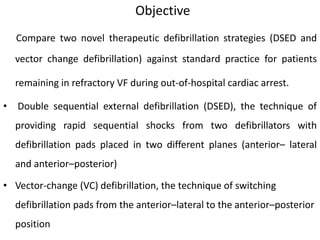
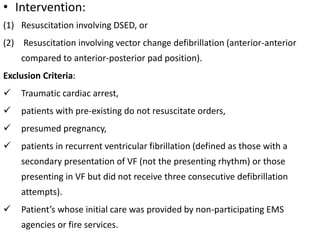
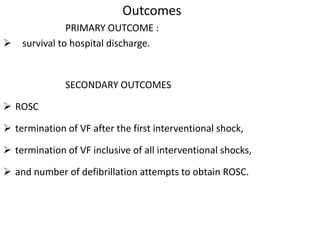
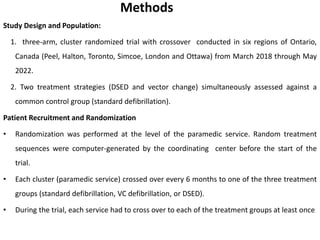
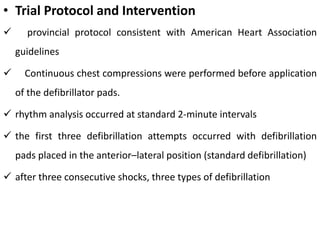
This document summarizes a clinical trial that compared two novel defibrillation strategies (double sequential external defibrillation (DSED) and vector change defibrillation) to standard practice for patients in refractory ventricular fibrillation during out-of-hospital cardiac arrest. The primary outcome was survival to hospital discharge. Paramedic services were randomly assigned to provide standard defibrillation, DSED, or vector change defibrillation over 6-month periods. The trial aimed to determine if DSED or vector change defibrillation results in greater survival rates compared to standard defibrillation.