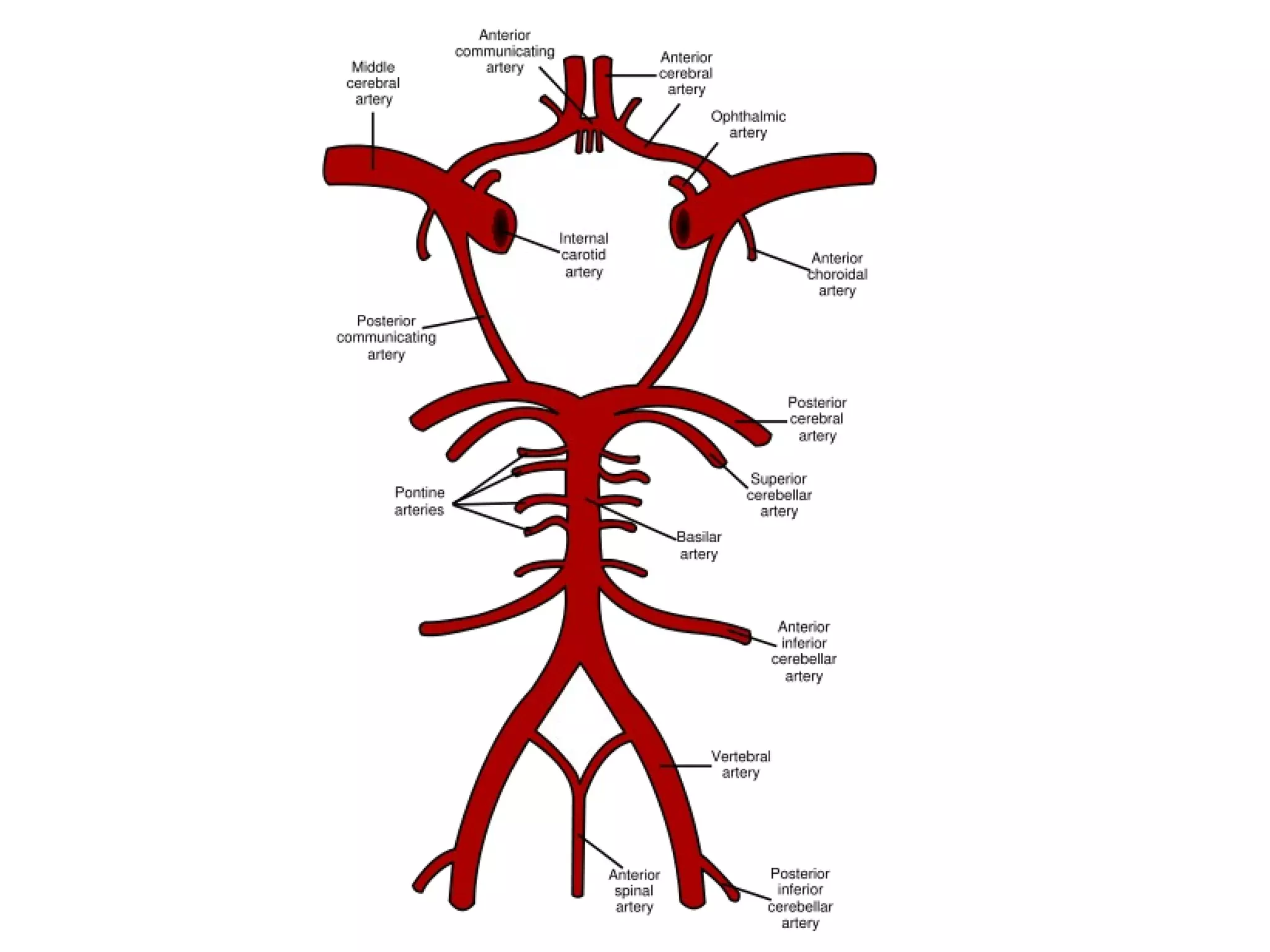
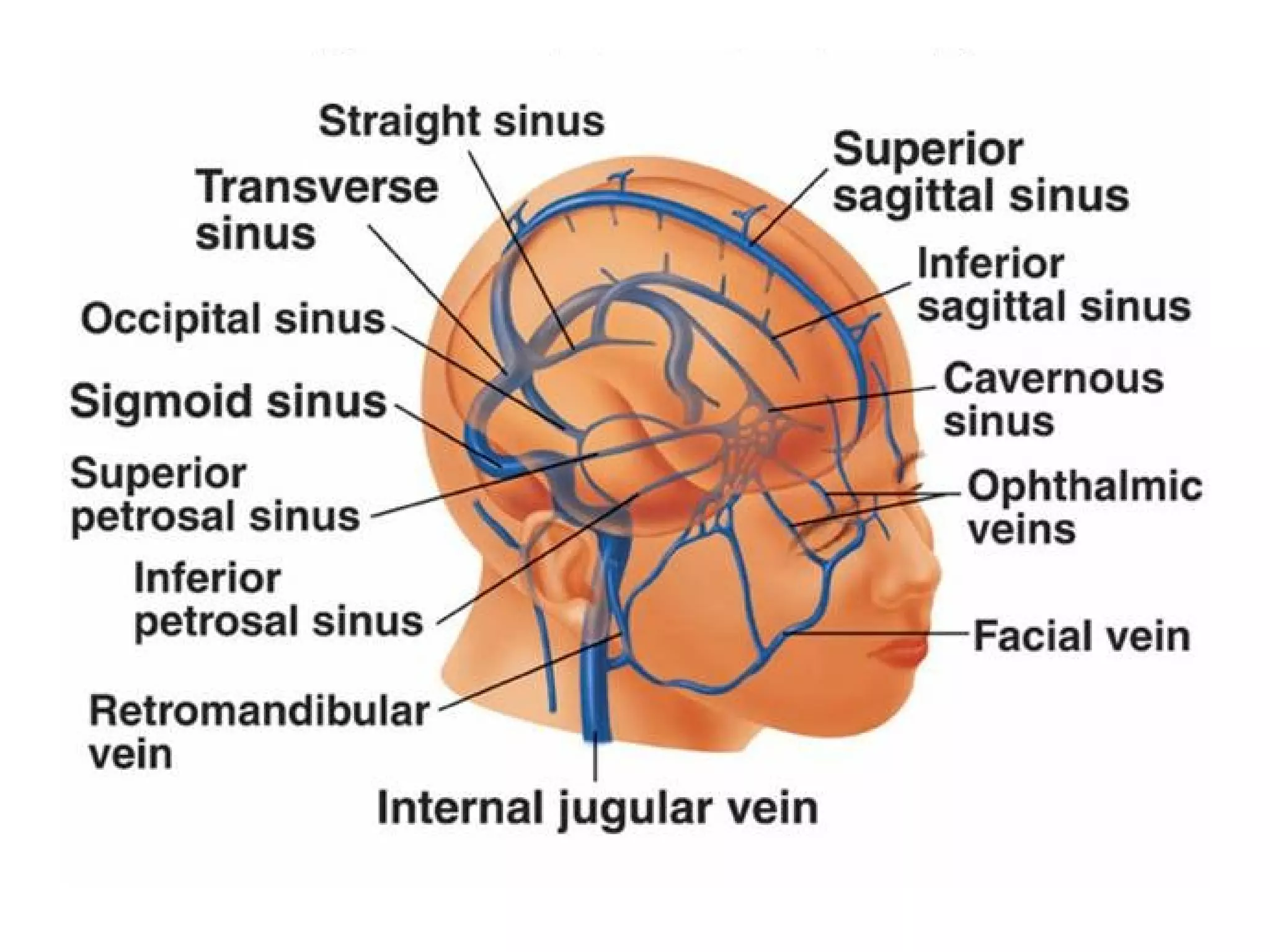
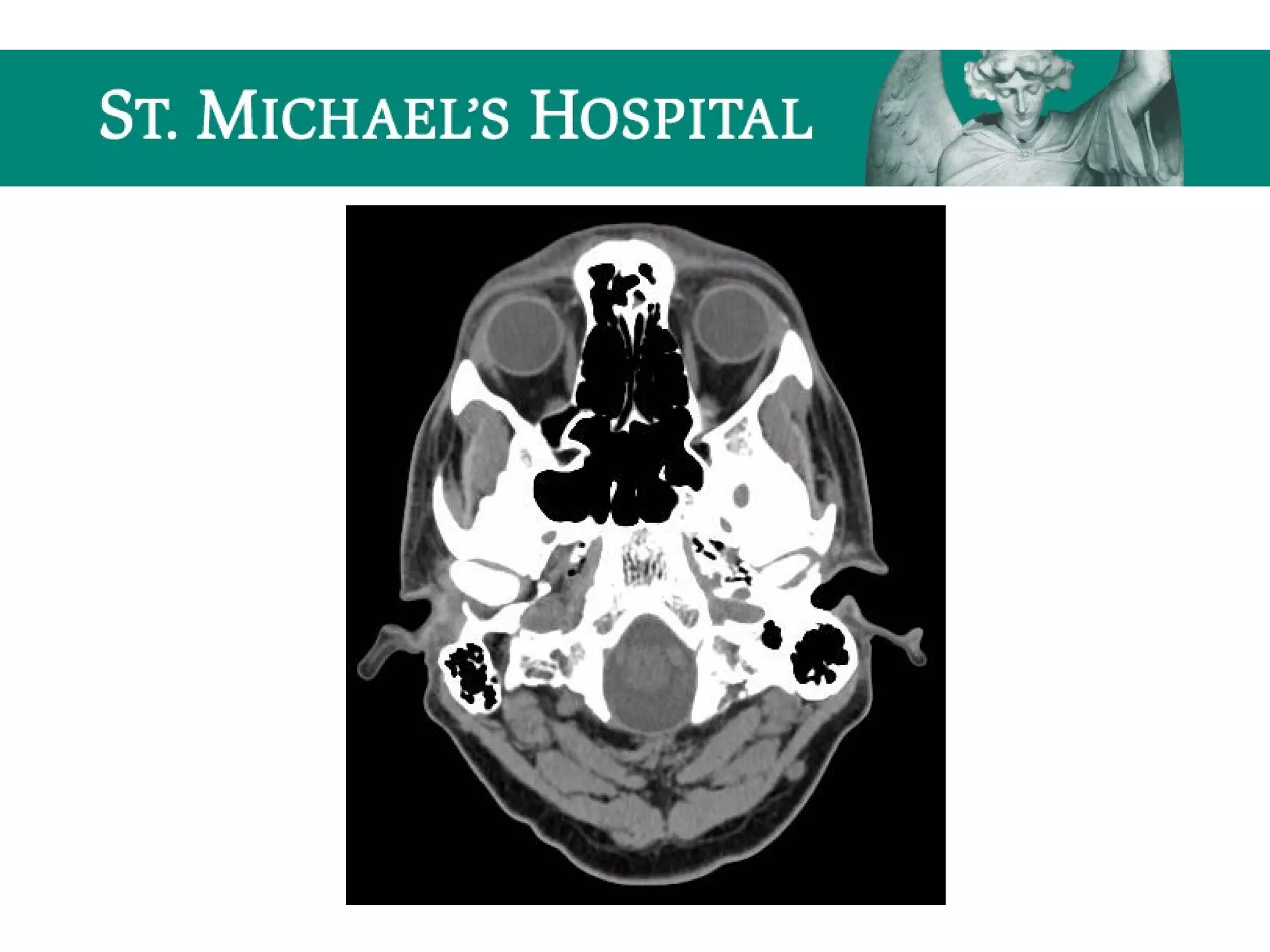
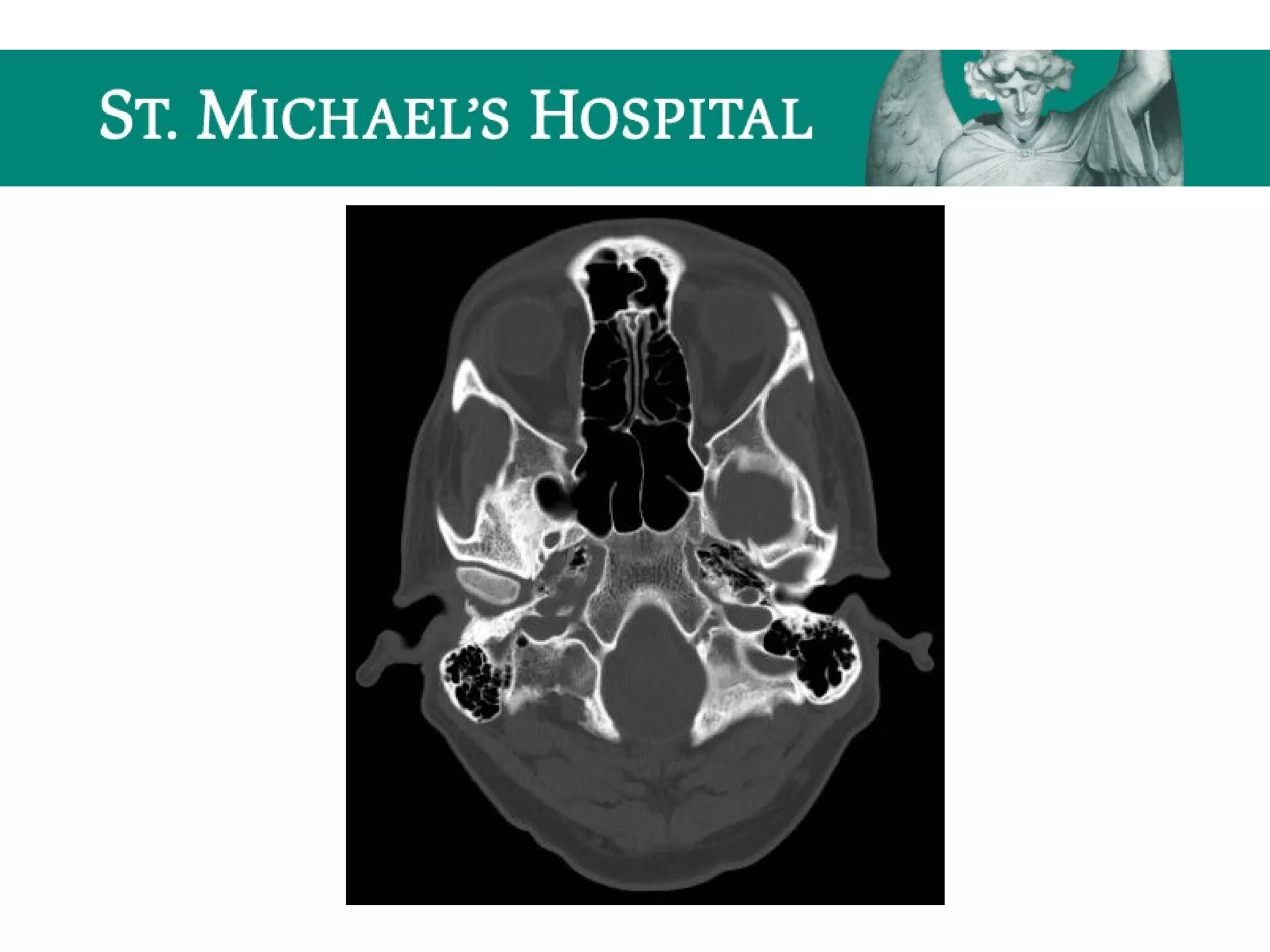
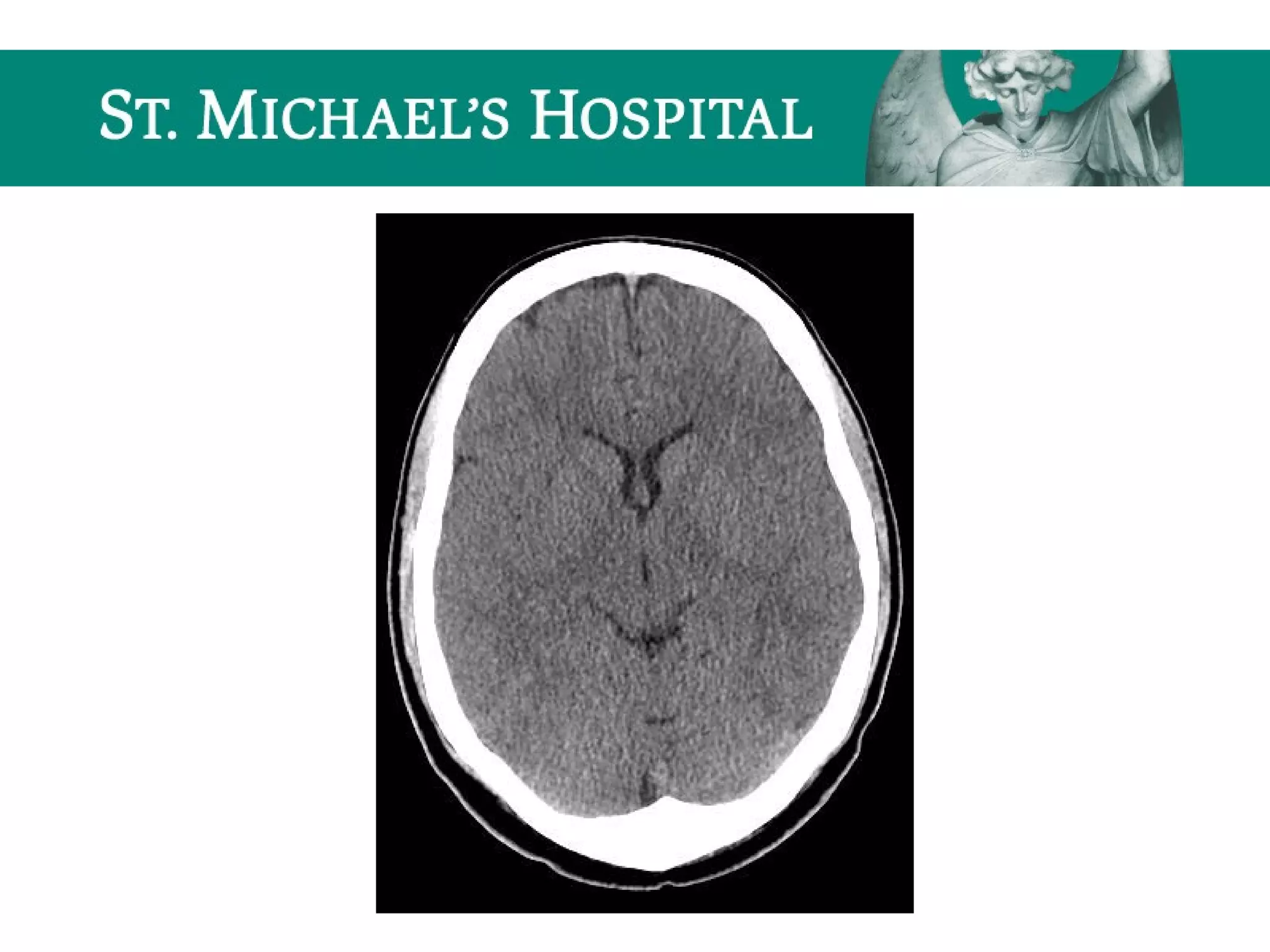
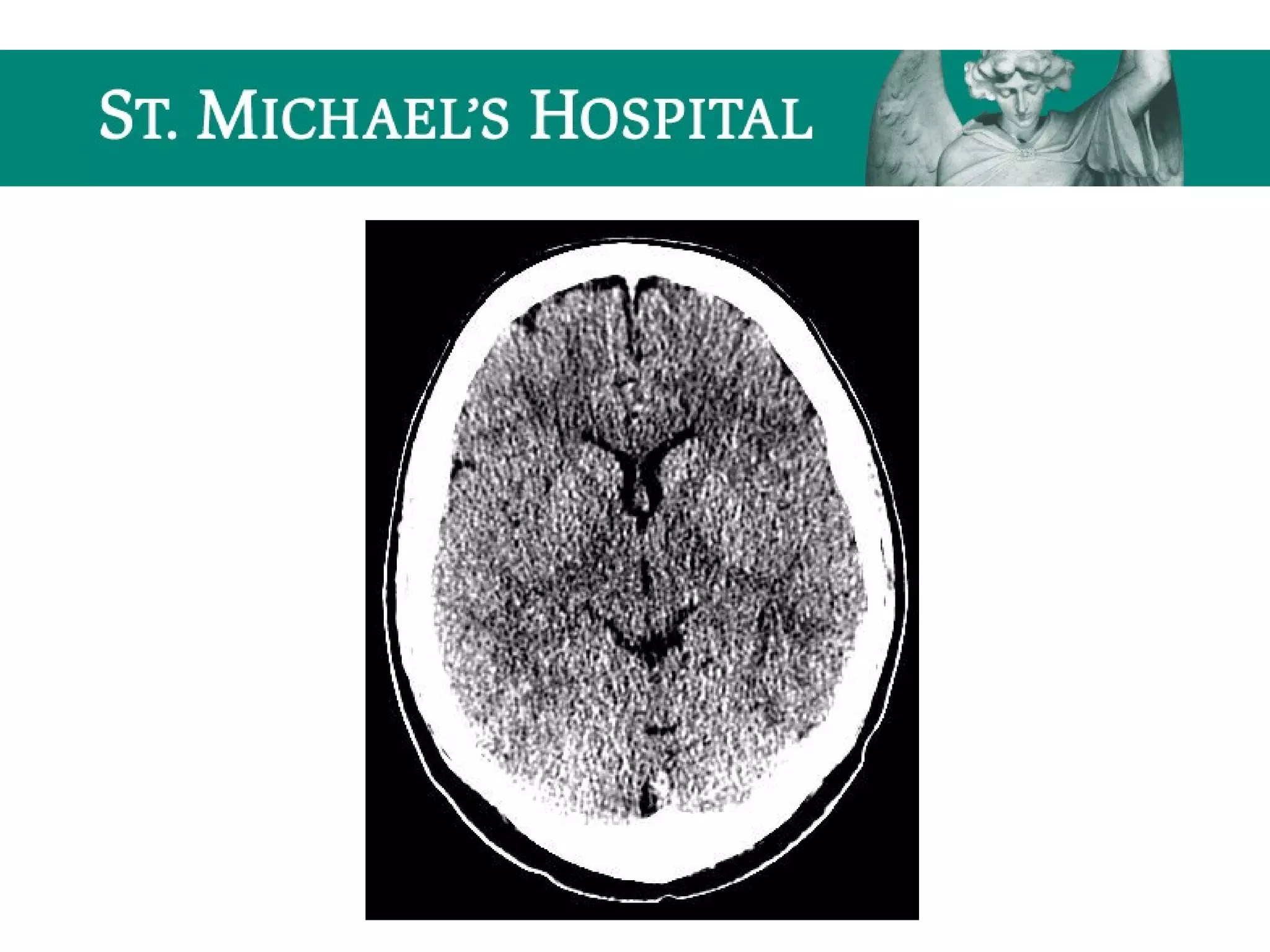
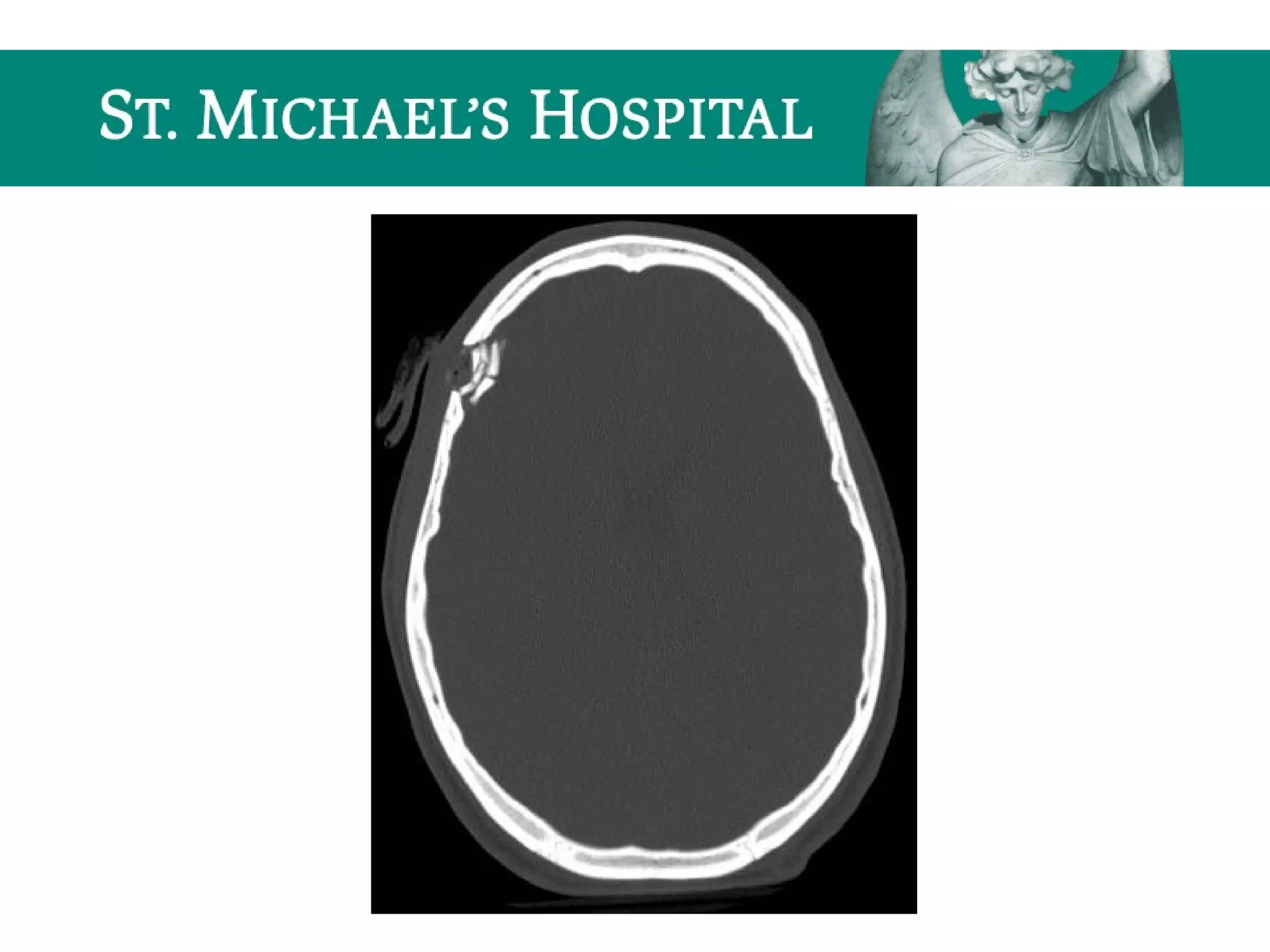
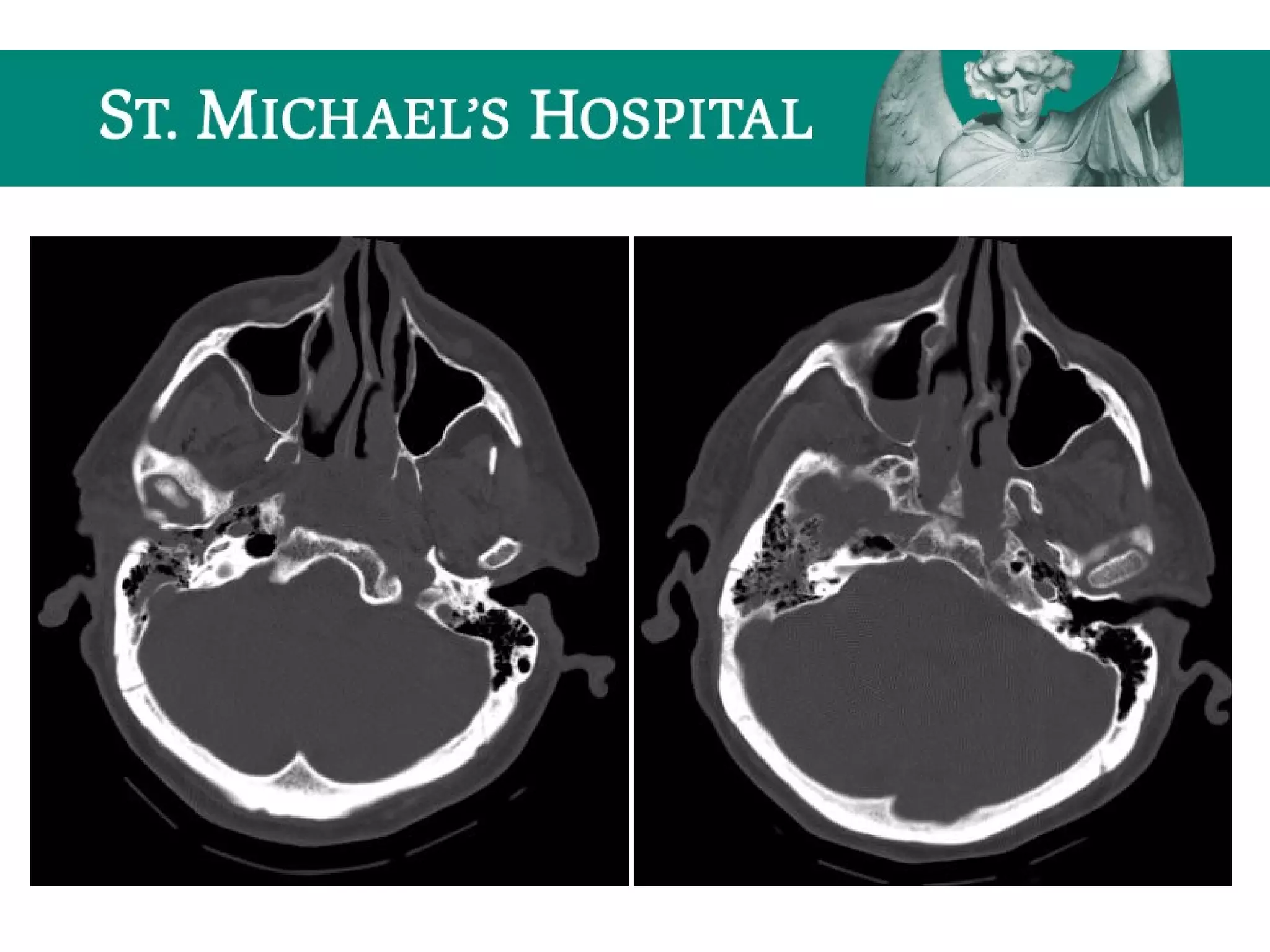
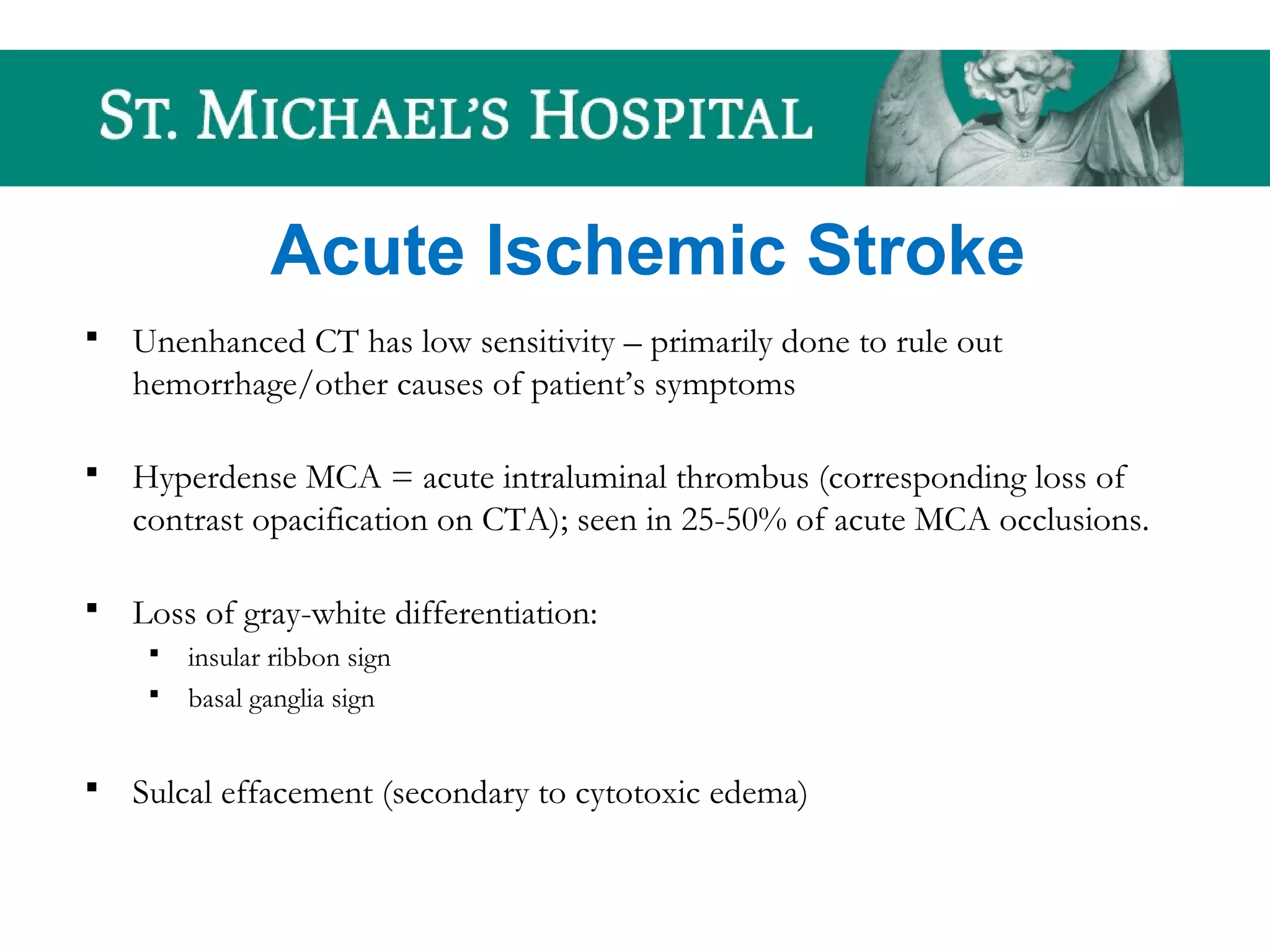
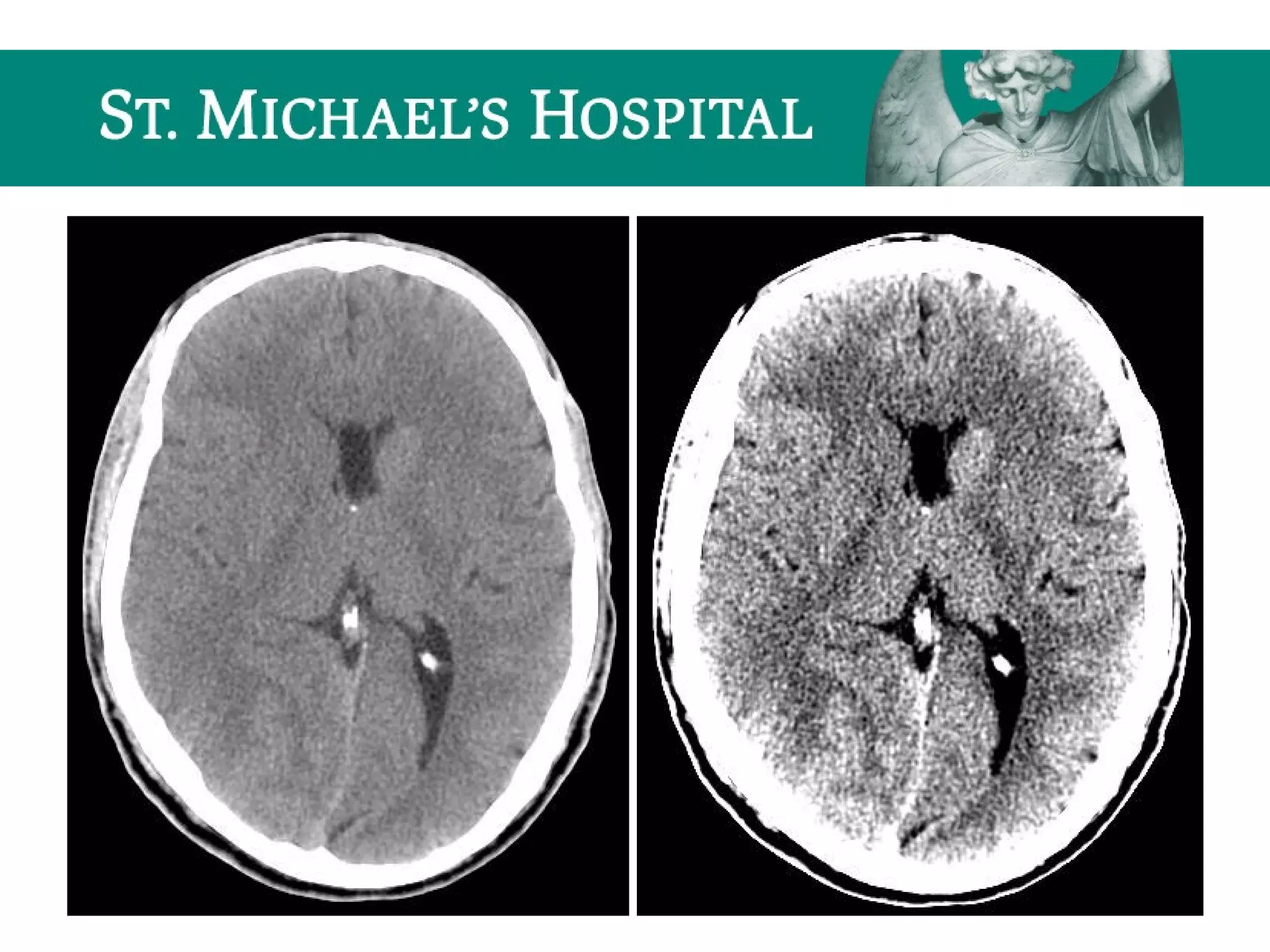
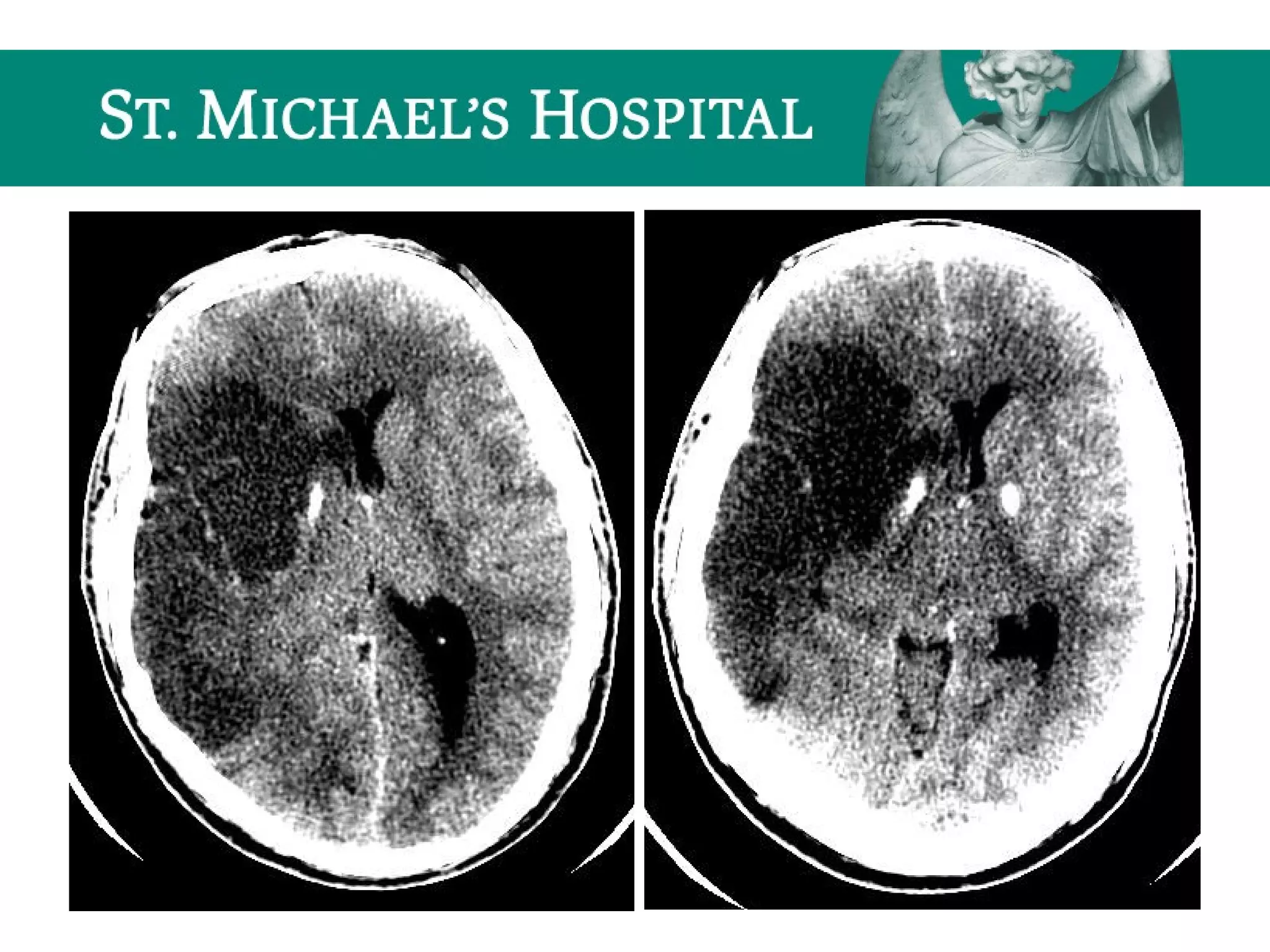
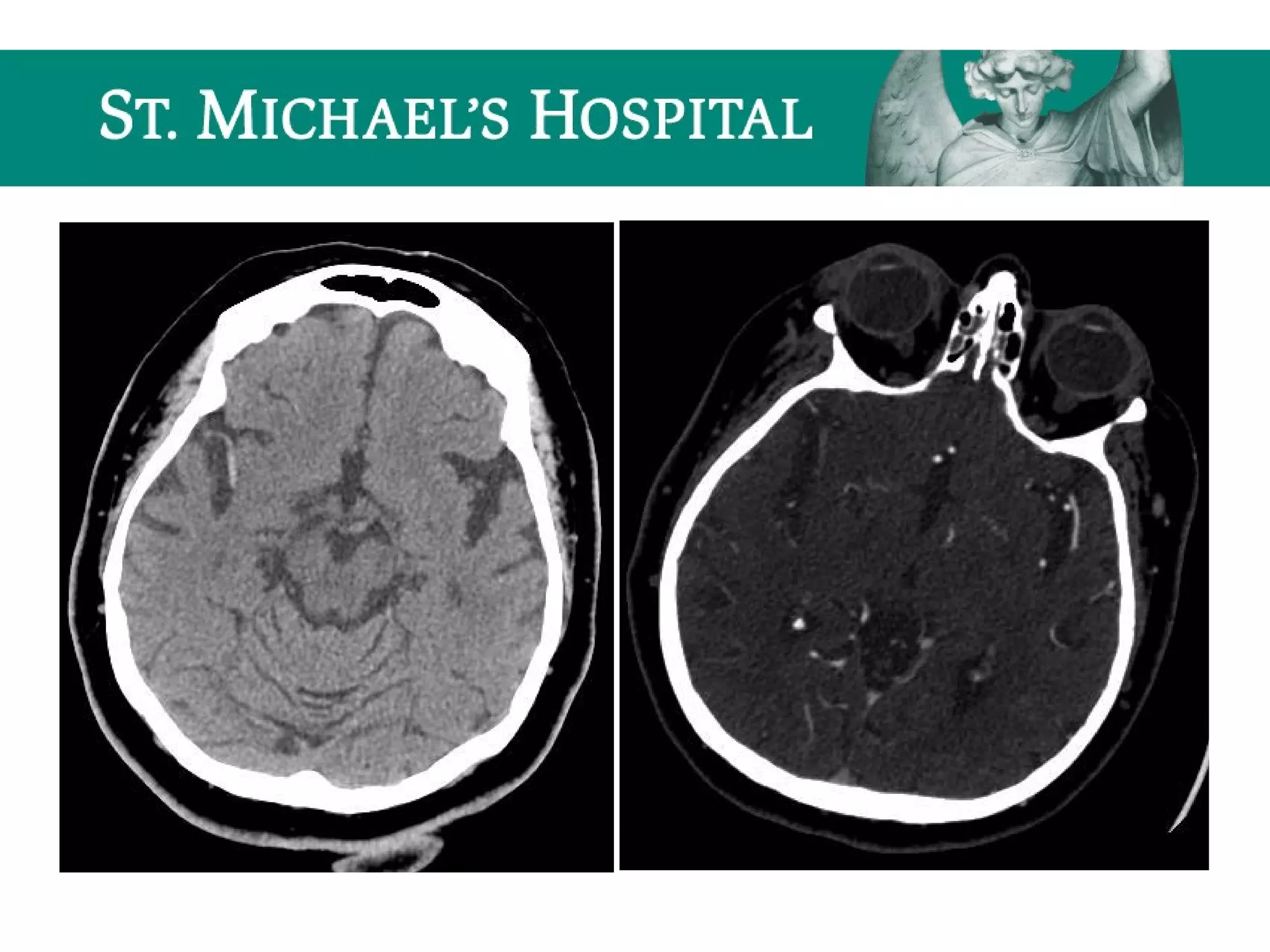
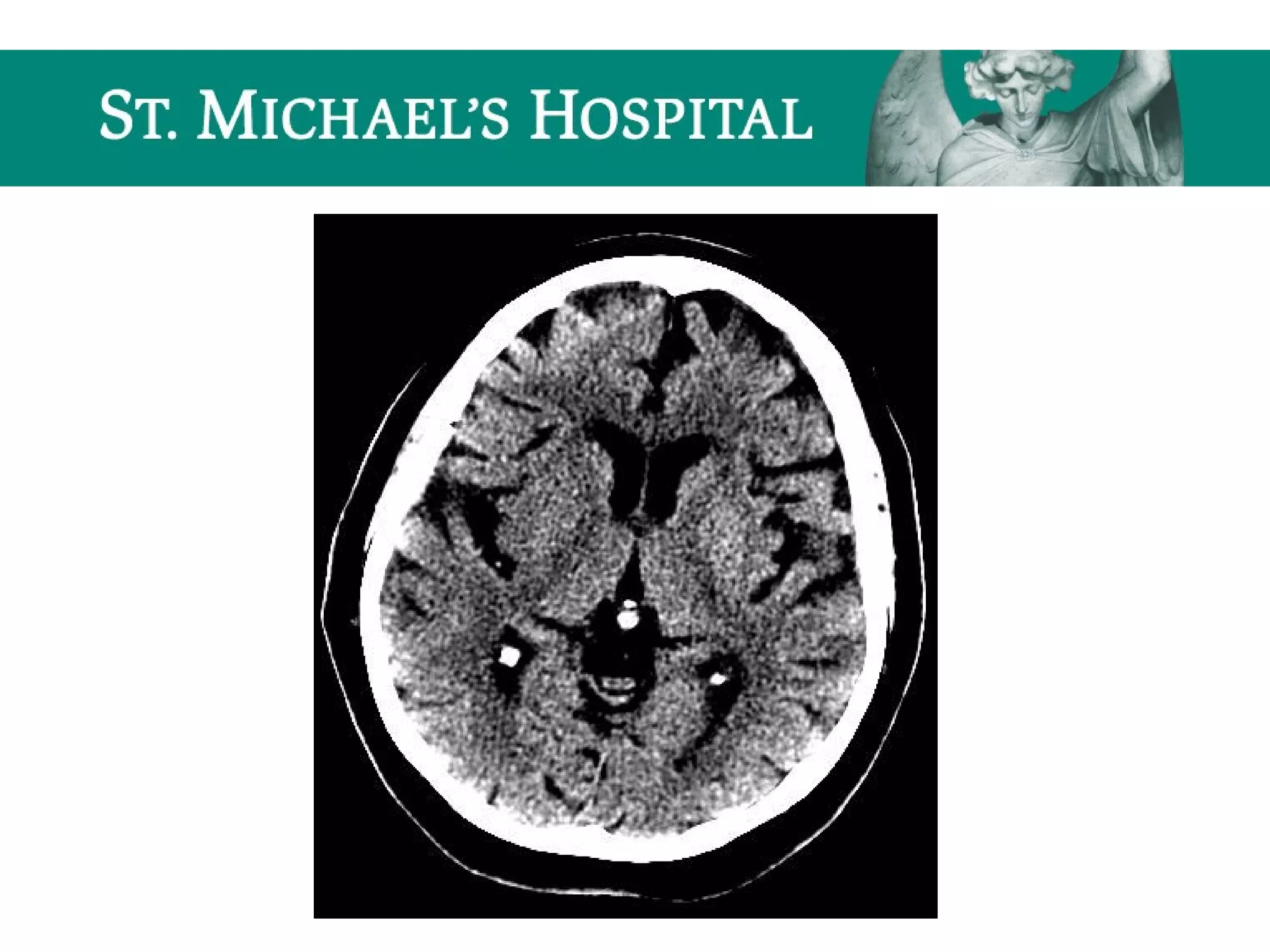
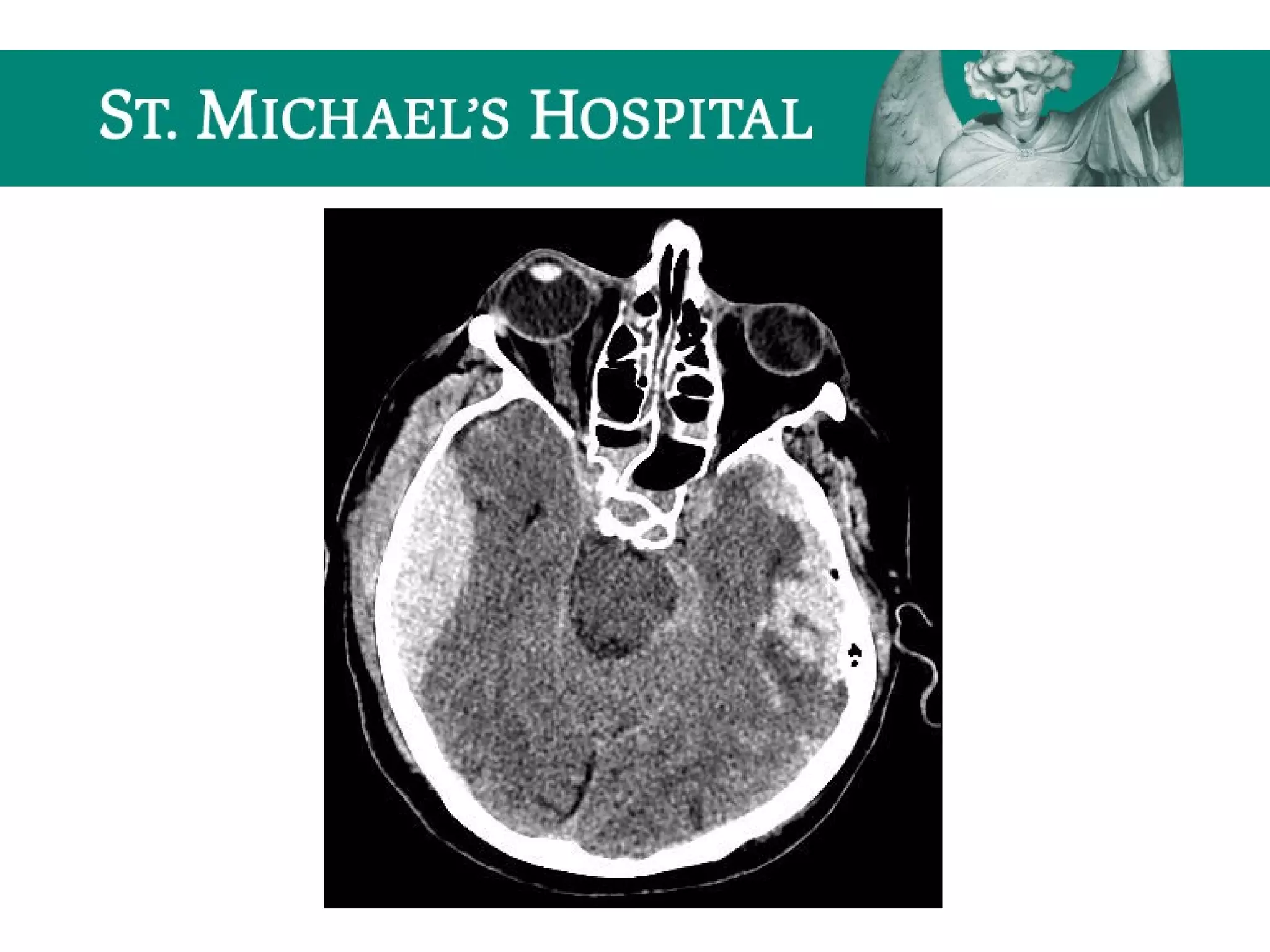
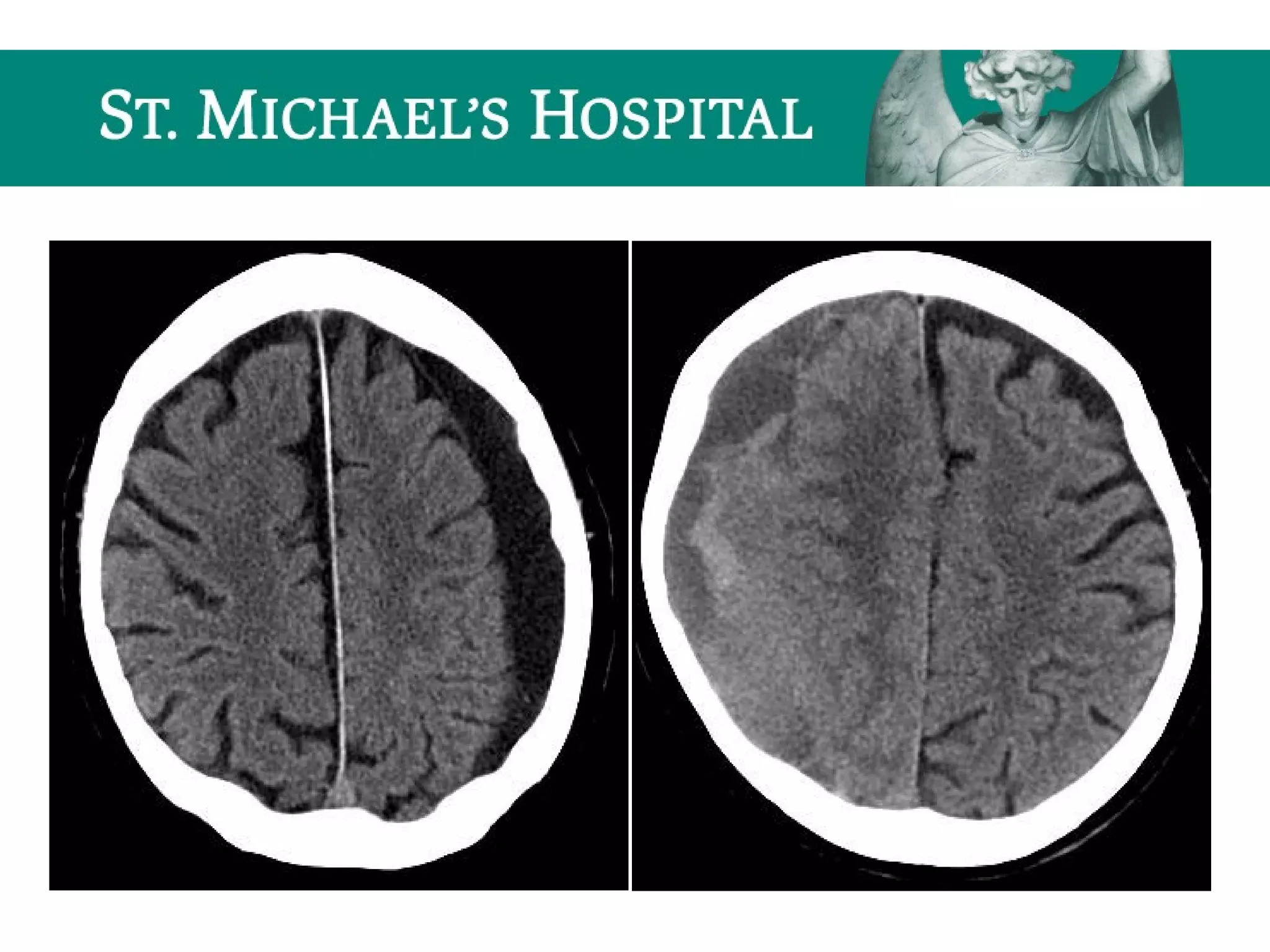
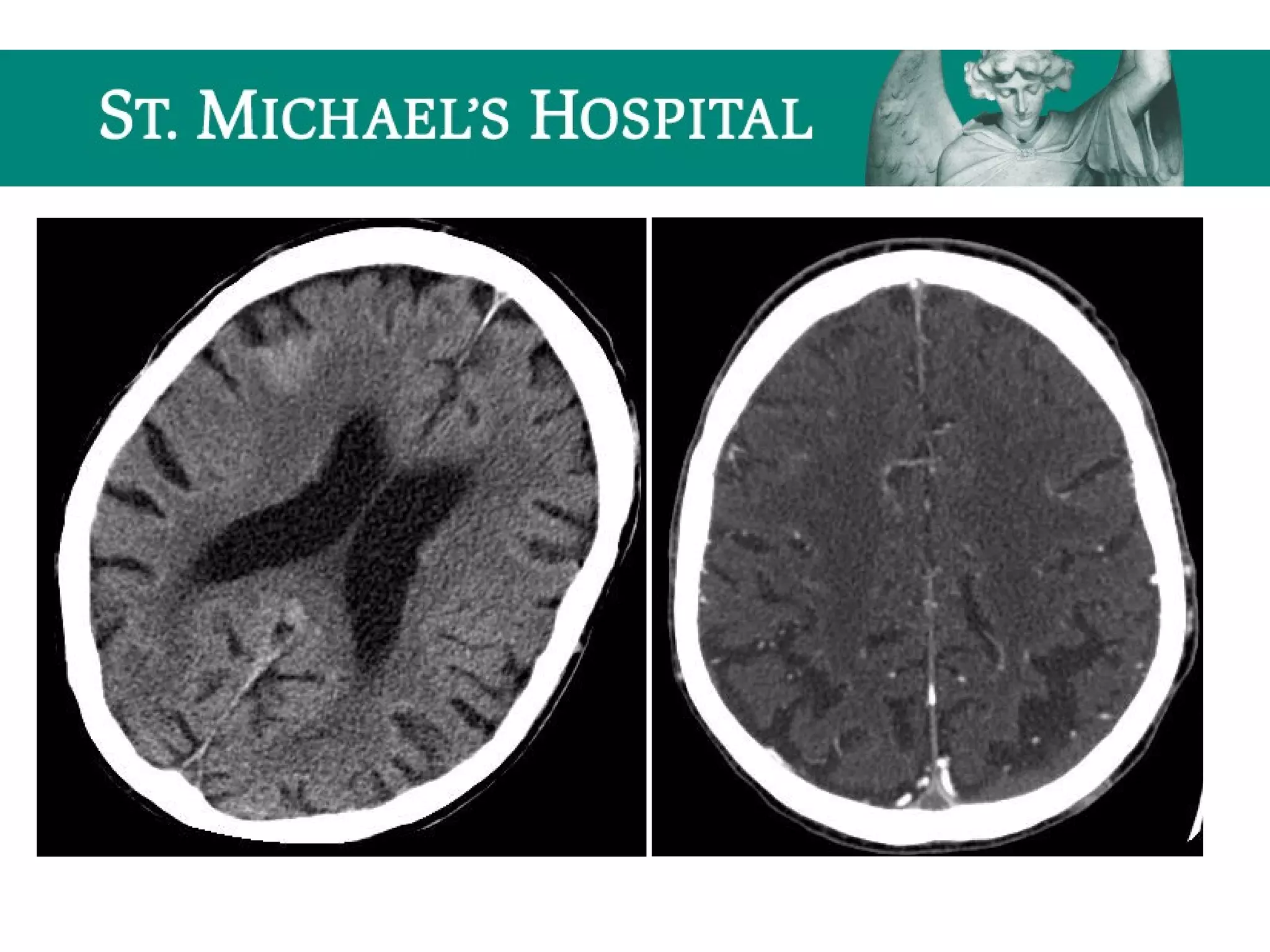
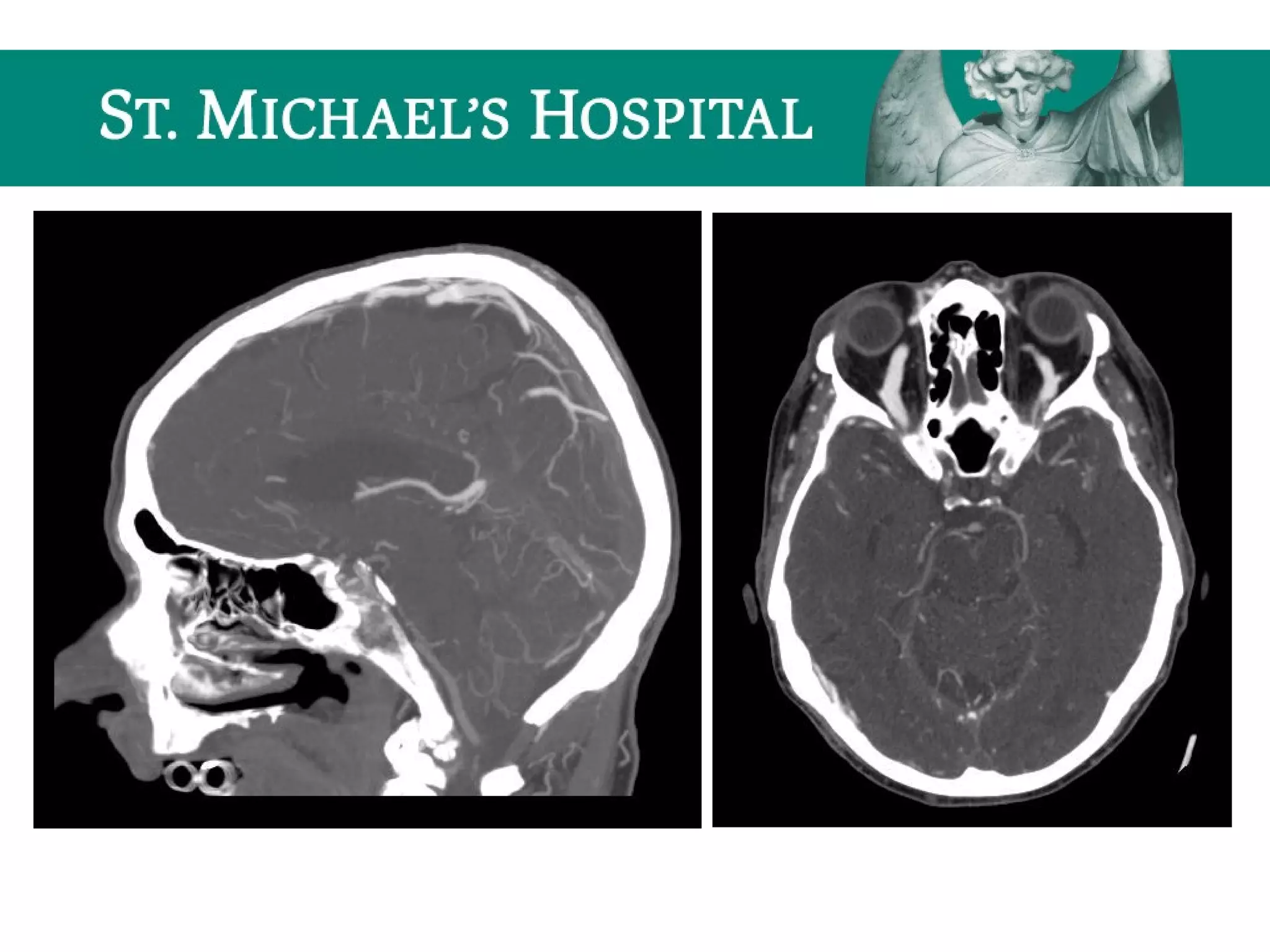
This document provides an overview of the approach to interpreting head CT scans for radiology residents on call. It reviews CT basics like windowing and normal anatomy. Important search patterns are outlined for unenhanced, enhanced, CTA and CTV studies. Common indications, findings and algorithms are discussed for acute conditions like hemorrhage, stroke and skull fractures. Key imaging features of ischemic stroke, anoxic brain injury and intracranial hemorrhage are also summarized. The document aims to equip radiology residents with the essential knowledge for accurately interpreting and reporting emergent head CT scans.