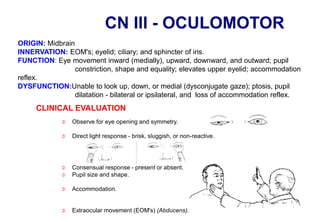
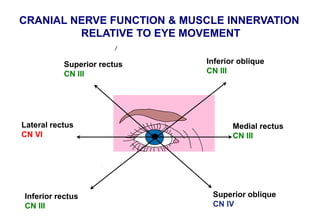
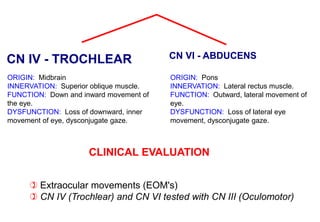
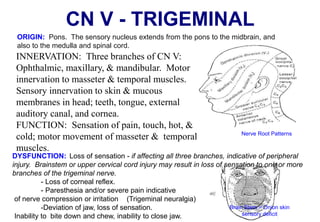
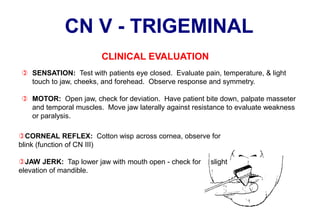
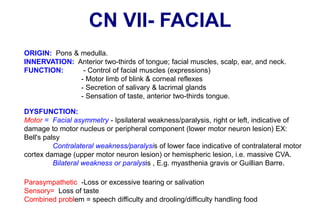
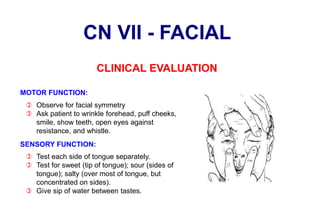
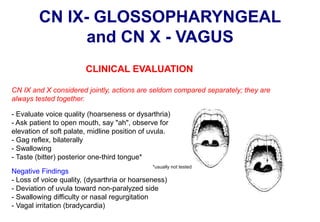
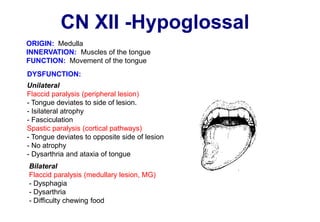
The document outlines the 12 pairs of cranial nerves, detailing their origin, innervation, functions, and clinical evaluations to identify dysfunctions. Each nerve is associated with sensory, motor, or mixed functions, with specific tests recommended for assessing various conditions, such as visual loss, facial asymmetry, or hearing issues. Key nerves discussed include the olfactory, optic, oculomotor, trigeminal, facial, acoustic, glossopharyngeal, vagus, accessory, and hypoglossal nerves.