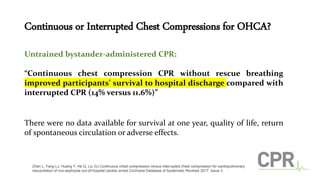
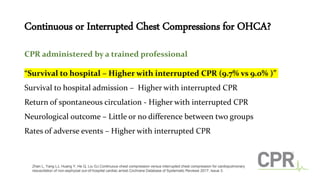
1. A Cochrane review found that for untrained bystanders, continuous chest compressions without rescue breathing improved survival to hospital discharge compared to interrupted CPR. For trained professionals, interrupted CPR had slightly better outcomes.
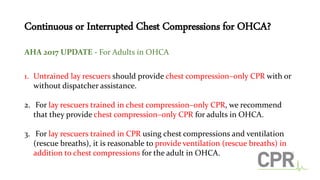
2. The AHA recommends that untrained lay rescuers provide continuous chest compressions with or without dispatcher assistance for adults in cardiac arrest. For trained lay rescuers, compression-only CPR is recommended.
3. A study found no difference in outcomes between continuous compressions with asynchronous ventilations and 30:2 CPR. 30:2 CPR was associated with better outcomes than 15:2 CPR. It may be reasonable for EMS to use 10 breaths per