This document discusses the definition and treatment of locally advanced rectal cancers. Key points include:
- Locally advanced rectal cancers are defined as T4 or node-positive lesions that cannot be fully resected without a high risk of residual disease.
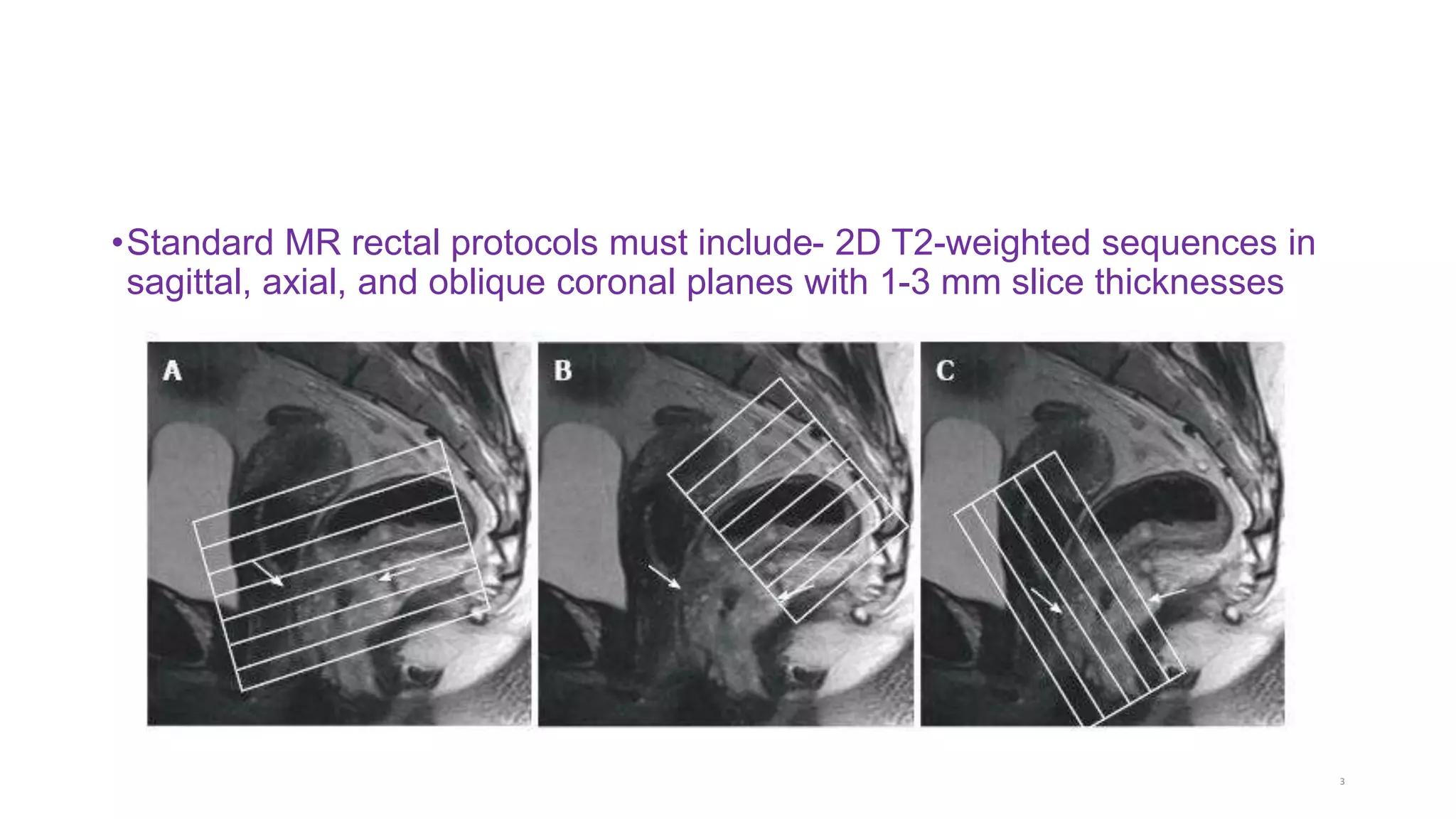
- Standard MR protocols for rectal imaging include T2-weighted sequences in sagittal, axial, and oblique planes with 1-3mm slice thicknesses.
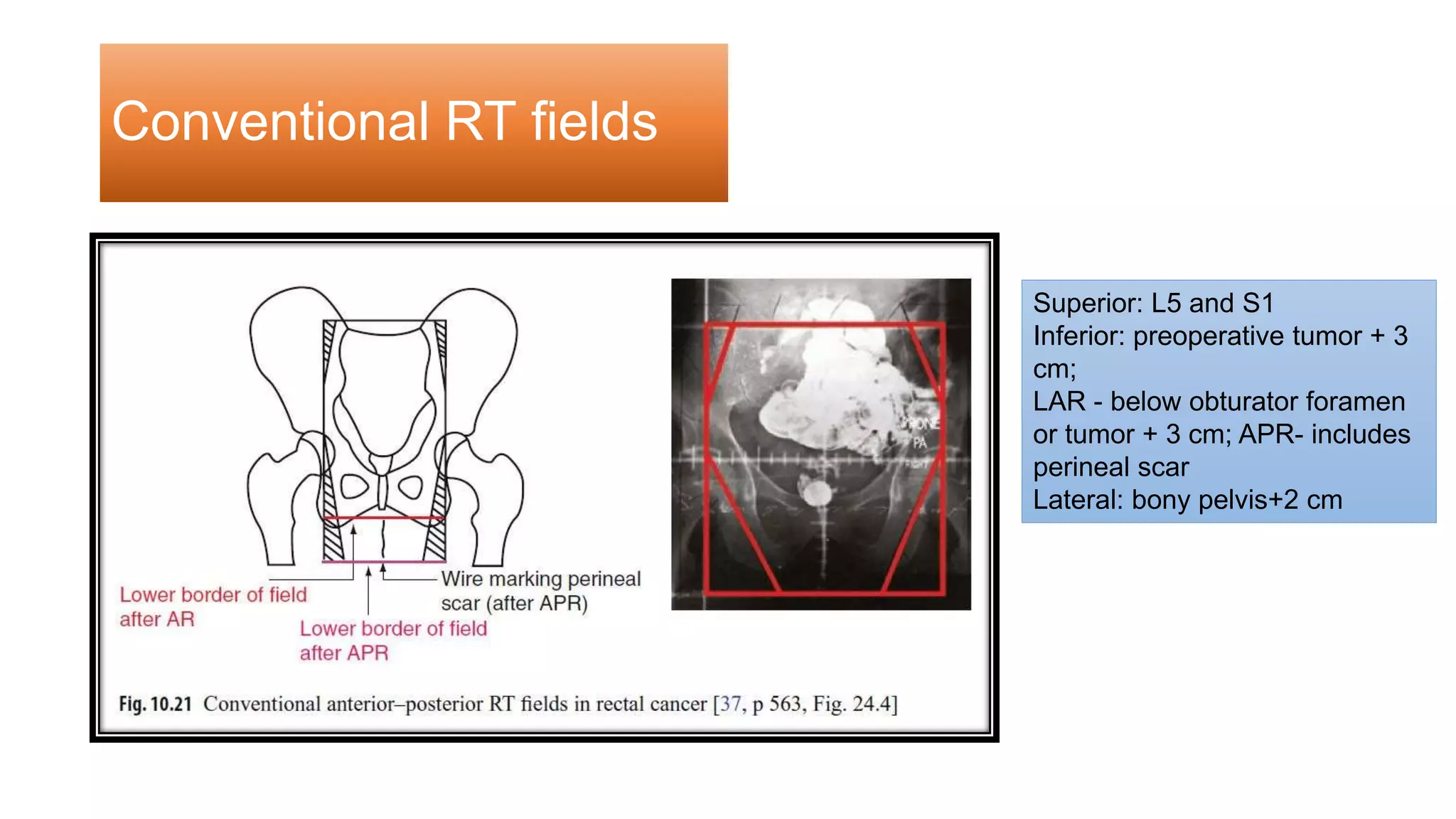
- Treatment recommendations include pre-operative chemoradiotherapy or short-course radiotherapy followed by surgery and adjuvant chemotherapy.
- Total mesorectal excision is the standard surgical procedure to completely remove the rectal tumor and lymph nodes.



















![•Local recurrence rate for T3-4 or N1 rectal cancer is -25%.
•Total mesorectal excision [tme], 10year lr 11% [dutch tme study]).
•TME got its wide spread attention after herald’s articled a new approach to rectal cancer.
•(Heald rj, br j hosp med. 1979 sep; 22(3)277-81.)
•Goal of this surgery-
• 1. En bloc resection of the rectal cancer with a complete pararectal lymph
node dissection as contained in the mesorectum.
• 2. Any additional lymphadenopathy may also be dealt with depending on
the stage of the tumor.
•To reach this goal, the lateral dissection of the rectum must not breech
the fascia propria of the rectum, which stays outside the mesorectum.](https://image.slidesharecdn.com/larec-230203161428-efa6aa67/75/LA-Rec-pptx-21-2048.jpg)