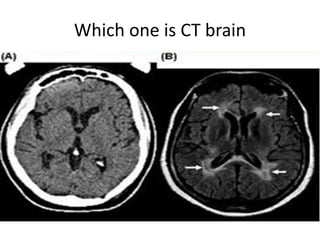
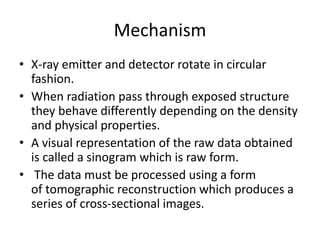
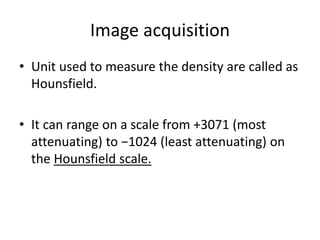
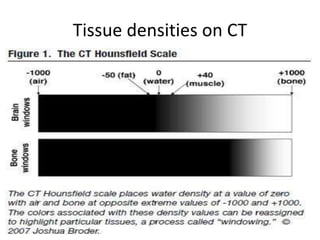
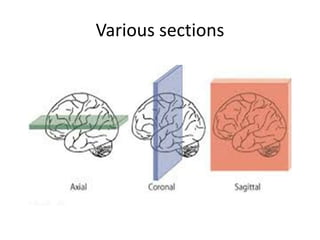
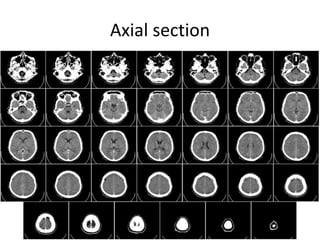
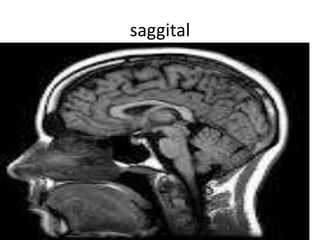
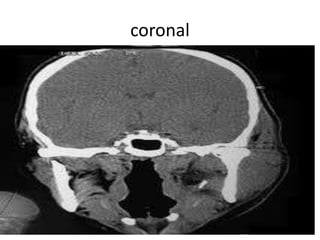
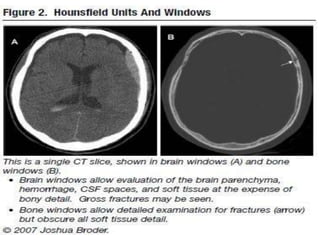
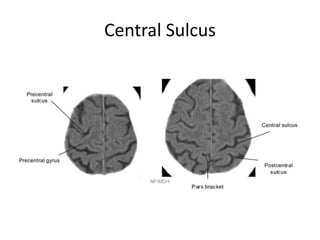
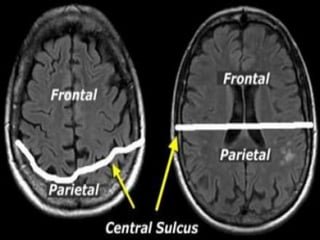
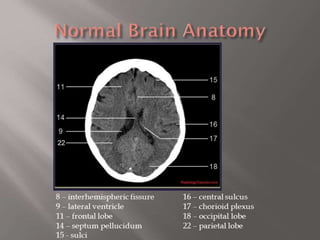
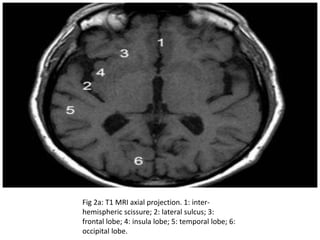
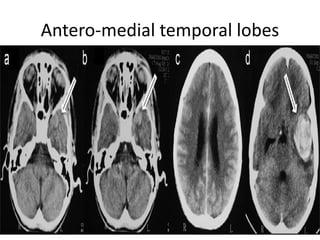
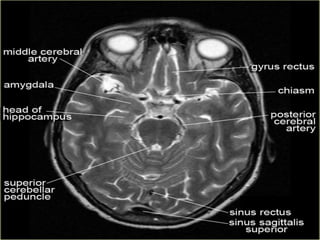
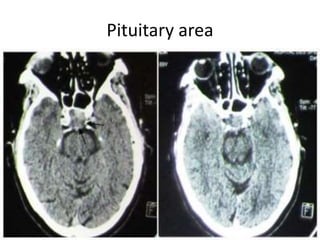
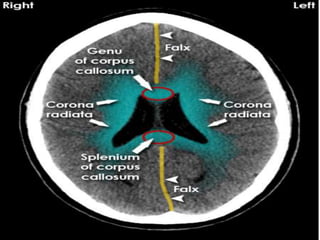
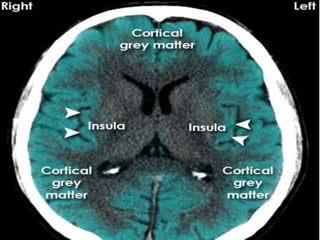
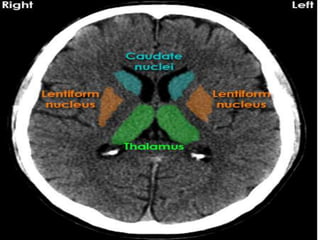
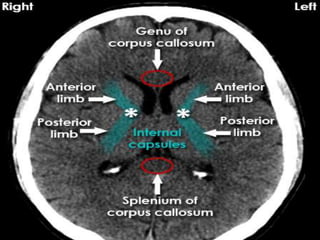
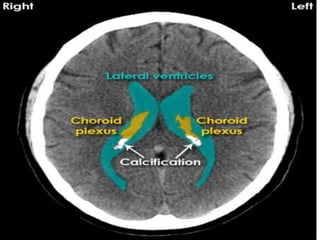
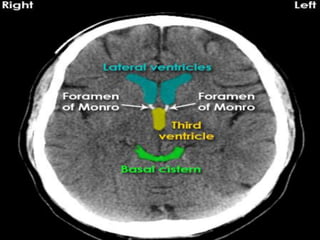
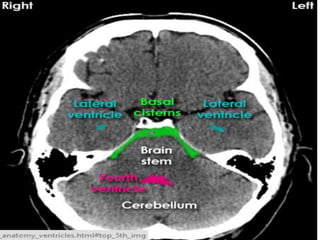
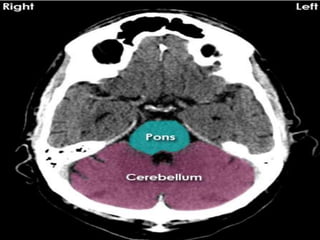
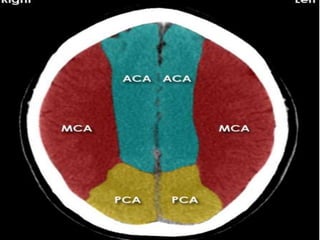
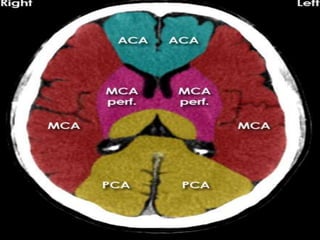
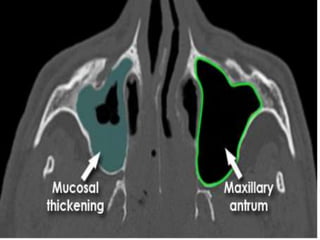
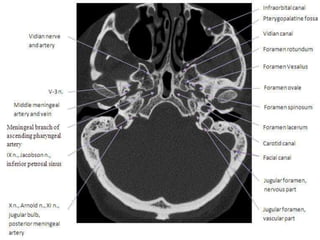
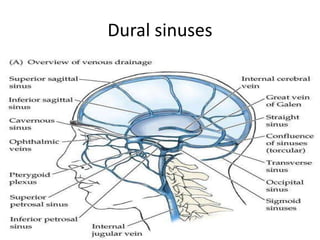
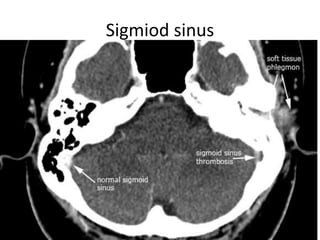
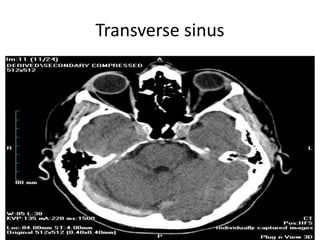
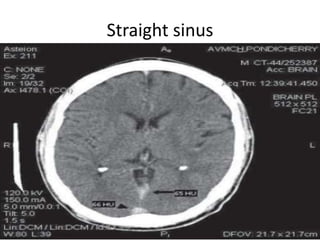
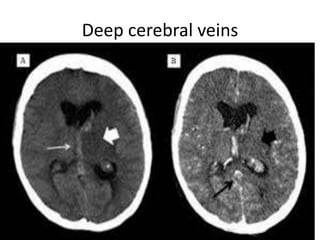
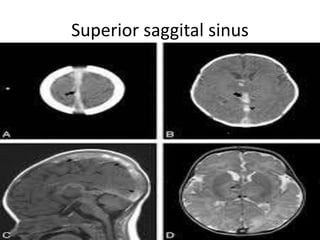
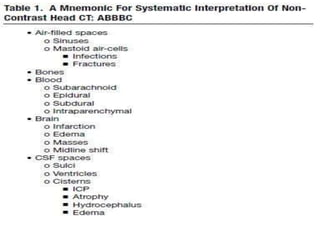
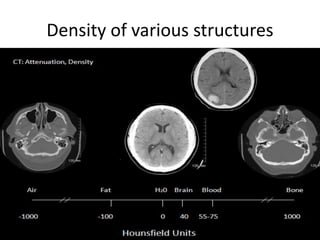
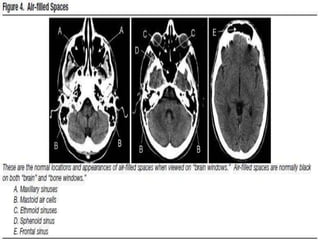
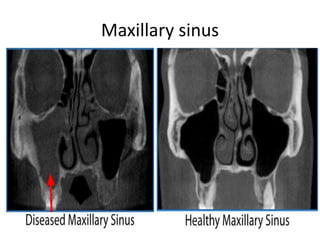
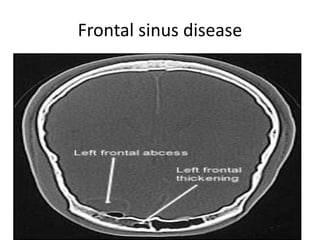
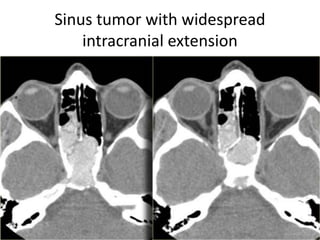
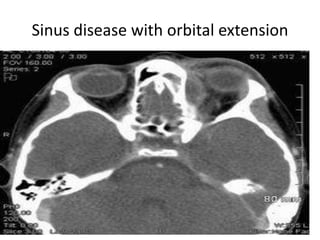
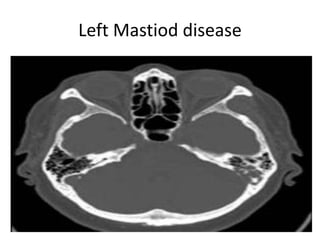
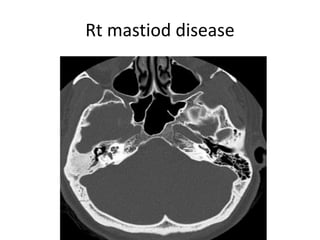
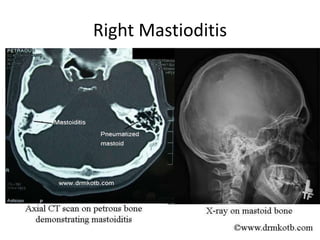
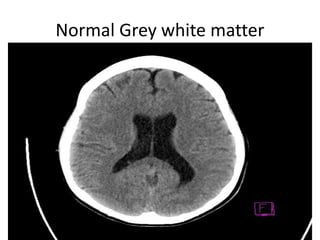
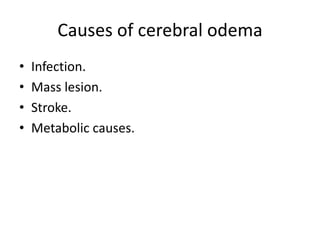
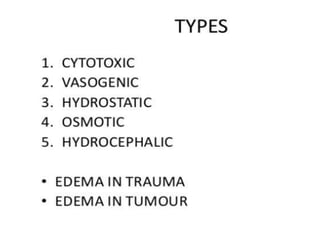
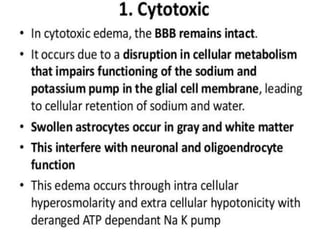
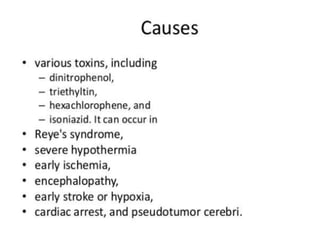
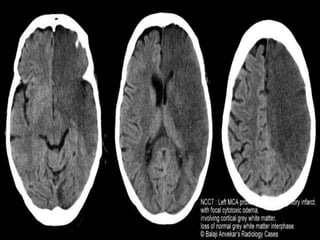
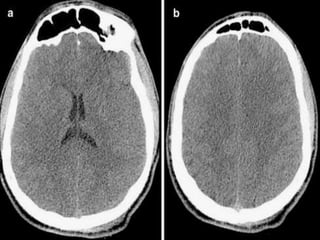
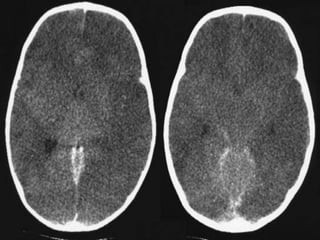
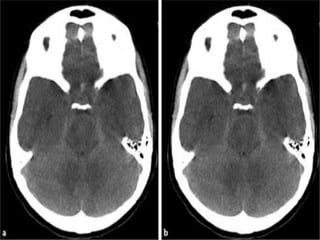
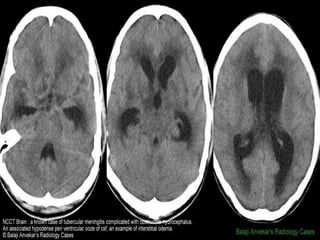
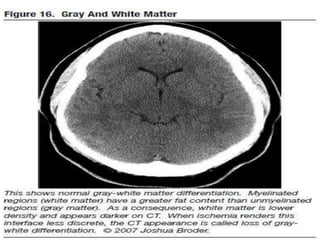
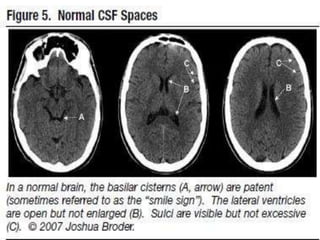
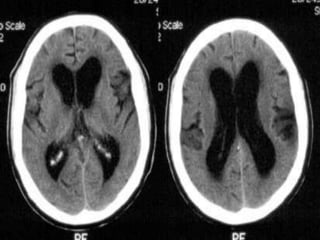
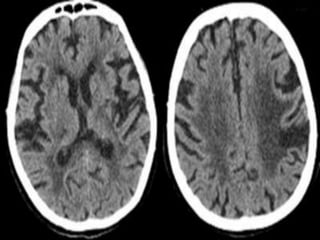
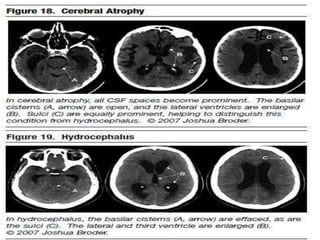
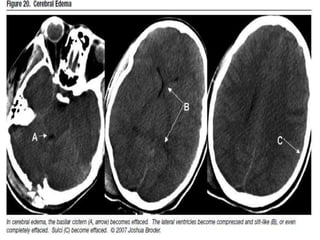
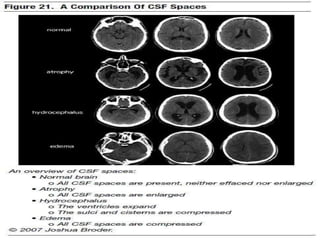
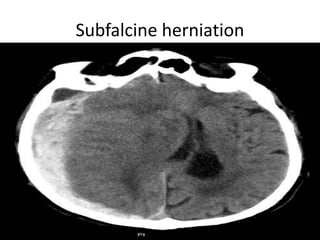
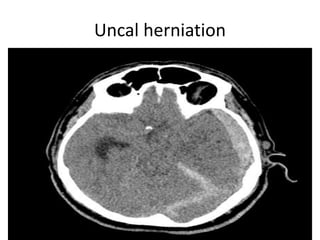
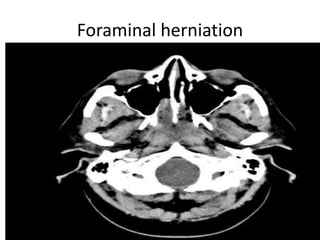
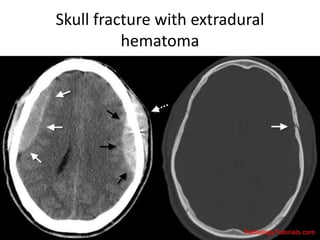
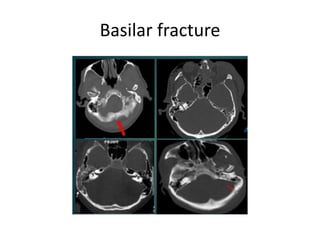
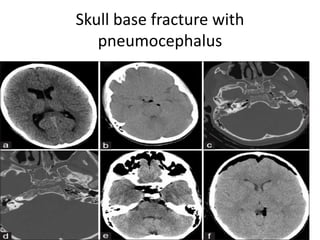
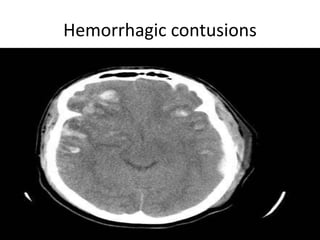
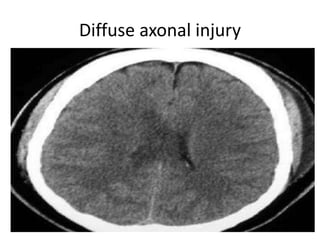
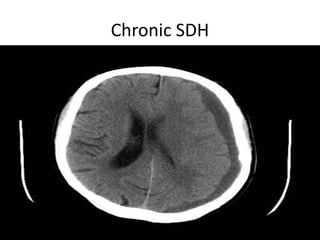
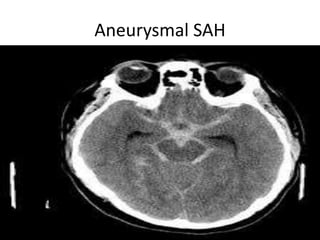
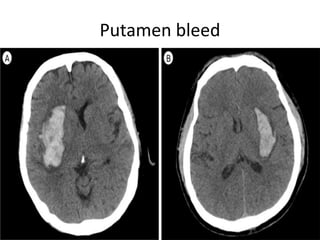
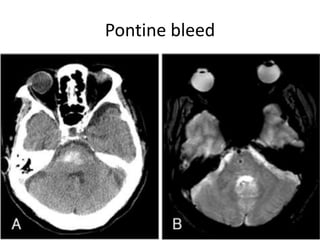
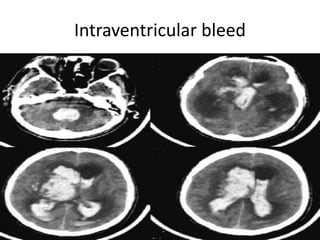
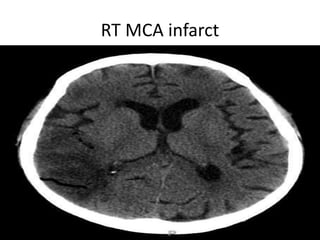
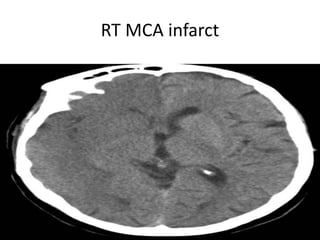
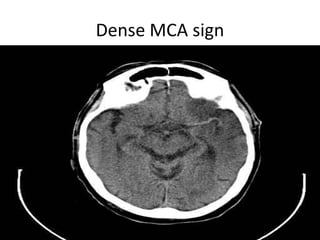
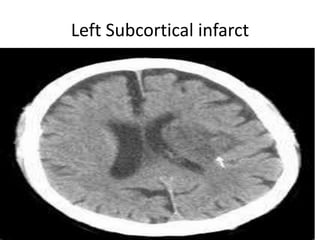
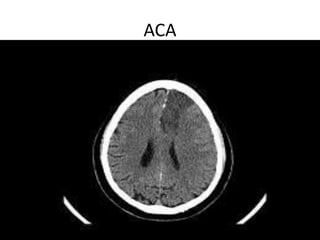
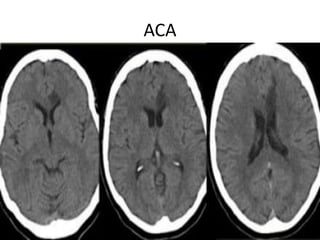
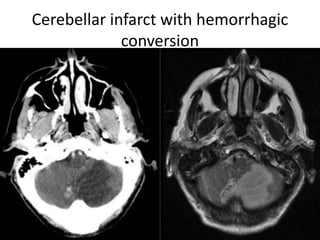
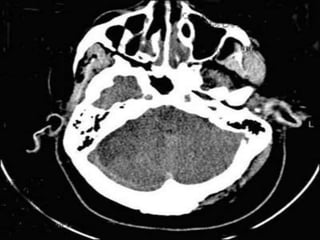
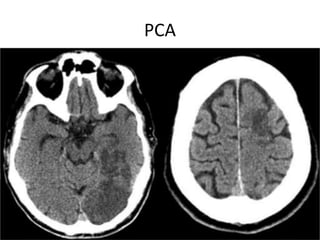
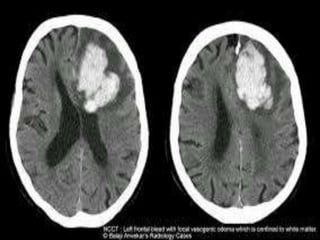
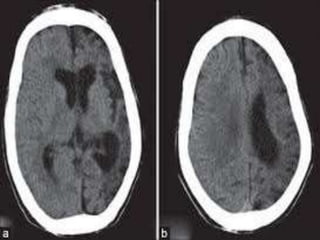
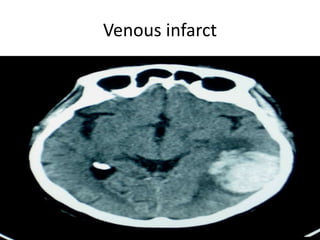
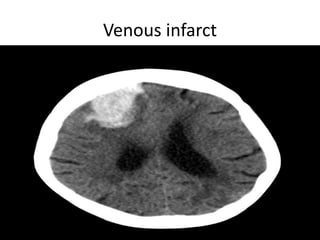
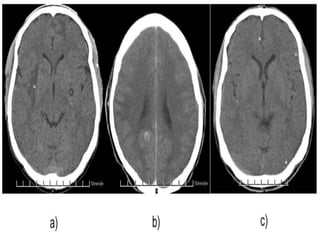
The document provides information about CT brain imaging including terminology used, differences between CT and MRI, how a CT scan works, tissue densities visualized on CT, common anatomical structures seen on brain CT, approaches to interpreting a CT brain scan, and various pathological conditions that can be identified on CT including trauma, vascular insults, infections, tumors and other disorders. Key points covered include how CT provides clear bone images while MRI better depicts soft tissue contrast, how CT reconstruction works to create cross-sectional images, and examples of some common abnormalities that manifest as hyperdense or hypodense lesions on CT scans.