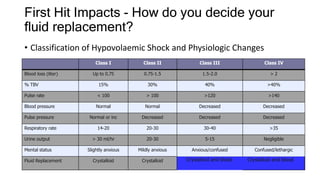
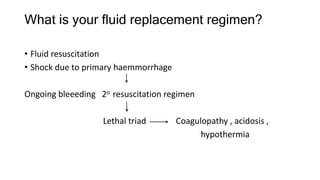
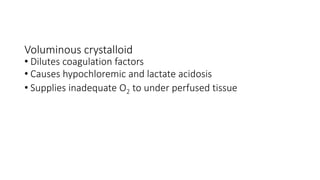
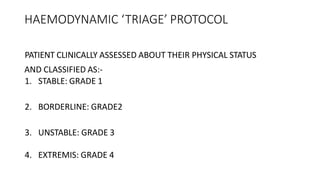
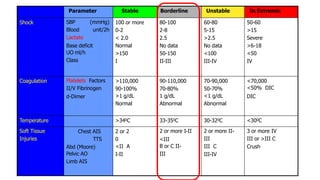
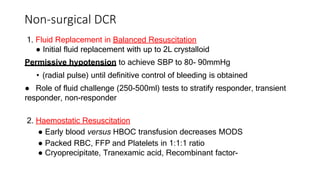
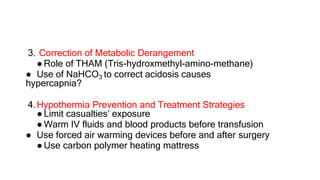
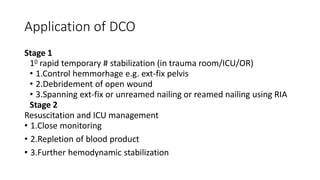
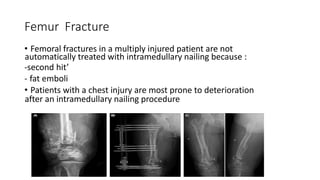
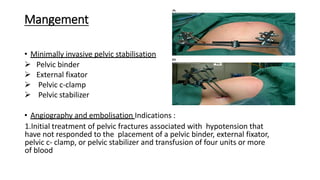
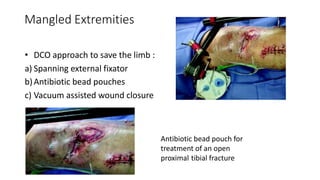
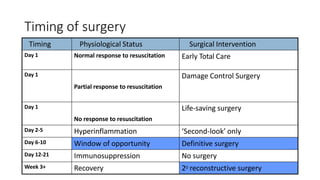
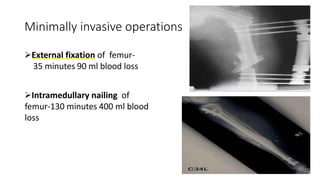
Damage control orthopaedics is an approach that temporarily stabilizes orthopaedic injuries to avoid worsening a patient's condition through a "second hit" of major surgery. It aims to arrest hemorrhage, restore blood volume, and correct coagulopathy, acidosis, and hypothermia before definitive fracture repair. Key principles include early rapid stabilization using external fixation and avoiding prolonged operative times. It is applied for polytrauma patients with multiple long bone fractures and injuries like pelvic fractures associated with hemorrhage or chest injuries, where early stabilization is safe and may be beneficial.