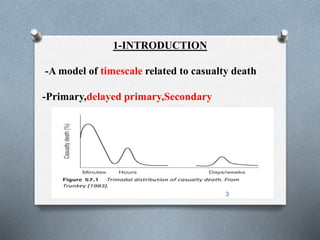
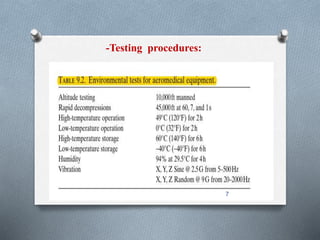
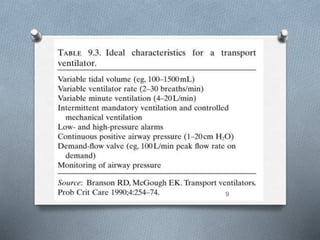
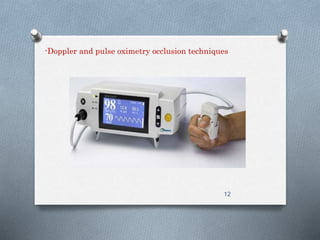
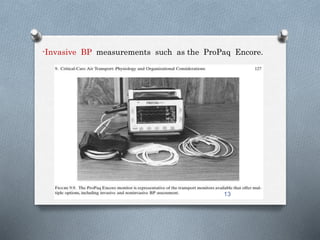
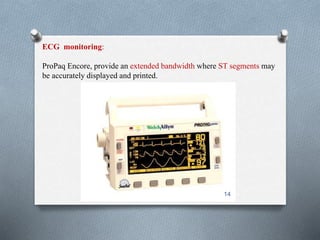
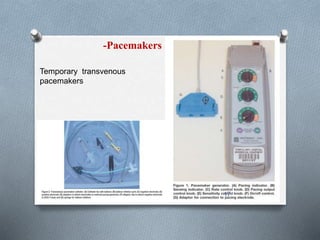
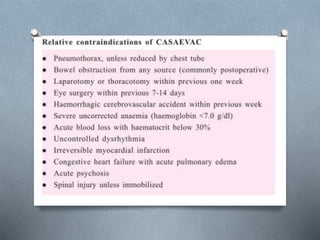
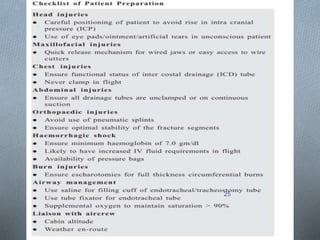
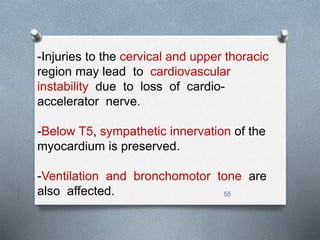
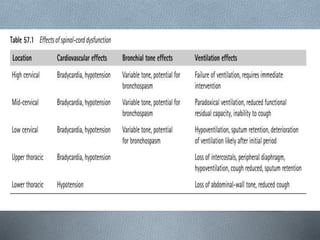
This document discusses the aeromedical transfer of critically ill patients. It covers the composition of the transfer team, necessary equipment including ventilators, monitors, pumps and analysis tools. It then discusses potential issues during flight like changes in altitude, and special considerations for patients with trauma, surgery, or neurological, respiratory or circulatory conditions. The checklist, therapeutic regimens and staffing for transfers are also outlined.