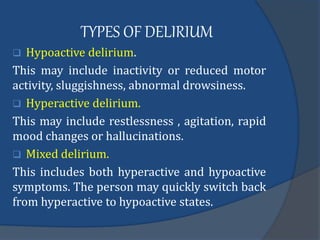
3. Symptoms of delirium include impaired concentration, altered consciousness, cognitive changes, as well as behavioral disturbances like restlessness, hallucinations, or withdrawal. Diagnosis involves assessing mental status, physical examination, and testing to identify underlying medical causes.